Summary
Background/Objective
This study aimed to assess the available evidence on the survival of distal cholangiocarcinoma (DCC) patients following resection with curative intent and analyze the prognostic factors.
Methods
Relevant studies published between January 2000 and January 2015 were identified by searching PubMed and Embase and reviewed systematically. Summary relative risks (RR) and 95% confidence intervals (95% CI) were estimated using random-effects models.
Results
A total of 39 observational studies involving 3258 patients were included in the review. R0 resection was achieved in 84% (range, 46–100%) of patients. The median 5-year overall survival rate after resection was 37% (range, 13–54%), with corresponding rate of 44% (range, 27–63%) in R0 resection. The meta-analysis for 25 studies showed that R1 resection (RR 2.36, 95% CI 1.89–2.93), lymph node metastasis (RR 2.35, 95% CI 1.89–2.93), perineural invasion (RR 1.96, 95% CI 1.64–2.34), lymphatic invasion (RR 1.84, 95% CI 1.47–2.31), vascular invasion (RR 1.99, 95% CI 1.40–2.82), pancreatic invasion (RR 2.13, 95% CI 1.39–3.27), and pathological tumor stage ≥ T3 (RR 1.56, 95% CI 1.25–1.93) were associated with shorter survival.
Conclusion
In general, prognosis of DCC after resection is poor. R0 resection results in a substantially improved survival and represents one of the most important prognostic variables.
Keywords
distal cholangiocarcinoma;prognostic factors;resection;survival
1. Introduction
Distal cholangiocarcinoma (DCC) is defined as tumor arising in the common bile duct below the confluence of the cystic duct and above the ampulla of Vater and constitutes ∼20–40% of all diagnosed cholangiocarcinomas.1 Surgical resection offers patients the only chance for cure and long-term survival. In addition, due to its rarity, data on DCC are often combined with either periampullary cancer or perihilar cholangiocarcinoma.2 ; 3 Thus, the real benefit of surgical resection for DCC patients remains to be clarified. In this context, the present systematic review was undertaken to evaluate the available evidence on the survival of DCC patients following resection with curative intent and analyze the prognostic factors.
2. Methods
2.1. Systematic search strategy
A literature search was conducted using PubMed and Embase databases to identify all relevant peer-reviewed English-language papers that reported survival after surgical resection of DCC from January 2000 to January 2015. The following MeSH headings and keywords were used: distal bile duct cancer, distal cholangiocarcinoma, and distal bile duct carcinoma. The bibliographies of identified articles were further manually searched for additional citations. This study was performed in accordance with the guidelines of preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2009.4
2.2. Selection criteria
Inclusion criteria were: (1) original article; (2) patients with DCC undergoing resection with curative intent; (3) study populations aged at least 18 years; and (4) reported 5-year overall survival (OS). Studies from the same institution covering different time periods were included. Reviews, conference abstracts, nonhuman studies, case series with fewer than 10 patients, studies that focused on molecular markers, and studies that contained mixed populations without separate assessments were excluded.
2.3. Data extraction
Two reviewers (Y.Z. and S.L.) independently appraised each article using a predefined form. First author, publication year, study period, country of origin, trial design, sample size, patients' characteristics, and outcomes of interests were extracted. Differences in opinion between the two investigators were resolved by discussion and consensus. Margin status is classified as microscopically negative (R0) and microscopically positive (R1).
2.4. Statistical analysis
Summary statistics were reported as total and percentage for categorical variables and as median values and range for continuous variables, unless otherwise specified. The meta-analysis was performed using the Review Manager (RevMan) software, version 5.1 (The Cochrane Collaboration Software Update, Oxford, UK). Risk estimates from univariate analysis or multivariate estimating survival were obtained from each study and meta-analyzed for the prognostic factors using a random-effects model. Data were expressed as relative risks (RRs) with 95% confidence interval (95% CI). Where RR was not reported, published data and figures from original papers were used to calculate the RR and variance according to the methods described by Parmar et al.5 The impact of variables on survival was considered to be statistically significant if the 95% CI for the RR did not overlap 1. In the forest plot, squares indicate point estimates of prognostic effect with the size of the squares representing the weight attributed to each study. The horizontal lines represent 95% CI for RR. The pooled RR and its 95% (CI) are presented as a diamond. Statistical significance was set at p < 0.05.
3. Results
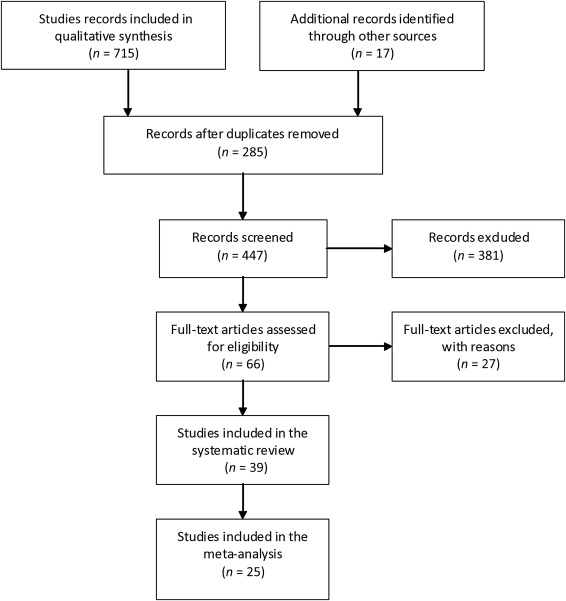
The initial literature search yielded 732 studies for potential inclusion. Of these, 39 publications totaling 3258 patients (range, 15–370 per study) met the inclusion criteria and were included for analysis (Figure 1). Characteristics of patients in the analyzed studies are summarized in Table 1.2; 3; 6; 7; 8; 9; 10; 11; 12; 13; 14; 15; 16; 17; 18; 19; 20; 21; 22; 23; 24; 25; 26; 27; 28; 29; 30; 31; 32; 33; 34; 35; 36; 37; 38; 39; 40; 41 ; 42 All studies were retrospective. Most reports originated from Asia (Japan, n = 16; Korea, n = 6; and China, n = 3), followed by USA (n = 8) and Europe (n = 6). Patient cohorts in three studies from Fong et al, 3 Nakeeb et al,6 and Ebata et al19 overlapped with those in other studies by Allen et al,23 Hong et al,28 and Kiriyama et al,2, respectively. The fifth, sixth, and seventh editions of the American Joint Committee on Cancer tumor-nodes-metastasis (TNM) classification system was used for tumor staging in five, 11; 12; 13; 14 ; 16 15, 17; 18; 19; 20; 21; 22; 23; 24; 26; 27; 28; 31 ; 32 and seven 35; 38; 39; 40; 41 ; 42 studies, respectively. Intraoperative frozen section examination was described in eight studies 17; 21; 27; 34; 38; 39; 40 ; 41; 11 studies reported the use of preoperative biliary drainage (PBD) by endoscopic procedure or percutaneous transhepatic procedure due to obstructive jaundice. 14; 18; 19; 24; 27; 31; 34; 35; 38; 40 ; 41 The study period extended from 1960 to 2013.
