Abstract
Objectives
The main objective of this study was to assess the blood flow rate and velocity in coronary artery stenosis using intracoronary frequency domain optical coherence tomography (FD-OCT). A correlation between fractional flow reserve (FFR) and FD-OCT derived blood flow velocity is also included in this study.
Methods & results
A total of 20 coronary stenoses in 15 patients were assessed consecutively by quantitative coronary angiography (QCA), FFR and FD-OCT. A percutaneous coronary intervention (PCI) optimization system was used in this study which combines wireless FFR measurement and FD-OCT imaging in one platform. Stenoses were labelled severe if FFR ≤ 0.8. Blood flow rate and velocity in each stenosis segment were derived from the volumetric analysis of the FD-OCT pull back images. The FFR value was ≤ 0.80 in 5 stenoses (25%). The mean blood flow rate in severe coronary stenosis (n = 5) was 2.54 ± 0.55 ml/s as compared to 4.81 ± 1.95 ml/s in stenosis with FFR > 0.8 (n = 15). A good and significant correlation between FFR and FD-OCT blood flow velocity in coronary artery stenosis (r = 0.74, p < 0.001) was found.
Conclusion
The assessment of stenosis severity using FD-OCT derived blood flow rate and velocity has the ability to overcome many limitations of QCA and intravascular ultrasound (IVUS).
Keywords
Intracoronary optical coherence tomography (IOCT);Blood flow rate;Blood flow velocity;Fractional flow reserve (FFR);Coronary lesions
1. Introduction
Quantitative coronary angiography (QCA) has been used for the assessment of coronary artery disease (CAD) for many years and it is still the most common technique for the estimation of lumen diameter stenosis (DS). The evaluation of intermediate coronary stenosis, having luminal narrowing with %DS of 40% to 70% on angiography, via QCA is inaccurate [1]; [2] ; [3]. Therefore different diagnostic modalities are used to define the severity of such stenosis. In this regard, functional assessment of coronary stenosis by pressure derived fractional flow reserve (FFR) is considered as gold standard [4]; [5]; [6] ; [7].
Intracoronary optical coherence tomography (IOCT) is a high resolution optical imaging technology used for anatomical and morphological assessment of coronary stenosis [8]; [9] ; [10]. IOCT is similar to intravascular ultrasound (IVUS) but uses near-infrared (NIR) light rather than sound waves to create in vivo images of coronary arteries and deployed stents. The higher resolution of IOCT as compared to IVUS (10 times higher than IVUS) allows measurements of lumen dimensions with excellent reproducibility [11]; [12] ; [13]. Recently intracoronary frequency domain optical coherence tomography (FD-OCT) has been introduced to overcome many technical limitations of the time domain OCT (TD-OCT). FD-OCT systems enable in vivo imaging of coronary vessel wall with an axial resolution up to 15 μm and a lateral resolution up to 25 μm with high frame rates (100 frames/s) and pull back speeds (20 mm/s) [14].
The primary objective of this study was to assess the blood flow rate and velocity in coronary artery stenosis, calculated through the volumetric analysis of FD-OCT pull back images of the vessel segments, and investigate the relationship between FD-OCT derived these measurements and FFR.
2. Materials & methods
20 coronary stenoses were studied in 15 patients planned for coronary angiography due to stable angina and/or ischemia documented on exercise stress test. QCA analysis, FD-OCT imaging and FFR measurement were performed in all patients. The study was approved by Galway clinical research ethics committee and the written informed consent for all procedures was obtained from each patient. All patients had at least one target vessel with single de novo stenosis with %DS > 30% by visual estimation. Patients with an additional stenosis in second coronary artery were also included in the study if the other inclusion criteria were fulfilled. Patients having multiple stenoses in target vessel, left main stenosis, bypass graft stenosis and acute myocardial infarction were excluded from the study.
QCA was performed after intracoronary administration of nitrates (0.1 mg) according to standard procedures [1] ; [2]. A validated QCA software (CASS II, Pie Medical Imaging, BV, Maastricht, Netherlands) was employed for the estimation of reference vessel diameter (RVD), %DS, percent area stenosis (%AS), lesion length (LL) and minimum lumen diameter (MLD).
