Summary
Hepatobiliary involvement by malignant lymphoma is usually a secondary manifestation of systemic disease, whereas primary non-Hodgkins lymphoma of the extrahepatic biliary ducts is an extremely rare entity. We describe the case of a 57-year-old man who presented with an acute onset of obstructive jaundice and severe itching. Abdominal ultrasonography and computed tomography revealed intrahepatic and common hepatic ducts dilatation. Magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography showed a mid-common bile duct stricture. The patient was presumed to have cholangiocarcinoma of the common bile duct, and an en bloc resection of the tumor with Roux-en-Y hepaticojejunostomy and porta-hepatis lymph nodes dissection was performed. Histopathology and immunohistochemistry revealed a large B cell non-Hodgkins lymphoma. The patient received six cycles of combination chemotherapy using cyclophosphamide, vincristine, prednisone, and rituximab (CVP-R) protocol, and after a 5-year follow-up he is still in complete remission. We also reviewed the cases published from 1982 to 2012, highlighting the challenges in reaching a correct preoperative diagnosis and the treatment modalities used in each case.
Keywords
bile duct;non-Hodgkins lymphoma
1. Introduction
Non-Hodgkins lymphoma (NHL) accounts for 1–2% of all cases of malignant biliary obstruction.1 To our knowledge and after reviewing the literature since the first case was published by Nguyen2 in 1982, only 28 cases have been reported. Herein we present another case of primary NHL of the common bile duct. A literature review was conducted of the challenges in arriving at the diagnosis preoperatively and the debate around the optimal treatment modalities.
2. Case report
A 57-year-old man with no previous chronic medical illnesses presented with a 2-week history of severe itching all over his body, associated with general fatigue, malaise, and nausea, without vomiting or anorexia. He also reported having a yellowish discoloration of sclera, dark (tea color) urine, and a bulky foul-smelling stool. However, he denied any history of fever or chills, abdominal pain, previous episodes of similar symptoms, recent travels, or contact with sick people. He is not on any regular medications, and he denied recent ingestion of any drug. His surgical history and family history showed no significant finding. Moreover, he has a 40 pack-year smoking history but no history of alcohol consumption or illicit drug use.
On presentation his vital signs were within normal limits. The physical examination revealed deep scleral and skin jaundice with itching marks on his skin. There was no cervical lymphadenopathy and no stigmata of chronic liver disease. An abdominal examination revealed a soft and lax abdomen with mild tenderness over the epigastric and right upper quadrant areas, and active bowel sounds but no masses or hepatosplenomegaly.
His laboratory results showed hemoglobin, white cell count, and platelets of 15 g/dL, 7 × 103/mm3, and 162 × 103, respectively. His serum total bilirubin, direct bilirubin, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, gamma glutamyl transpeptidase, lactate dehydrogenase, and amylase results were 18.3 mg/dL 16.1 mg/dL, 116 U/L, 66 U/L, 161 U/L, 658 U/L, 898 U/L, and 58 U/L, respectively. His blood carbohydrate antigen 19-9 level rose to more than 1200 U/mL, and carcinoembryonic antigen was within normal levels at 0.88 ng/mL. Hepatitis A, B, and C serology was negative.
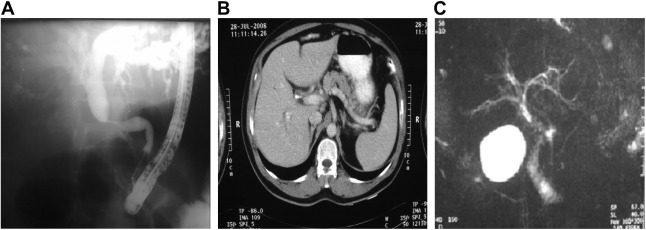
Abdominal ultrasonography revealed dilated common hepatic and intrahepatic ducts. An endoscopic retrograde cholangiopancreatography (ERCP) was subsequently performed and showed a 3-cm mid-common bile duct stricture with significantly dilated intrahepatic and common hepatic biliary ducts. The rushing cytology of the common bile duct was suspicious for malignancy. A 9-cm, 10 F stent was inserted across this for drainage (Fig. 1A).