|
|
|
Figure 1. Flow diagram for the selection of eligible studies. |
| Study | Study period (Region) | n (M/F) | Age (y) a | PD | R0 R | LNM | PNI | LI | VI | PI |
|---|---|---|---|---|---|---|---|---|---|---|
| Nagorney et al (1993)2 | 1976–1985 (USA) | 22 (—) | — | 22 (100) | 12 (56) | — | — | — | — | — |
| Fong et al (1996)3 | 1983–1993 (USA) | 45 (—) | — | 39 (87) | 37 (82) | 19 (42) | — | — | — | — |
| Nakeeb et al (1996)6 | 1983–1993 (USA) | 73 (—) | — | 73 (100) | 66 (90) | — | — | — | — | — |
| Wade et al (1997)7 | 1987–1991 (USA) | 34 (—) | — | 30 (88) | — | — | — | — | — | — |
| Rijken et al (1998)8 | 1985–1996 (NL) | 47 (37/10) | 60 | 47 (100) | 25 (53) | 21 (45) | 29 (62) | — | 19 (40) | — |
| Zerbi et al (1998)9 | 1990–1996 (Italy) | 27 (19/8) | 62 | 27 (100) | 26 (96) | 23 (48) | 15 (56) | 20 (74) | — | — |
| Kayahara et al (1999)10 | 1973–1997 (Japan) | 50 (37/13) | 65 | 40 (80) | 36 (72) | 34 (68) | 42 (84) | — | — | — |
| Takao et al (1999)11 | 1980–1997 (Japan) | 64 (42/22) | 67 | 58 (91) | 42 (66) | 25 (39) | 48 (75) | 45 (70) | 35 (55) | 28 (44) |
| Bortolasi et al (2000)12 | 1988–1993 (USA) | 15 (8/7) | 65 | 15 (100) | 14 (93) | 4 (27) | 9 (60) | 4 (27) | — | — |
| Suzuki et al (2000)13 | 1960–1997 (Japan) | 99 (—) | — | 79 (80) | 79 (80) | — | — | — | — | — |
| Todoroki et al (2001)14 | 1997–2000 (Japan) | 57 (—) | — | 50 (88) | 26 (46) | 35 (67) | — | 30 (58) | — | — |
| Yoshida et al (2002)15 | 1995–2000 (Japan) | 26 (16/10) | 64 | 26 (100) | 22 (85) | 15 (58) | 22 (85) | 21 (81) | 15 (58) | — |
| Park et al (2004)16 | 1985–1997 (Korea) | 59 (—) | — | 48 (81) | 59 (100)b | — | — | — | — | — |
| Sakamoto et al (2005)17 | 1987–2003 (Japan) | 55 (41/14) | 66 | 45 (82) | 45 (82) | 27 (53) | 41 (80) | — | — | 24 (47) |
| Cheng et al (2007)18 | 1996–2002 (China) | 112 (78/44) | 56 | 112 (100) | 97 (87) | 25 (22) | — | — | — | 8 (7.1) |
| Ebata et al (2007)19 | 1975–2005 (Japan) | 95 (55/40) | 67 | 95 (100) | 85 (89) | 36 (38) | 69 (73) | 67 (71) | 29 (31) | 26 (27) |
| Murakami et al (2007)20 | 1990–2004 (Japan) | 43 (36/7) | 70 | 35 (81) | 30 (70) | 17 (40) | 26 (60) | — | — | 19 (44) |
| Sasaki et al (2007)21 | 1985–2005 (Japan) | 77 (—) | — | — | 71 (92) | — | — | — | — | — |
| Woo et al (2007)22 | 1991–2006 (Korea) | 91 (57/34) | 62 | 91 (100) | 91 (100)b | 23 (25) | 63 (69) | 21 (23) | 6 (7) | — |
| Allen et al (2008)23 | 1987–2005 (USA) | 98 (64/34) | 67 | 90 (92) | 82 (85) | 46 (47) | — | — | — | — |
| Bahra et al (2008)24 | 1990–2006 (Germany) | 95 (—) | 63 | 95 (100) | 77 (81) | 65 (68) | — | 57 (60) | — | 37 (39) |
| Shimizu et al (2008)25 | 1985–2001 (Japan) | 34 (19/15) | — | 29 (85) | 29 (85) | 11 (32) | 20 (59) | — | — | 18 (53) |
| van Roest et al (2008)26 | 1989–2006 (NL) | 19 (14/5) | 62 | 19 (100) | 18 (95) | — | 7 (37) | 2 (11) | — | — |
| Choi et al (2009)27 | 2000–2007 (Korea) | 125 (84/41) | 60 | 94 (75) | 103 (82) | 41 (33) | 51 (41) | — | — | 57 (46) |