FFR measurement was performed using Pressure Wire™ Aeris (St. Jude Medical, San Diego, California), a wireless tool to measure FFR in coronary artery stenosis. Maximal hyperaemia was induced by intravenous adenosine managed at 140 μg/kg/min. A wireless device Wi-Box™ was used to receive aortic pressure readings wirelessly. FFR was calculated as the ratio of intracoronary pressure to the aortic pressure during hyperaemia. Stenoses were considered severe if FFR ≤ 0.80 [2].
For OCT imaging of the stenosis we used commercially available FD-OCT C7-XR™ system and the Dragonfly catheter (St. Jude Medical, Light lab Imaging Inc., Westford, Massachusetts). The automated pullback was performed at 0.2 cm/s and the blood removal was achieved by injecting iso-osmolar contrast at 37 °C through the guiding catheter.
FD-OCT measurements were performed using Lightlab imaging software. The minimum lumen area (MLA) and MLD were measured at the frame with smallest intraluminal area. The proximal reference lumen area and diameter were measured at the frame with largest intraluminal area proximal to the stenosis. Similarly, distal reference lumen area and diameter was measured at the frame with largest intraluminal area distal to the stenosis.
The assessment of the blood flow rate and velocity in coronary artery stenosis is based on a model of blood flow resistances [15] which consists of a series combination (Rt) of the blood flow resistance of the stenosis, microvascular resistance under maximal hyperaemia and the blood flow resistance of the length of vessel outside the FD-OCT imaged segment. In this model the blood flow driven by the difference between the arterial pressure (Pa) and the coronary venous pressure (Pv) is limited by the total flow resistance Rt (series combination) of the branch.
Microvascular resistance was calculated by dividing hyperaemic microvascular resistance index (h-MRv) to the proximal reference lumen area. h-MRv was set equal to the minimum value measured by Doppler flowmetry in previous studies (100 mm Hg·s− 1/cm3) [16]. Blood flow resistance of the vessel outside FD-OCT imaged segment was calculated using Poiseuilles law assuming that the entire vessel had a fixed length of 8 cm and a cross-sectional area equal to the average of the proximal and distal reference lumen areas. Stenosis resistance, which consists of a flow independent component that results from viscous losses and a flow dependent component that results from kinetic losses, was calculated using analytical method developed by Gould et al. [17] and Kirkeeide [18]. Blood flow rate was calculated by dividing Pa − Pv (assuming 90 mm Hg) to Rt. Blood flow velocity in coronary artery stenosis was calculated by dividing blood flow rate to the minimum lumen area of the stenosis. A relationship between FFR and FD-OCT derived blood flow velocity in coronary artery stenosis was determined using linear regression analysis. A p value of < 0.05 was considered as significant.
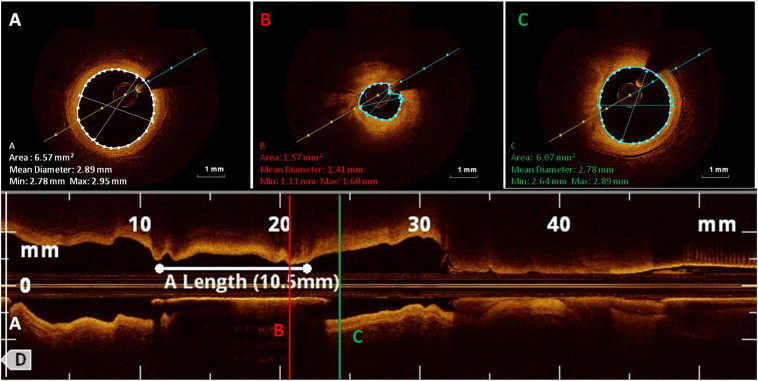
Fig. 1 shows intracoronary FD-OCT B-scans (cross-sectional images) of the vessel wall with calculated lumen measurements at different locations; reference frame proximal to stenosis with largest intraluminal area, frame with minimum intraluminal area and reference frame distal to stenosis with largest intraluminal area. The figure also shows longitudinal reconstruction of the artery showing the locations of FD-OCT B-scans.