|
|
|
Figure 1. Imaging studies. (A) Endoscopic retrograde cholangiopancreatography showing the mid common bile duct stricture. (B) Computed tomography scan of the abdomen showing intrahepatic bile tract dilatation. (C) Magnetic resonance cholangiopancreatography showing the tapered stricture of the distal common bile duct. |
The abdominal computed tomography (CT) scan revealed a mild intrahepatic biliary tree dilatation but was otherwise unremarkable (Fig. 1B).
Magnetic resonance cholangiopancreatography showed a marked tapered stricture at the distal common bile duct with mild to moderate dilatation of biliary tree proximally, and a normal pancreatic duct (Fig. 1C).
Based on the above presentation and investigations, a presumptive diagnosis of cholangiocarcinoma was made, and extrahepatic biliary tract excision, a Roux-en-Y hepaticojejunostomy, and porta-hepatis lymph nodes excision were performed.
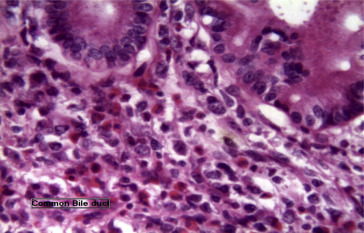
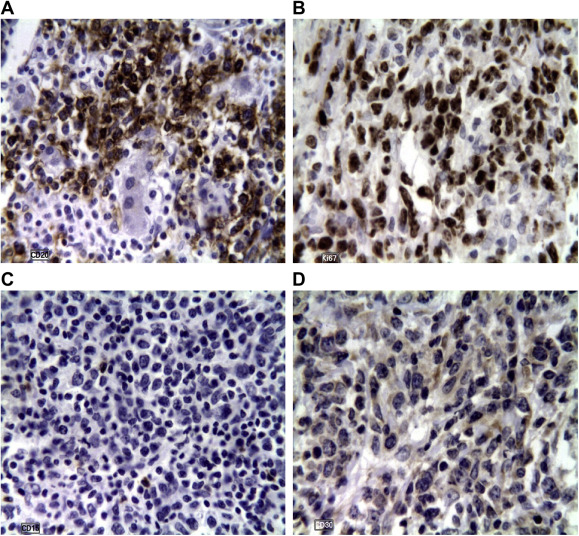
A histopathologic examination of the common bile duct revealed a large B cell-type NHL with tumor-free surgical resection margins (Fig. 2), and the porta-hepatis lymph nodes showed a reactive nonspecific hyperplasia. Immunohistochemical staining was positive for CD3, CD5, CD20, CD45, BCL2, and Ki67, and negative for CD15 and CD30 (Fig. 3).
|
|
|
Figure 2. Histopathology of the common bile duct showing proliferating lymphocytes of medium to large size, in a background of eosinophils, neutrophils, and reactive T cell lymphocytes. Many mitotic figures and apoptotic bodies are seen. |
|
|
|
Figure 3. Immunohistochemistry showing (A) positive CD20, a marker of B cell lymphoma; (B) positive Ki67 in 80% of the slide reflecting a high grade; (C) negative CD15, a marker of Hodgkins lymphoma; (D) negative CD30, a marker of Hodgkins lymphoma. |
The patient was referred to the oncology clinic, where a positron emission tomography showed no evidence of malignant lesions. He received six cycles of chemotherapy using the CVP-R (cyclophosphamide, vincristine, prednisone, and rituximab) protocol. One-year follow-up chest, abdomen, and pelvis CT and whole-body positron emission tomography scans revealed no evidence of malignancy. He received six maintenance courses of rituximab (anti-CD20) and remains in complete remission 5 years from the time of diagnosis with a normal whole-body CT scan.