| Hong et al (2009)28 | 1984–2004 (USA) | 147 (90/57) | 61 | 210 (100) | 133 (91) | 93 (63) | 98 (67) | — | 109 (74) | 19 (13) |
| Nomura et al (2009)29 | 1991–2005 (Japan) | 57 (39/18) | 67 | 46 (81) | 35 (61) | — | — | 46 (81) | 35 (61) | 18 (32) |
| Hatzaras et al (2010)30 | 1992–2007 (USA) | 18 (13/5) | 66 | 18 (100) | 15 (83) | 6 (33) | 6 (33) | 2 (11) | — | — |
| Kawai et al (2010)31 | 1991–2004 (Japan) | 62 (39/23) | 67 | 58 (94) | 48 (77) | 24 (39) | 35 (56) | 21 (34) | 13 (21) | 34 (55) |
| Qiao et al (2011)32 | 1998–2008 (China) | 122 (—) | — | 122 (100) | 98 (86) | 39 (35) | — | — | — | — |
| Noji et al (2012)33 | 1997–2007 (Japan) | 118 (67/51) | 57 | 93 (79) | 105 (89) | 38 (32) | 92 (77) | — | — | — |
| van der Gaag et al (2012)34 | 1992–2007 (NL) | 90 (—) | — | — | 51 (57) | 45 (50) | — | — | — | — |
| Chung et al (2013)35 | 1995–2011 (Korea) | 241 (166/75) | 6 | 241 (100) | 227 (96) | 72 (30) | — | — | — | — |
| Pomianowska et al (2013)36 | 1998–2009 (Norway) | 46 (—) | — | 46 (100) | 21 (46) | 26 (57) | 36 (78) | — | 26 (57) | — |
| Tan et al (2013)37 | 2003–2008 (China) | 82 (55/27) | 54 | 82 (100) | — | 52 (63) | 58 (71) | — | — | — |
| Iso et al (2014)38 | 2000–2013 (Japan) | 90 (59/31) | 69 | 90 (100) | 81 (90) | 28 (31) | — | — | — | — |
| Kim et al (2014)39 | 2004–2011 (Korea) | 91 (59/32) | 67 | 91 (100) | 91 (100)b | 32 (35) | 57 (63) | 23 (25) | — | 53 (58) |
| Kwon et al (2014)40 | 1990–2011 (Korea) | 133 (81/52) | — | 90 (68) | 102 (77) | 33 (25) | 55 (41) | 25 (20) | — | — |
| Miura et al (2015)41 | 1980–2013 (Japan) | 129 (88/41) | 68 | 129 (100) | 104 (81) | 77 (60) | 95 (74) | 88 (68) | 70 (54) | 60 (47) |
| Kiriyama et al (2015)42 | 2001–2000 (Japan) | 370 (249/121) | 69 | 370 (100) | 346 (94) | 213 (58) | 261 (71) | 253 (68) | — | 212 (57) |
Data are presented as n (%) unless otherwise indicated.
F = female; LI = lymphatic invasion; LNM = lymph node metastasis; M = male; PD = pancreaticoduodenectomy; PI = pancreatic invasion; PNI = perineural invasion; R0 R = R0 resection; VI = venous invasion.
a. Median or mean.
b. Cases with a positive microscopic resection margin were excluded.
Ninety-five percent of patients (range, 68–100%) underwent pancreaticoduodenectomy and 5% (range, 0–32%) patients underwent bile duct resection, with a curative resection (R0 resection) rate of 84% (range, 46–100%). Lymph node metastasis, perineural invasion, lymphatic invasion, vascular invasion, and pancreatic invasion was identified in 43% (range, 22–68%), 66% (range, 33–85%), 52% (range, 11–81%), 46% (range, 7–74%), and 41% (range, 7–58%) of patients, respectively.
3.1. Survival and prognostic factors
The operative mortality rate ranged from 0% to 8% (median 4%) among the studies analyzed. The 5-year OS rate following resection ranged from 13% to 54% (median 37%), and the median survival from 18 months to 102 months (median 33 months; Table 2). The 5-year OS rate of those with R0 resection and without R0 resection were 27–63% and (0–40%), respectively.