|
|
|
Fig. 1. FD-OCT B-scans (cross-sectional images) of the vessel wall with calculated lumen measurements and longitudinal reconstruction of the artery showing the locations of FD-OCT B-scans. (A) Reference frame proximal to stenosis with largest intraluminal area. (B) Frame with minimum intraluminal area. (C) Reference frame distal to stenosis with largest intraluminal area. |
3. Results
20 coronary stenoses in 15 patients were analysed with QCA, FFR and FD-OCT. The patients' data and stenosis characteristics obtained through QCA are presented in Table 1. The mean age of the patients was 63 ± 13 years. 11 patients (73%) were male. 12 patients (80%) had hypertension and 6 (40%) had diabetes mellitus. The left anterior descending artery (LAD) was the most common studied vessel with 12 stenoses (60%). The mean reference vessel diameter (RVD), lesion length (LL), MLD, %DS and %AS by QCA were 2.15 ± 0.58 mm, 8 ± 4.37 mm, 1.27 ± 0.48 mm, 44.8 ± 12.2% and 68 ± 13.6% respectively. The FFR value was ≤ 0.80 in 5 stenoses (25%). The mean MLA, MLD and %AS by FD-OCT were 2.39 ± 1.15 mm2, 1.36 ± 0.39 mm and 63.4 ± 12.8% respectively. The differences in FD-OCT measurements between stenosis with FFR ≤ 0.80 (n = 5) and those with FFR > 0.80 (n = 15) are presented in Table 2. The mean blood flow rate in severe coronary stenosis (n = 5) was 2.54 ± 0.55 ml/s as compared to 4.81 ± 1.95 ml/s in stenosis with FFR > 0.8 (n = 15).
| Patients' data (n = 15) | |
| Age, years | 63 ± 13 |
| Male, n (%) | 11 (73) |
| HTN, n (%) | 12 (80) |
| DM, n (%) | 6 (40) |
| Smoking, n (%) | 7 (47) |
| Dyslipidemia, n (%) | 13 (87) |
| Family history of coronary disease, n (%) | 8 (53) |
| Clinical presentation, n (%) | |
| Stable angina | 10 (67) |
| Unstable angina | 1 (6) |
| Atypical/asymptomatic | 4 (27) |
| Stenosis characteristics (n = 20) | |
| Stenosis location, n (%) | |
| LAD | 12 (60) |
| RCA | 3 (15) |
| LCX | 3 (15) |
| OM1 | 1 (5) |
| Ramus intermedius | 1 (5) |
| QCA parameters (n = 20) | |
| Reference vessel diameter (mm) | 2.15 ± 0.58 |
| Lesion length (mm) | 8 ± 4.37 |
| Minimal lumen diameter (mm) | 1.27 ± 0.48 |
| Diameter stenosis, % | 44.8 ± 12.2 |
| Area stenosis, % | 68 ± 13.6 |
HTN = hypertension; DM = diabetes mellitus; LAD = left anterior descending artery; RCA = right coronary artery; LCX = left circumflex coronary artery; OM1 = first obtuse marginal artery; D1 = first diagonal artery; QCA = quantitative coronary angiography.