3. Discussion
Diffuse large B cell lymphoma (DLBCL) is the most common lymphoid neoplasm and the most common histologic subtype of NHL, accounting for approximately 25% of all cases.3 It has an overall incidence rate of 3–7 cases per 100,000 persons per year. The incidence also increases with age (median age 64 years), and the disease appears to be slightly more predominant in men (55% of cases) and Caucasian Americans.4 DLBCL typically presents with rapid nodal enlargement in the neck or abdomen, and systemic “B” symptoms are observed in 30% of patients.5 The extranodal extramedullary disease occurs in up to 40% of the cases, and the gastrointestinal tract is the most common site of involvement. In such cases, the presenting symptoms are abdominal pain, loss of appetite, weight loss, vomiting, and night sweats.6
Among all patients with malignant biliary obstruction, NHL accounts for 1–2% of all cases. Their presentation with obstructive jaundice is mostly secondary to compression of the extrahepatic bile ducts by periportal, perihepatic, or peripancreatic lymphadenopathy, associated tumor lysis, or direct hepatic involvement.1
It is extremely rare for NHL to arise primarily from the extrahepatic bile ducts. As shown below in (Table 1),2; 7; 9; 10; 11; 12; 13; 14; 15; 16; 17; 18; 19; 20; 21; 22; 23; 24; 25; 26; 27; 28; 29; 30; 31; 32; 33 ; 34 a literature review of the period between 1982 and 2012 revealed only 28 cases, with an acute onset of obstructive jaundice being the presenting symptom in most. Of note is that only one case presented with a picture of acute pancreatitis.
| Case | Author | Age (y)/sex | Preliminary diagnosis | Histopathologic diagnosis | Treatment modality | Outcome |
|---|---|---|---|---|---|---|
| 1 | Nguyen2 | 59/male | Sclerosing cholangitis | Lymphohistiocytic lymphoma, diffuse type | Surgery Chemotherapy | Died after 8 mo |
| 2 | Takehara et al11 | 60/male | Non-Hodgkins lymphoma of the extrahepatic duct | Surgery Chemotherapy | Unknown | |
| 3 | Kaplan et al12 | 42/male | Cholangitis | High-grade non-Hodgkins lymphoma | Surgery: Cholecystectomy, segmental resection of the CBD, and hepaticoduodenostomy Chemotherapy using cyclophosphamide, vincristine, etoposide, methotrexate, and cytosine arabinoside | Died after 10 mo |
| 4 | Tartar and Balfe13 | 48/male | Bile duct wall lymphoma | Surgery Chemotherapy | Alive after 14 mo | |
| 5 | Tzanakakis et al14 | 70/male | Mixed small and large cell non-Hodgkins lymphoma | Surgery Chemotherapy | Died after 4 mo | |
| 6 | Kosuge et al15 | 68/female | B cell lymphoma of the CBD | Surgery Chemotherapy Radiotherapy | Died after 16 mo | |
| 7 | Brouland et al16 | 34/female | GB carcinoma vs. sclerosing cholangitis | T cell-rich B cell lymphoma (centroblastic type) of the CBD | Surgery Chemotherapy using MACOP-B | Alive after 48 mo |
| 8 | Machado et al17 | 43/female | Bile duct lymphoma | Surgery Radiotherapy | Alive after 6 mo | |
| 9 | Chiu et al18 | 25/female | Malignant lymphoma of the bile duct | Surgery | Died after 12 mo | |
| 10 | Andre et al19 | 44/female | Klatskin tumor | Non-Hodgkins lymphoma of the extrahepatic duct | Surgery Chemotherapy | Alive after 48 mo |
| 11 | Maymind et al20 | 39/female | Diffuse large B cell lymphoma of the CBD | Surgery Chemotherapy using six courses of CHOP protocol Radiotherapy | Alive after 13 mo | |
| 12 | Podbielski et al21 | 66/male | Klatskin tumor vs. sclerosing cholangitis | Large B cell non-Hodgkins lymphoma | Surgery: En bloc resection of the tumor | Unknown |
| 13 | Oda et al22 | 58/male | Non-Hodgkins lymphoma of the extrahepatic duct | Surgery | Died after 32 d | |