| Study | Mortalityn (%) | Median survival (mo) | Overall survival (%) | ||
|---|---|---|---|---|---|
| 1 y | 3 y | 5 y | |||
| Nagorney et al2 | — | 24 | 71 | 43 | 43 |
| Fong et al3 | 2 (4) | 33 | 79 | 46 | 27 |
| Nakeeb et al6 | 0 (0) | 22 | 70 | 31 | 28 |
| Wade et al7 | — | — | 68 | 19 | 14 |
| Rijken et al8 | 3 (6) | 20 | — | — | 20 |
| Zerbi et al9 | 1 (4) | 22 | 78 | 20 | 13 |
| Kayahara et al10 | 1 (2) | — | 70 | 47 | 35 |
| Takao et al11 | 5 (8) | — | — | — | 32 |
| Bortolasi et al12 | 0 (0) | 21 | 73 | 27 | 20 |
| Suzuki et al13 | 3 (3) | — | — | — | 37 |
| Todoroki et al14 | 3 (5) | 37 | — | — | 39 |
| Yoshida et al15 | 1 (4) | 21 | 65 | 37 | 37 |
| Park et al16 | 0 (0) | 45 | 73 | 56 | 47 |
| Sakamoto et al17 | 4 (7) | 38 | 78 | 52 | 24 |
| Cheng et al18 | 4 (3) | 36 | 86 | 51 | 25 |
| Ebata et al19 | 5 (5) | 30 | 75 | 47 | 35 |
| Murakami et al20 | 0 (0) | 26 | 72 | 53 | 44 |
| Sasaki et al21 | — | 55 | — | — | 37 |
| Woo et al22 | — | — | — | — | 54 |
| Allen et al23 | 3 (3) | — | — | — | 43 |
| Bahra et al24 | 4 (4) | — | 60 | 36 | 29 |
| Shimizu et al25 | 1 (3) | 35 | — | — | 45 |
| van Roest et al26 | — | 102 | — | — | 54 |
| Choi et al27 | 5 (4) | 35 | 86 | 49 | 38 |
| Hong et al28 | — | 20 | — | 33 | 18 |
| Nomura et al29 | 2 (4) | 34 | — | — | 36 |
| Hatzaras et al30 | 1 (6) | 18 | 68 | 27 | 27 |
| Kawai et al31 | — | — | 88 | 63 | 51 |
| Qiao et al32 | 8 (7) | 36 | 83 | 49 | 33 |
| Noji et al33 | — | — | — | 57 | 51 |
| van der Gaag et al34 | — | — | 71 | 39 | 19 |
| Chung et al35 | 4 (2) | 73 | 78 | 55 | 48 |
| Pomianowska et al36 | — | 22 | 82 | 31 | 26 |
| Tan et al37 | 2 (2) | — | 70 | 43 | 37 |
| Iso et al38 | 0 | — | 90 | 51 | 45 |
| Kim et al39 | 5 (4) | 33 | 84 | 50 | 39 |
| Kwon et al40 | — | — | 87 | 54 | 41 |
| Miura et al41 | 9 (7) | 33 | 79 | 48 | 37 |
| Kiriyama et al42 | 18 (4) | 42 | — | 53 | 41 |
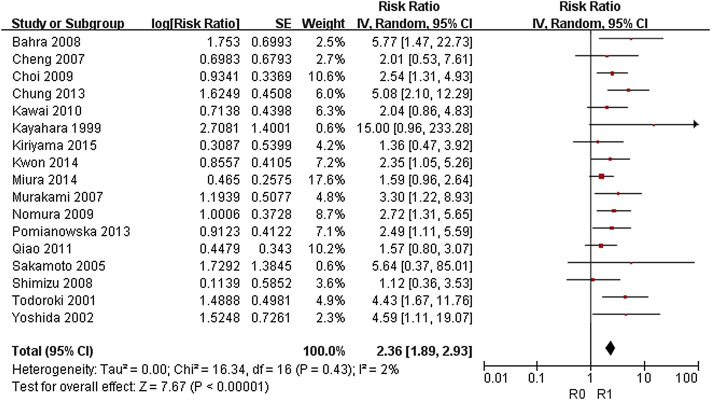
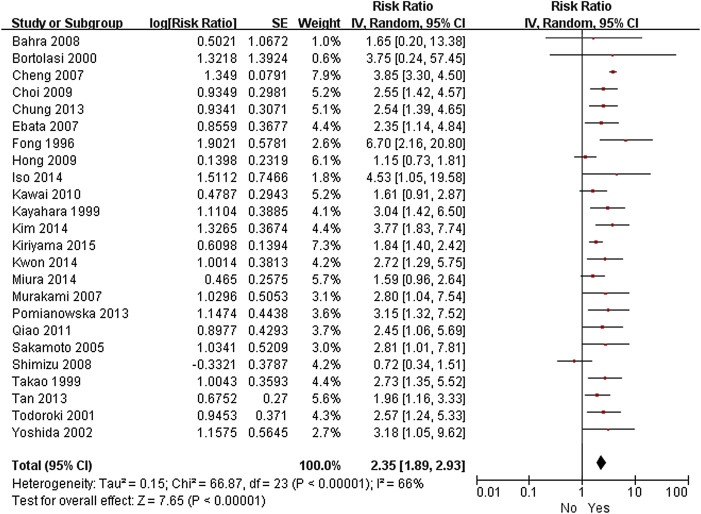
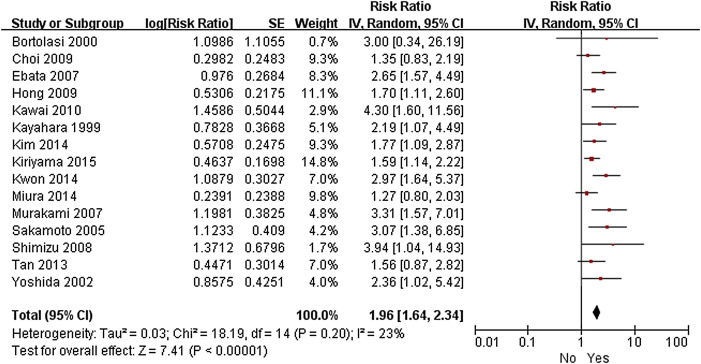
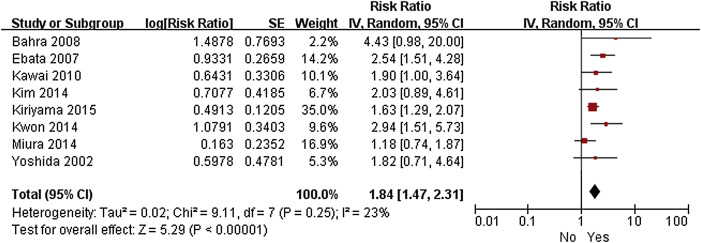
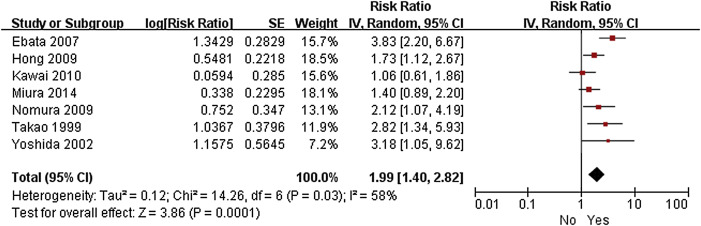
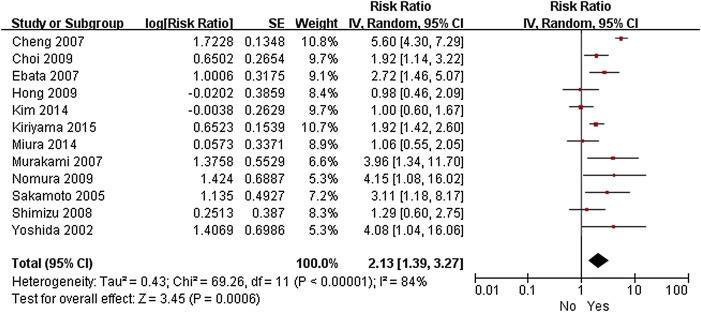
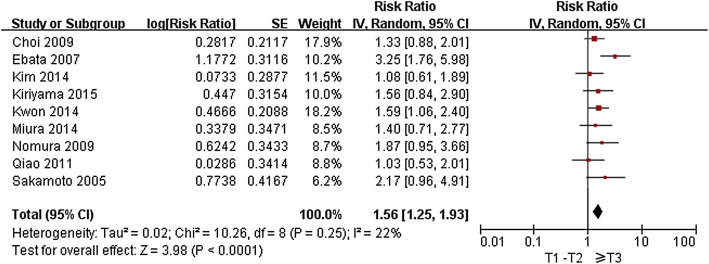
Twenty-five studies were eligible for inclusion in the meta-analysis.3; 10; 11; 12; 14; 15; 17; 18; 19; 20; 24; 25; 27; 28; 29; 31; 32; 35; 36; 37; 38; 39; 40; 41 ; 42 R1 resection (RR 2.36, 95% CI 1.89–2.93; p < 0.001), lymph node metastasis (RR 2.35, 95% CI 1.89–2.93; p < 0.001), perineural invasion (RR 1.96, 95% CI 1.64–2.34; p < 0.001), lymphatic invasion (RR 1.84, 95% CI 1.47–2.31; p < 0.001), vascular invasion (RR 1.99, 95% CI 1.40–2.82; p < 0.001), pancreatic invasion (RR 2.13, 95% CI 1.39–3.27; p < 0.001), and pathological tumor stage ≥ T3 (RR 1.56, 95% CI 1.25–1.93; p < 0.001) were found to be associated with shorter OS ( Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7 ; Figure 8). However, sex, age, and blood transfusion have no impact on survival (Table 3).