| FFR ≤ 0.80 (n = 5) | FFR > 0.80 (n = 15) | p value | |
|---|---|---|---|
| Minimal lumen area (MLA), mm2 | 1.15 ± 0.25 | 2.8 ± 1.03 | 0.001 |
| Minimal lumen diameter (MLD), mm | 0.91 ± 0.11 | 1.50 ± 0.33 | < 0.001 |
| Proximal reference lumen area, mm2 | 4.15 ± 0.52 | 6.42 ± 2.48 | 0.03 |
| Proximal reference lumen diameter, mm | 2.29 ± 0.14 | 2.78 ± 0.52 | 0.03 |
| Distal reference lumen area, mm2 | 10.64 ± 6.4 | 12.28 ± 4.67 | 0.27 |
| Distal reference lumen diameter, mm | 3.53 ± 1.12 | 3.86 ± 0.81 | 0.27 |
| Percent area stenosis (%AS), % | 70.2 ± 4.6 | 61.2 ± 13.9 | 0.08 |
| Stenosis resistance (Rs), mm Hg cm− 3.s | 12.3 ± 5.2 | 3.54 ± 2.49 | < 0.001 |
| Blood flow rate (Q), ml/s | 2.54 ± 0.55 | 4.81 ± 1.95 | 0.01 |
| Blood flow velocity, cm/s | 2.23 ± 0.23 | 1.73 ± 0.26 | < 0.001 |
FD-OCT = frequency domain optical coherence tomography.
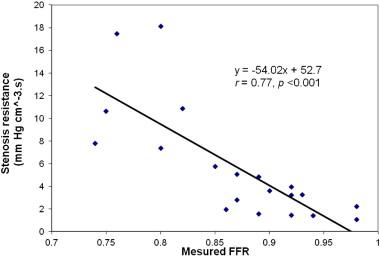
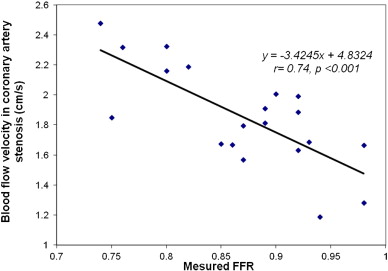
Fig. 2 shows the linear regression analysis for FFR and FD-OCT derived stenosis resistance. There was a good and significant correlation between FFR and FD-OCT derived stenosis resistance (r = 0.77, p < 0.001). Fig. 3 shows the linear regression analysis for FFR and FD-OCT derived blood flow velocity in coronary artery stenosis. There was a good and significant correlation between FFR and FD-OCT derived blood flow velocity (r = 0.74, p < 0.001).
|
|
|
Fig. 2. Correlation between FFR and FD-OCT derived stenosis resistance. |
|
|
|
Fig. 3. Correlation between FFR and FD-OCT derived blood flow velocity in coronary artery stenosis. |
4. Discussion
The major findings of the present study are that there is a good and significant correlation between FFR and FD-OCT derived blood flow velocity in coronary artery stenosis, a measure of stenosis severity calculated from the volumetric analysis of the vessel segments imaged by FD-OCT.
Gregory T. Stefano et al determined the correlation between FFR and the FD-OCT measured anatomical parameters in their study performed on 14 patients with 18 stenoses [19]. They found no significant correlation between FFR and FD-OCT measured lumen dimensions MLA (r = 0.167, p = 0.56), MLD (r = − 0.42, p = 0.13) and %AS (r = 0.29, p = 0.29). FD-OCT derived volumetric blood flow measurements, stenosis resistance and blood flow velocity, correlate more closely with FFR than the OCT measured anatomical parameters MLD, MLA and %AS. Blood flow measurements presented in this study were derived from the volumetric measurement of the lumen profile with FD-OCT, on the other hand anatomical parameters MLD, MLA and %AS were derived from single image cross-sections. The combination of excellent lumen measurement capability of FD-OCT and blood flow resistances model, that also take into account microvascular resistance and volume integrated pressure losses, improves the predictive ability of FD-OCT derived blood flow measurements as compared to intraluminal parameters; MLA, MLD and %AS.
FD-OCT has better diagnostic efficiency than IVUS in identifying severe coronary stenosis (FFR ≤ 0.80) [11]; [12] ; [13]. Recently we evaluated the diagnostic efficiency of FD-OCT derived intraluminal dimensions (MLA, MLD and %AS) in identifying haemodynamically severe coronary stenoses in 30 patients with 41 stenoses [20]. In the overall group, we demonstrated a moderate diagnostic efficiency with FD-OCT derived intraluminal parameters (area under the curve (AUC): 0.80 for MLA and AUC: 76 for MLD). We also demonstrated a high diagnostic efficiency in identifying severe coronary stenosis in vessels having reference diameter of < 3 mm (AUC: 0.96 for MLA).