| 14 | Corbinais et al23 | 29/male | High-grade T cell non-Hodgkins lymphoma of the CBD | Chemotherapy using COP plus CHOP protocol | Alive after 12 mo | |
| 15 | Eliason and Grosso24 | 41/male | Klatskin tumor | Diffuse large B cell lymphoma of the extrahepatic ducts | Surgery: CBD excision, Roux-en-Y hepaticojejunostomy, and cholecystectomy | Unknown |
| 16 | Gravel et al25 | 4/male | Sclerosing cholangitis, histiocytosis X or lymphoma | Lymphoblastic lymphoma of the pre-B type of the biliary ducts | Surgery: Exploratory laparotomy, incisional biopsy of the GB, and then cholecystectomy Chemotherapy using methotrexate, vincristine, doxorubicin, and prednisone | Alive after 18 mo |
| 17 | Kang et al26 | 73/female | Pancreatic vs. cholangiocarcinoma | Low-grade B cell lymphoma of MALT type | Surgery: Whipples operation | Alive after 23 mo |
| 18 | Ferluga et al27 | 3/female | Klatskin tumor | Grade II follicular lymphoma of the GB, cystic duct and CBD | Surgery: Resection of GB and CBD followed by hepaticojejunostomy | Alive after 36 mo |
| 19 | Suzuki et al28 | 71/female | Bile duct carcinoma | MALT lymphoma of the CBD | Surgery: Pylorus-preserving pancreaticoduodenectomy | Unknown |
| 20 | Joo et al9 | 21/female | Bile duct cholangiocarcinoma | Diffuse large B cell malignant non-Hodgkins lymphoma | Surgery Chemotherapy using CHOP protocol Radiotherapy using 3060 cGy external irradiation | Alive after 17 mo |
| 21 | Sugawara et al29 | 33/male | Hepatic hilar cholangiocarcinoma | Follicular lymphoma of the extrahepatic duct | Surgery: Extrahepatic duct resection with right and left hepaticojejunostomy | Alive after 12 mo |
| 22 | Shito et al30 | 71/male | Klatskin tumor | MALT lymphoma of the main hepatic duct junction | Surgery: Left hepatic and caudate lobectomy, bile duct resection and LN dissection Chemotherapy using three courses of CHOP protocol | Alive after 45 mo |
| 23 | Dote et al10 | 63/male | Pancreatic head carcinoma or cholangiocarcinoma of the CBD | Diffuse large B cell non-Hodgkins lymphoma of the CBD | Surgery: Subtotal stomach-preserving pancreaticoduodenectomy Chemotherapy using three courses of R-CHOP protocol | Alive after 8 mo |
| 24 | Christophides et al31 | 53/female | Infiltrative cholangiocarcinoma vs. hepatocellular carcinoma | High-grade follicular lymphoma (grade 3A) of the extrahepatic ducts | Surgery: Extended right hepatectomy and Roux-en-Y hepaticojejunostomy Chemotherapy using CHOP-R protocol | Alive after 48 mo |
| 25 | Kang et al32 | 60/male | Klatskin tumor | Diffuse large B cell non-Hodgkins lymphoma of the CHD | Surgery: CHD excision, Roux-en-Y hepaticojejunostomy and LN dissection Chemotherapy: Adjuvant chemotherapy was scheduled | Unknown |
| 26 | Yoon et al7 | 62/male | Cholangiocarcinoma of the bile duct | Marginal zone B cell lymphoma of the MALT type | Surgery: Right hemihepatectomy, bile duct resection and LN resection | Unknown |
| 27 | Luigiano et al33 | 30/male | Acute pancreatitis | Malignant large B cell-type lymphoma of the CBD | Surgery: Resection of the CBD Chemotherapy using CHOP-R protocol | Alive after 6 mo |
| 28 | Khozeimeh et al34 | 32/male | Klatskin tumor | Follicular lymphoma of the bile duct | Surgery: En bloc resection of the bile duct and GB and Roux-en-Y hepaticojejunostomy Chemotherapy using four courses of rituximab (anti-CD20) and galiximab (anti-CD80) | Alive after 72 mo |
| 29 | This study | 57/male | Cholangiocarcinoma of the CBD | High-grade large B cell non-Hodgkins lymphoma of the CBD | Surgery: CBD resection, Roux-en-Y hepaticojejunostomy and LN dissection Chemotherapy using six courses of CVP-R protocol | Alive after 41 mo |