|
|
|
Figure 2. Forest plot of the meta-analysis of the relationship between resection margin status and overall survival. |
|
|
|
Figure 3. Forest plot of the meta-analysis of the relationship between lymph node metastasis and overall survival. |
|
|
|
Figure 4. Forest plot of the meta-analysis of the relationship between perineural invasion and overall survival. |
|
|
|
Figure 5. Forest plot of the meta-analysis of the relationship between lymphatic invasion and overall survival. |
|
|
|
Figure 6. Forest plot of the meta-analysis of the relationship between venous invasion and overall survival. |
|
|
|
Figure 7. Forest plot of the meta-analysis of the relationship between pancreatic invasion and overall survival. |
|
|
|
Figure 8. Forest plot of the meta-analysis of the relationship between pathological tumor stage and overall survival. |
| Patient group | RR (95% CI) | p | 5-year OS (%) Median (range) | No. of studies |
|---|---|---|---|---|
| Sex | 13 | |||
| Male | 1.00 (ref) | 40 (27–53) | ||
| Female | 0.94 (0.73–1.20) | 0.60 | 45 (21–71) | |
| Age (y) | 14 | |||
| Young | 1.00 (ref) | 40 (25–69) | ||
| Old | 1.13 (0.95–1.33) | 0.16 | 36 (0–54) | |
| Resection margin status | 17 | |||
| R0 | 1.00 (ref) | 44 (27–63) | ||
| R1 | 2.36 (1.89–2.93) | < 0.001 | 16 (0–40) | |
| Lymph node metastasis | 24 | |||
| No | 1.00 (ref) | 53 (30–65) | ||
| Yes | 2.35 (1.89–2.93) | < 0.001 | 20 (0–40) | |
| Perineural invasion | 15 | |||
| No | 1.00 (ref) | 57 (33–78) | ||
| Yes | 1.96 (1.64–2.34) | < 0.001 | 29 (11–35) | |
| Lymphatic invasion | 8 | |||
| No | 1.00 (ref) | 54 (42–64) | ||
| Yes | 1.84 (1.47–2.31) | < 0.001 | 28 (7–43) | |
| Venous invasion | 7 | |||
| No | 1.00 (ref) | 53 (44–64) | ||
| Yes | 1.99 (1.40–2.82) | < 0.001 | 26 (14–54) | |
| Pancreatic invasion | 12 | |||
| No | 1.00 (ref) | 47 (27–62) | ||
| Yes | 2.13 (1.39–3.27) | < 0.001 | 17 (0–40) | |
| Pathological tumor stage | 9 | |||
| T1–T2 | 1.00 (ref) | 50 (37–-64) | ||
| ≥T3 | 1.546 (1.25–1.93) | < 0.001 | 19 (13–37) | |
| Blood transfusion | 5 | |||
| No | 1.00 (ref) | 36 (29–53) | ||
| Yes | 1.25 (0.86–1.83) | 0.24 | 26 (18–51) |
CI = confidence interval; OS = overall survival; Ref = reference; RR = relative risk.
4. Discussion
The clinical data of patients with DCC are relative scarce, probably due to the rarity of this tumor, and are limited to a small number of patients in individual reports. The current review of 3258 patients from 39 studies provides a comprehensive appraisal of the current status of surgical resection for DCC and facilitates analysis of prognostic factors associated with survival.