We used ILUMEIN (St. Jude) percutaneous coronary intervention (PCI) optimization system in the present study. This system is the integrated technology that combines wireless FFR and FD-OCT imaging in one platform which provides advanced physiological and anatomical information with precise measurements of stenosis dimensions, vessel size and structure to improve the diagnosis and treatment of CAD. FD-OCT imaging is a non occlusion technique which performs measurements without the requirement of balloon inflation. TD-OCT (occlusive OCT technique) has been proven to miscalculate the intraluminal dimensions during balloon inflation [21].
The results presented in this study included a small sample size so further studies are suggested to confirm these results. We included stenoses in the major coronary arteries (LAD, RCA, LCX etc.) but the calculation methodologies for estimating the blood flow rate and velocity in coronary artery stenosis may not hold in all locations. The evaluation of severe coronary stenosis based on FD-OCT derived these blood flow measurements can overcome many limitations of the QCA and IVUS but these measurements do not take into account the variations in myocardium mass. The number of stenoses presented in this study were small so without further validation and development FD-OCT derived blood flow measurements introduced in this study should not be considered as substitute or compliment to FFR in interventional procedural planning and decision making.
5. Conclusions
In this study, the blood flow rate and velocity in coronary artery stenosis were derived using FD-OCT and validated against FFR. We found a good and significant correlation between FFR and FD-OCT derived blood flow velocity in coronary artery stenosis. The assessment of coronary artery stenosis severity based on FD-OCT derived these blood flow measurements can overcome many limitations of the QCA and IVUS and have the potential to become a helpful tool in the assessment of CAD.
Conflict of interest
We declare that there is no conflict of interest for any author.
Acknowledgements
We thank the Health Service Executive Ireland (provides all of Irelands public health services, in hospitals and communities across the country). Haroon Zafar is supported by a Hardiman Fellowship from NUI Galway.
References
- [1] N.H. Pijls, W.F. Fearon, P.A. Tonino, U. Siebert, F. Ikeno, B. Bornschein, et al.; Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study; J Am Coll Cardiol, 56 (3) (2010), pp. 177–184
- [2] P.A. Tonino, B. De Bruyne, N.H. Pijls, U. Siebert, F. Ikeno, M. van' t Veer, et al.; Fractional flow reserve versus angiography for guiding percutaneous coronary intervention; N Engl J Med, 360 (3) (2009), pp. 213–224
- [3] C.W. White, C.B. Wright, D.B. Doty, L.F. Hiratza, C.L. Eastham, D.G. Harrison, et al.; Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis?; N Engl J Med, 310 (13) (1984), pp. 819–824
- [4] B. De Bruyne, N.H. Pijls, J. Bartunek, K. Kulecki, J.W. Bech, H. De Winter, et al.; Fractional flow reserve in patients with prior myocardial infarction; Circulation, 104 (2) (2001), pp. 157–162
- [5] N.H. Pijls, B. Van Gelder, P. Van der Voort, K. Peels, F.A. Bracke, H.J. Bonnier, et al.; Fractional flow reserve: a useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow; Circulation, 92 (11) (1995), pp. 3183–3193
- [6] N.H. Pijls, B. De Bruyne, K. Peels, P.H. Van Der Voort, H.J. Bonnier, J. Bartunek, et al.; Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenosis; N Engl J Med, 334 (26) (1996), pp. 1703–1708
- [7] N.H. Pijls, P. van Schaardenburgh, G. Manoharan, E. Boersma, J.W. Bech, M. van't Veer, et al.; Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER study; J Am Coll Cardiol, 49 (21) (2007), pp. 2105–2111