CBD = common bile duct; CHD = common hepatic duct; CHOP = cyclophosphamide, hydroxydaunorubicin, oncovin and prednisone; COP = cyclophosphamide, oncovin and prednisone; CVP-R = cyclophosphamide, vincristine, prednisone, and rituximab; GB = gallbladder; LN = lymph node; MACOP-B = methotrexate, adriamycin, cyclophosphamide, oncovin, prednisone, and bleomycin.
In all cases reviewed, including the one reported above, the clinical presentation, the laboratory investigations, and the results of CT and cholangiography were more consistent with sclerosing cholangitis, Klatskin tumor (cholangiocarcinoma at the hepatic duct bifurcation), or pancreatic carcinoma.
It is very difficult to diagnose primary lymphoma of the extrahepatic bile ducts on the basis of CT scan, magnetic resonance imaging, and cholangiography results. However, Yoon et al7 suggested that despite the paucity of published cases, radiologists should raise the possibility of primary biliary tree lymphoma when cholangiography shows smooth, mild luminal narrowing of the extrahepatic ducts without mucosal irregularities, in spite of the diffuse thickening of the ductal wall on CT/magnetic resonance images.
It is crucial to differentiate primary NHL of the bile ducts from other causes of obstructive jaundice, as the treatment approach and prognosis are fundamentally different. There have been recent reports of success with endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB) in reaching a definitive tissue diagnosis, thus avoiding the surgical interventions that were performed in almost all of the reported cases for lymphomas mistakenly thought to be chemotherapy- or radiotherapy-resistant malignancies.8
In our case, the patients clinical presentation, high level of carbohydrate antigen 19-9, a mid-common bile duct stricture on ERCP, brush cytology suspicious for malignant cells, and a dilated common bile duct on CT scan were consistent with cholangiocarcinoma of the bile duct. It was only upon surgical resection of the tumor and histopathologic as well as immunohistochemical examination of the specimens that a definitive diagnosis of high-grade B cell-type NHL of the common bile duct was made.
DLBCL is an aggressive form of lymphoma, and its primary extranodal involvement of the common bile duct is an extremely rare disease. There is therefore unfortunately no consensus on the best treatment modality to be used. Joo et al9 and Dote et al10 suggest that surgery is important for establishing the diagnosis and removing the lymphoma, and that subsequent chemotherapy and/or radiotherapy after the initial surgery might be effective.
Our case revealed that surgical resection of the tumor for definitive tissue diagnosis followed by a combination of chemotherapy using six cycles of CVP-R, maintain the patient in a complete remission for more than 5 years. However, further follow-up and more studies are required to further elucidate the most appropriate treatment modality.
In conclusion, although primary NHL of the biliary ducts is an extremely rare disease, it should be considered in the differential diagnosis of malignant obstructive jaundice. A tissue biopsy by either EUS-FNAB or surgical intervention showing a characteristic histopathologic and immunohistochemical findings is the gold standard for definitive diagnosis. The best treatment modality is still to be identified, although surgical resection of the tumor followed by chemotherapy and/or radiotherapy is considered an effective option.