Significant improvements in short-term results after resection for DCC have been achieved in the past decades as a result of advancement in surgical techniques and postoperative management, with operative mortality of < 5% in high-volume centres.18 ; 28 However, the long-term outcome is still unsatisfactory. The 5-year OS rate ranged from 13% to 54%, and did not exceed 50% in most series. Bile duct cancer exhibits two major forms of tumor extension—superficial spread and submucosal infiltration—making it difficult to achieve cancer-free margin and consequently worsen prognosis.17 This study shows that the 5-year OS rate for patients undergoing R0 resection (27–60%) is significantly higher than those for patients undergoing R1 resection (0–40%) and that the status of the resection margin is a strong prognostic factor. This finding highlights that the surgeon should make an effort to achieve R0 resection. The extent of ductal spread of DCC cannot be determined preoperatively by diagnostic imaging modalities, and therefore intraoperative frozen section diagnosis of the stump of the bile duct has been recommended. When residual disease is detected at the stump, additional resection of the bile duct are required as far as is technically feasible.
Kwon et al40 reported that 5-year survival rates of patients with pancreaticoduodenectomy and bile duct resection were 46.6% and 30.0% (p = 0.105), respectively; this difference, although not statistically significant, can be attributed to a higher rate of positive resection margins in patients with bile duct resection (90.0% vs. 48.8%, p < 0.0001). This finding indicated that pancreaticoduodenectomy is the preferred approach for DCC. Bile duct resection is considered only in the comorbidities of patients who are intolerant of pancreaticoduodenectomy or patients who are judged that curative resection can be achieved. 40
The poor prognosis is also related to the fact that many patients present with advanced disease at the time of surgery, as reflected by the high incidence of lymph node metastasis (43%), perineural invasion (66%), lymphatic invasion (52%), vascular invasion (46%), and pancreatic invasion (41%). Each of these factors in turn has a negative impact on survival. In an effort to improve prognosis, some surgeons, especially in Japan, advocate the complete removal of the primary DCC with extended lymphadenectomy (i.e. para-aortic lymph node dissection extended from the celiac axis to the inferior mesenteric artery and from the right margin of the inferior vena cava to the left margin of the abdominal aorta) and dissection of the nerve plexus around major vessels.10 ; 15 However, the clinical significance of this strategy is still controversial. One randomized controlled trial (RCT) of 294 patients found no differences in survival between groups of patients undergoing standard and extended surgical procedures, but only 16% had tumors of distal bile duct origin.43 Further investigations with larger groups of patients are required to evaluate the value of extended surgery for DCC.
Whether blood transfusion is a negative predictor of survival in the setting of oncological surgery is a matter of debate.44 The current study show that blood transfusion was not a predictor of outcome on pooled analysis, just that it might reflect the extensiveness of the operation, and its effect on prognosis was largely attributable to extensiveness of the operation rather than blood transfusion itself. Nonetheless, there is evidence to suggest that transfusions have immunosuppressive effects that promote tumor growth and metastasis.44 Still, decrease blood loss should be sought whenever possible.
Liver metastasis is a major cause of treatment failure in DCC after resection. Hepatectomy for a solitary metastasis is the treatment of choice but < 15% of patients are candidates for such treatment.45 Adjuvant therapy has been shown to have a survival benefit for pancreatic cancer by decreasing liver metastasis.46 However, the role of this strategy for DCC is not well established. Yoshida et al15 reported that the use of adjuvant chemotherapy was an independent prognostic factor for survival. Another study from Johns Hopkins Medical Center observed that the mean survival for patients who received adjuvant chemoradiation was 36.9 months, compared with 22 months for surgery alone (p < 0.04). 47 However, other studies have been unable to reproduce these findings, 18; 20; 27; 31 ; 32 probably due to the small number of case studied. In this context, large RCTs are needed to determine whether this cohort of patients can actually benefit from postoperative adjuvant therapy, particularly those with lymph node metastasis or positive resection margin. The efficacy and safety of single-agent gemcitabine or gemcitabine-based combinations in the adjuvant treatment of cholangiocarcinoma after potentially curative resection have been tested in several trials. 48; 49 ; 50 It is hoped that these ongoing trials will contribute to the determination of optimal adjuvant treatment, which will result in a survival benefit with DCC.
Most patients with DCC will present with obstructive jaundice, which is associated with impaired immune responses, disturbances in coagulation, and renal and other organ dysfunction. Furthermore, in some studies, authors have shown that the elevated serum bilirubin as an independent prognostic factor.2 ; 12 Nonetheless, the beneficial effect of PBD remained uncertain. A recent meta-analysis of six RCTs showed that patients undergoing surgery for obstructive jaundice is associated with similar mortality but increased serious morbidity compared with no PBD.51 However, these RCTs included tumors causing proximal and distal bile duct obstruction, but such tumors are now considered to be different diseases and to require different forms of treatment. Therefore, new properly designed RCTs focused exclusively on the unique population of patients with DCC are warranted.
A limitation of the current study is the retrospective nature of the studies included, which could have resulted in recall bias. In addition, the prognostic significance of the number or ratio of involved nodes, serum bilirubin and carbohydrate antigen 19-9 levels, and tumor size and location were not analyzed owing to the limited data.
In conclusion, this review of 3258 patients from 39 studies represents the largest body of currently available information regarding surgical resection for DCC. In general, prognosis of DCC after resection is poor. R0 resection results in a substantially improved survival and represents one of the most important prognostic variables.
Acknowledgments
The authors express their thanks to Doctor Yanfang Zhao (Department of Health Statistics, Second Military Medical University, Shanghai, China) for her critical revision of the Statistical analysis section.