- [8] N. Gonzalo, P.W. Serruys, E. Regar; Optical coherence tomography: clinical applications and the evaluation of DES; Minerva Cardioangiol, 56 (5) (2008), pp. 511–525
- [9] N. Gonzalo, H.M. Garcia-Garcia, P.W. Serruys, K.H. Commissaris, H. Bezerra, P. Gobbens, et al.; Reproducibility of quantitative optical coherence tomography for stent analysis; EuroIntervention, 5 (2) (2009), pp. 224–232
- [10] N. Gonzalo, H.M. Garcia-Garcia, E. Regar, P. Barlis, J. Wentzel, Y. Onuma, et al.; In vivo assessment of high-risk coronary plaques at bifurcations with combined intravascular ultrasound and optical coherence tomography; JACC Cardiovasc Imaging, 2 (4) (2009), pp. 473–482
- [11] G. Guagliumi, G. Musumeci, V. Sirbu, H.G. Bezerra, N. Suzuki, L. Fiocca, et al.; Optical coherence tomography assessment of in vivo vascular response after implantation of overlapping bare-metal and drug-eluting stents; JACC Cardiovasc Interv, 3 (5) (2010), pp. 531–539
- [12] N. Gonzalo, G.J. Tearney, P.W. Serruys, G. van Soest, T. Okamura, H.M. García-García, et al.; Second-generation optical coherence tomography in clinical practice. High-speed data acquisition is highly reproducible in patients undergoing percutaneous coronary intervention; Rev Esp Cardiol, 63 (8) (2010), pp. 893–903
- [13] T. Okamura, N. Gonzalo, J.L. Gutiérrez-Chico, P.W. Serruys, N. Bruining, S. de Winter, et al.; Reproducibility of coronary Fourier domain optical coherence tomography: quantitative analysis of in vivo stented coronary arteries using three different software packages; EuroIntervention, 6 (3) (2010), pp. 371–379
- [14] Giuseppe Ferrante, Patrizia Presbitero, Robert Whitbourn, Peter Barlis; Current applications of optical coherence tomography for coronary intervention; Int J Cardiol, 165 (1) (2013), pp. 7–16
- [15] Schmitt JM, Friedman JM, Petroff C, Elbasiony A. Lumen morphology and vascular resistance measurements data collection systems, apparatus, and methods. US Patent 2011; Application No. 0071404.
- [16] Y.F. Zhou, G.S. Kassab, S. Molloi; On the design of the coronary arterial tree: a generalization of Murrays Law; Phys Med Biol, 44 (1999), pp. 2929–2945
- [17] K.L. Gould, K.O. Kelley, E.L. Bolson; Experimental validation of quantitative coronary arteriography for determining pressure-flow characteristics of coronary stenosis; Circulation, 66 (1982), pp. 930–937
- [18] R.L. Kirkeeide; Coronary obstructions, morphology, and physiological significance; J.H.C. Reiber, P.W. Serruys (Eds.), Quantitative coronary arteriography, Kluwer Academic Publishers, The Netherlands (1991), pp. 229–244
- [19] G.T. Stefano, H.G. Bezerra, G. Attizzani, D. Chamié, E. Mehanna, H. Yamamoto, et al.; Utilization of frequency domain optical coherence tomography and fractional flow reserve to assess intermediate coronary artery stenosis: conciliating anatomic and physiologic information; Int J Cardiovasc Imaging, 27 (2011), pp. 299–308
- [20] Haroon Zafar, Ihsan Ullah, Kate Dinneen, Sajjad Matiullah, Alan Hanley, Martin J. Leahy, et al.; Evaluation of hemodynamically severe coronary stenosis as determined by fractional flow reserve with frequency domain optical coherence tomography measured anatomical parameters; J Cardiol, 64 (1) (2014), pp. 19–24
- [21] N. Gonzalo, P.W. Serruys, H.M. García-García, G. Van Soest, T. Okamura, J. Ligthart, et al.; Quantitative ex vivo and in vivo comparison of lumen dimensions measured by optical coherence tomography and intravascular ultrasound in human coronary arteries; Rev Esp Cardiol, 62 (2009), pp. 615–624
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?