References
- 1 J.J. Lokich, R.A. Kane, D.A. Harrison, W.V. McDermott; Biliary tract obstruction secondary to cancer: management guidelines and selected literature review; J Clin Oncol, 5 (1987), pp. 969–981
- 2 G.K. Nguyen; Primary extranodal non-Hodgkins lymphoma of the extrahepatic bile ducts. Report of a case; Cancer, 50 (1982), pp. 2218–2222
- 3 S.H. Swerdlow, E. Campo, N.L. Harris, et al.; World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues; IARC Press, Lyon (2008)
- 4 L.M. Morton, S.S. Wang, S.S. Devesa, et al.; Lymphoma incidence patterns by WHO subtype in the United States, 1992–2001; Blood, 107 (2006), p. 265
- 5 J.O. Armitage, D.D. Weisenburger; New approach to classifying non-Hodgkins lymphomas: clinical features of the major histologic subtypes. Non-Hodgkins Lymphoma Classification Project; J Clin Oncol, 16 (1998), p. 2780
- 6 K.J. Lewin, M. Ranchod, R.F. Dorfman; Lymphomas of the gastrointestinal tract: a study of 117 cases presenting with gastrointestinal disease; Cancer, 42 (1978), pp. 693–707
- 7 M.A. Yoon, J.M. Lee, S.H. Kim, et al.; Primary biliary lymphoma mimicking cholangiocarcinoma: a characteristic feature of discrepant CT and direct cholangiography findings; J Korean Med Sci, 24 (2009), pp. 956–959
- 8 B. Coiffier; State-of-the-art therapeutics: diffuse large B-cell lymphoma; J Clin Oncol, 23 (2005), pp. 6387–6393
- 9 Y.-E. Joo, C.-H. Park, W.-S. Lee; Primary non-Hodgkins lymphoma of the common bile duct presenting as obstructive jaundice; J Gastroenterol, 39 (2004), pp. 692–696
- 10 H. Dote, K. Ohta, R. Nishimura, et al.; Primary extranodal non-Hodgkins lymphoma of the common bile duct manifesting as obstructive jaundice: report of a case; Surg Today, 39 (2009), pp. 448–451
- 11 T. Takehara, H. Matsuda, M. Naitou, et al.; A case report of primary extranodal non-Hodgkins lymphoma of the extrahepatic bile duct; Acta Hepatol Jpn, 88 (1989), pp. 247–252
- 12 L.D. Kaplan, J. Kahn, M. Jacobson, et al.; Primary bile duct lymphoma in the acquired immunodeficiency syndrome (AIDS); Ann Intern Med, 110 (1989), pp. 161–162
- 13 V.M. Tartar, D.M. Balfe; Lymphoma in the wall of the bile ducts: radiologic imaging; Gastrointest Radiol, 15 (1990), pp. 53–57
- 14 G.N. Tzanakakis, M.P. Vezeridis, B.T. Jackson, et al.; Primary extranodal non-Hodgkins lymphoma of the extrahepatic biliary tract; RI Med J, 73 (1990), pp. 483–486
- 15 T. Kosuge, M. Makuuchi, H. Ozaki, et al.; Primary lymphoma of the common bile duct; Hepatogastroenterology, 38 (1991), pp. 235–238
- 16 J.P. Brouland, J. Molimard, J. Nemeth, et al.; Primary T-cell rich B cell lymphoma of the common bile duct; Virchows Arch A Pathol Anat Histopathol, 423 (1993), pp. 513–517
- 17 M.C. Machado, E.E. Abdo, S. Penteado, et al.; Lymphoma of the biliary tract: report of two cases; Rev Hosp Clin Fac Med Sao Paolo, 49 (1994), pp. 64–68
- 18 K.W. Chiu, C.S. Changchien, L. Chen, et al.; Primary malignant lymphoma of common bile duct presenting as acute obstructive jaundice: report of a case; J Clin Gastroenterol, 20 (1995), pp. 259–261