References
- 1 N. Lad, D.A. Kooby; Distal cholangiocarcinoma; Surg Oncol Clin N Am, 23 (2014), pp. 265–287
- 2 D.M. Nagorney, J.H. Donohue, M.B. Farnell, C.D. Schleck, D.M. Ilstrup; Outcomes after curative resections of cholangiocarcinoma; Arch Surg, 128 (1993), pp. 871–879
- 3 Y. Fong, L.H. Blumgart, E. Lin, J.G. Fortner, M.F. Brennan; Outcome of treatment for distal bile duct cancer; Br J Surg, 83 (1996), pp. 1712–1715
- 4 D. Moher, A. Liberati, J. Tetzlaff, D.G. Altman, PRISMA Group; Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement; BMJ, 339 (2009), p. b2535
- 5 M.K. Parmar, V. Torri, L. Stewart; Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints; Stat Med, 17 (1998), pp. 2815–2834
- 6 A. Nakeeb, H.A. Pitt, T.A. Sohn, et al.; Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors; Ann Surg, 224 (1996), pp. 463–473
- 7 T.P. Wade, C.N. Prasad, K.S. Virgo, F.E. Johnson; Experience with distal bile duct cancers in U.S. Veterans Affairs hospitals: 1987–1991; J Surg Oncol, 64 (1997), pp. 242–245
- 8 A.M. Rijken, T.M. van Gulik, M.M. Polak, P.D. Sturm, D.J. Gouma, G.J. Offerhaus; Diagnostic and prognostic value of incidence of K-ras codon 12 mutations in resected distal bile duct carcinoma; J Surg Oncol, 68 (1998), pp. 187–192
- 9 A. Zerbi, G. Balzano, B.E. Leone, E. Angeli, P. Veronesi, V. Di Carlo; Clinical presentation, diagnosis and survival of resected distal bile duct cancer; Dig Surg, 15 (1998), pp. 410–416
- 10 M. Kayahara, T. Nagakawa, T. Ohta, H. Kitagawa, H. Tajima, K. Miwa; Role of nodal involvement and the periductal soft-tissue margin in middle and distal bile duct cancer; Ann Surg, 229 (1999), pp. 76–83
- 11 S. Takao, H. Shinchi, K. Uchikura, M. Kubo, T. Aikou; Liver metastases after curative resection in patients with distal bile duct cancer; Br J Surg, 86 (1999), pp. 327–331
- 12 L. Bortolasi, L.J. Burgart, G.G. Tsiotos, E. Luque-De León, M.G. Sarr; Adenocarcinoma of the distal bile duct. A clinicopathologic outcome analysis after curative resection; Dig Surg, 17 (2000), pp. 36–41
- 13 M. Suzuki, M. Unno, M. Oikawa, K. Endo, Y. Katayose, S. Matsuno; Surgical treatment and postoperative outcomes for middle and lower bile duct carcinoma in Japan—experience of a single institute; Hepatogastroenterology, 47 (2000), pp. 650–657
- 14 T. Todoroki, T. Kawamoto, N. Koike, K. Fukao, J. Shoda, H. Takahashi; Treatment strategy for patients with middle and lower third bile duct cancer; Br J Surg, 88 (2001), pp. 364–370
- 15 T. Yoshida, T. Matsumoto, A. Sasaki, Y. Morii, M. Aramaki, S. Kitano; Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer; Arch Surg, 137 (2002), pp. 69–73
- 16 S.W. Park, Y.S. Park, J.B. Chung, et al.; Patterns and relevant factors of tumor recurrence for extrahepatic bile duct carcinoma after radical resection; Hepatogastroenterology, 51 (2004), pp. 1612–1618
- 17 Y. Sakamoto, T. Kosuge, K. Shimada, et al.; Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins; Surgery, 137 (2005), pp. 396–402
- 18 Q. Cheng, X. Luo, B. Zhang, X. Jiang, B. Yi, M. Wu; Distal bile duct carcinoma: prognostic factors after curative surgery. A series of 112 cases; Ann Surg Oncol, 14 (2007), pp. 1212–1219
- 19 T. Ebata, M. Nagino, H. Nishio, T. Igami, Y. Yokoyama, Y. Nimura; Pancreatic and duodenal invasion in distal bile duct cancer: paradox in the tumor classification of the American Joint Committee on Cancer; World J Surg, 31 (2007), pp. 2008–2015
- 20 Y. Murakami, K. Uemura, Y. Hayashidani, et al.; Prognostic significance of lymph node metastasis and surgical margin status for distal cholangiocarcinoma; J Surg Oncol, 95 (2007), pp. 207–212
- 21 R. Sasaki, Y. Takeda, O. Funato, et al.; Significance of ductal margin status in patients undergoing surgical resection for extrahepatic cholangiocarcinoma; World J Surg, 31 (2007), pp. 1788–1796
- 22 S.M. Woo, J.K. Ryu, S.H. Lee, et al.; Recurrence and prognostic factors of ampullary carcinoma after radical resection: comparison with distal extrahepatic cholangiocarcinoma; Ann Surg Oncol, 14 (2007), pp. 3195–3201
- 23 P.J. Allen, A.S. Reiner, M. Gonen, et al.; Extrahepatic cholangiocarcinoma: a comparison of patients with resected proximal and distal lesions; HPB (Oxford), 10 (2008), pp. 341–346
- 24 M. Bahra, D. Jacob, J.M. Langrehr, U.P. Neumann, P. Neuhaus; Carcinoma of the distal and middle bile duct: surgical results, prognostic factors, and long-term follow-up; J Hepatobiliary Pancreat Surg, 15 (2008), pp. 501–507
- 25 Y. Shimizu, F. Kimura, H. Shimizu, H. Yoshidome, M. Ohtsuka, M. Miyazaki; The morbidity, mortality, and prognostic factors for ampullary carcinoma and distal cholangiocarcinoma; Hepatogastroenterology, 55 (2008), pp. 699–703
- 26 M.H. van Roest, A.S. Gouw, P.M. Peeters, et al.; Results of pancreaticoduodenectomy in patients with periampullary adenocarcinoma: perineural growth more important prognostic factor than tumor localization; Ann Surg, 248 (2008), pp. 97–103
- 27 S.B. Choi, S.W. Park, K.S. Kim, J.S. Choi, W.J. Lee; The survival outcome and prognostic factors for middle and distal bile duct cancer following surgical resection; J Surg Oncol, 99 (2009), pp. 335–342
- 28 S.M. Hong, T.M. Pawlik, H. Cho, et al.; Depth of tumor invasion better predicts prognosis than the current American Joint Committee on Cancer T classification for distal bile duct carcinoma; Surgery, 146 (2009), pp. 250–257
- 29 T. Nomura, Y. Tsuchiya, A. Nashimoto, et al.; Prognostic factors for radical resection of middle and distal bile duct cancer; Hepatogastroenterology, 56 (2009), pp. 294–298
- 30 I. Hatzaras, N. George, P. Muscarella, W.S. Melvin, E.C. Ellison, M. Bloomston; Predictors of survival in periampullary cancers following pancreaticoduodenectomy; Ann Surg Oncol, 17 (2010), pp. 991–997
- 31 M. Kawai, M. Tani, Y. Kobayashi, et al.; The ratio between metastatic and examined lymph nodes is an independent prognostic factor for patients with resectable middle and distal bile duct carcinoma; Am J Surg, 199 (2010), pp. 447–452
- 32 Q.L. Qiao, T.P. Zhang, J.C. Guo, et al.; Prognostic factors after pancreatoduodenectomy for distal bile duct cancer; Am Surg, 77 (2011), pp. 1445–1448
- 33 T. Noji, M. Miyamoto, K.C. Kubota, et al.; Evaluation of extra capsular lymph node involvement in patients with extra-hepatic bile duct cancer; World J Surg Oncol, 10 (2012), p. 106
- 34 N.A. van der Gaag, J.J. Kloek, J.K. de Bakker, et al.; Survival analysis and prognostic nomogram for patients undergoing resection of extrahepatic cholangiocarcinoma; Ann Oncol, 23 (2012), pp. 2642–2649
- 35 Y.J. Chung, D.W. Choi, S.H. Choi, J.S. Heo, D.H. Kim; Prognostic factors following surgical resection of distal bile duct cancer; J Korean Surg Soc, 85 (2013), pp. 212–218
- 36 E. Pomianowska, A. Westgaard, Ø. Mathisen, O.P. Clausen, I.P. Gladhaug; Prognostic relevance of number and ratio of metastatic lymph nodes in resected pancreatic, ampullary, and distal bile duct carcinomas; Ann Surg Oncol, 20 (2013), pp. 233–241
- 37 X. Tan, K. Xiao, W. Liu, S. Chang, T. Zhang, H. Tang; Prognostic factors of distal cholangiocarcinoma after curative surgery: a series of 84 cases; Hepatogastroenterology, 60 (2013), pp. 1892–1895
- 38 Y. Iso, J. Kita, M. Kato, M. Shimoda, K. Kubota; When hepatic-side ductal margin is positive in N+ cases, additional resection of the bile duct is not necessary to render the negative hepatic-side ductal margin during surgery for extrahepatic distal bile duct carcinoma; Med Sci Monit, 20 (2014), pp. 471–475
- 39 H.J. Kim, C.Y. Kim, Y.H. Hur, et al.; The prognostic factors for survival after curative resection of distal cholangiocarcinoma: perineural invasion and lymphovascular invasion; Surg Today, 44 (2014), pp. 1879–1886
- 40 H.J. Kwon, S.G. Kim, J.M. Chun, W.K. Lee, Y.J. Hwang; Prognostic factors in patients with middle and distal bile duct cancers; World J Gastroenterol, 20 (2014), pp. 6658–6665
- 41 F. Miura, K. Sano, H. Amano, et al.; Evaluation of portal vein invasion of distal cholangiocarcinoma as borderline resectability; J Hepatobiliary Pancreat Sci, 22 (2015), pp. 294–300
- 42 M. Kiriyama, T. Ebata, T. Aoba, et al.; Prognostic impact of lymph node metastasis in distal cholangiocarcinoma; Br J Surg, 102 (2015), pp. 399–406
- 43 C.J. Yeo, J.L. Cameron, K.D. Lillemoe, et al.; Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality; Ann Surg, 236 (2002), pp. 355–366
- 44 H. Luan, F. Ye, L. Wu, Y. Zhou, J. Jiang; Perioperative blood transfusion adversely affects prognosis after resection of lung cancer: a systematic review and a meta-analysis; BMC Surg, 14 (2014), p. 34
- 45 I. Kurosaki, M. Minagawa, C. Kitami, K. Takano, K. Hatakeyama; Hepatic resection for liver metastases from carcinomas of the distal bile duct and of the papilla of Vater; Langenbecks Arch Surg, 396 (2011), pp. 607–613
- 46 H. Oettle, P. Neuhaus; Adjuvant therapy in pancreatic cancer: a critical appraisal; Drugs, 67 (2007), pp. 2293–2310
- 47 M.A. Hughes, D.A. Frassica, C.J. Yeo, et al.; Adjuvant concurrent chemoradiation for adenocarcinoma of the distal common bile duct; Int J Radiat Oncol Biol Phys, 68 (2007), pp. 178–182
- 48 NCT01043172. A study of gemcitabine as an adjuvant treatment for cholangiocarcinoma after surgical resection. Available from https://www.clinicaltrials.gov/ct2/show/NCT01043172?term=cholangiocarcinoma&rank=67 Accessed 10.06.15.
- 49 A. Stein, D. Arnold, J. Bridgewater, et al.; Adjuvant chemotherapy with gemcitabine and cisplatin compared to observation after curative intent resection of biliary tract cancer (ACTICCA-1); BMC Cancer, 15 (2015), p. 564
- 50 M. Toyoda, T. Ajiki, Y. Fujiwara, et al.; A Phase I study of adjuvant chemotherapy with gc in biliary tract cancer undergoing resection without major hepatectomy; Cancer Chemother Pharmacol, 73 (2014), pp. 1295–1301
- 51 Y. Fang, K.S. Gurusamy, Q. Wang, et al.; Meta-analysis of randomized clinical trials on safety and efficacy of biliary drainage before surgery for obstructive jaundice; Br J Surg, 100 (2013), pp. 1589–1596
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?