- 19 S.B. Andre, A.Q. Farias, P.L. Bittencourt, et al.; Primary extranodal non-Hodgkins lymphoma of the extrahepatic bile duct mimicking Klatskin tumor; Rev Hosp Clin Fac Med Sao Paolo, 51 (1996), pp. 192–194
- 20 M. Maymind, J.E. Mergelas, D.G. Seibert, et al.; Primary non-Hodgkins lymphoma of the common bile duct; Am J Gastroenterol, 92 (1997), pp. 1543–1546
- 21 F.J. Podbielski, G.F. Pearsall Jr, D.G. Nelson, et al.; Lymphoma of the extrahepatic biliary ducts in acquired immunodeficiency syndrome; Am Surg, 63 (1997), pp. 807–810
- 22 I. Oda, N. Inui, Y. Onodera, et al.; An autopsy case of primary non-Hodgkins lymphoma of the extrahepatic bile duct; Nippon Shokakibyo Gakkai Zasshi (Japanese Journal of Gastroenterology), 96 (1999), pp. 418–422
- 23 S. Corbinais, S. Caulet-Maugendre, M. Pagenault, et al.; Primary T cell lymphoma of the common bile duct; Gastroenterol Clin Biol, 24 (2000), pp. 843–847
- 24 S.C. Eliason, L.E. Grosso; Primary biliary lymphoma clinically mimicking cholangiocarcinoma: a case report and review of the literature; Ann Diagn Pathol, 5 (2001), pp. 25–33
- 25 J. Gravel, M. Lallier, L. Garel, et al.; Primary non-Hodgkin lymphoma of the extrahepatic biliary tract and gallbladder in a child; J Pediatr Gastroenterol Nutr, 32 (2001), pp. 598–601
- 26 C.S. Kang, Y.S. Lee, S.M. Kim, B.K. Kim; Primary low-grade B cell lymphoma of mucosa-associated lymphoid tissue type of the common bile duct; J Gastroenterol Hepatol, 16 (2001), pp. 949–951
- 27 D. Ferluga, B. Luzar, E. Gadzijev; Follicular lymphoma of the gallbladder and extrahepatic bile ducts; Virchows Arch, 442 (2003), pp. 136–140
- 28 S. Suzuki, S. Tanaka, M. Suzuki, et al.; Mucosa-associated lymphoid tissue-type lymphoproliferative lesion of the common bile duct; Hepatogastroenterology, 51 (2004), pp. 110–113
- 29 G. Sugawara, M. Nagino, K. Oda, H. Nishio, T. Ebata, M. Nimura; Follicular Lymphoma of the extrahepatic bile duct mimicking cholangiocarcinoma; J Hepatobiliary Pancreat Surg, 15 (2008), pp. 196–199
- 30 M. Shito, T. Kakefuda, T. Omori, S. Ishii, H. Sugiura; Primary non-Hodgkins lymphoma of the main hepatic duct junction; J Hepatobiliary Pancreat Surg, 15 (2008), pp. 440–443
- 31 T. Christophides, B. Samstein, J. Emond, G. Bhagat; Primary follicular lymphoma of the extrahepatic bile duct mimicking a hilar cholangiocarcinoma: a case report and review of the literature; Hum Pathol, 30 (2009), pp. 1808–1812
- 32 H.G. Kang, J.S. Choi, J.A. Seo, et al.; A case of primary biliary malignant lymphoma mimicking Klatskin tumor; Korean J Gastroenterol, 54 (2009), pp. 191–195
- 33 C. Luigiano, F. Ferrara, C. Fabbri, et al.; Primary lymphoma of the common bile duct presenting with acute pancreatitis and cholangitis; Endoscopy, 42 (2010), pp. E265–E266
- 34 N. Khozeimeh, T. Bhatti, T.A. Ponsky, B.D. Cheson, F. Brody, P.P. Lin; Primary non-Hodgkins lymphoma of the extrahepatic bile duct; J Gastrointest Cancer, 43 (2012), pp. S46–S49
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?