Question
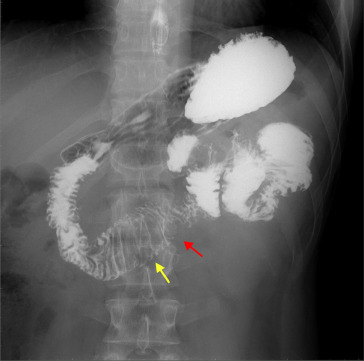
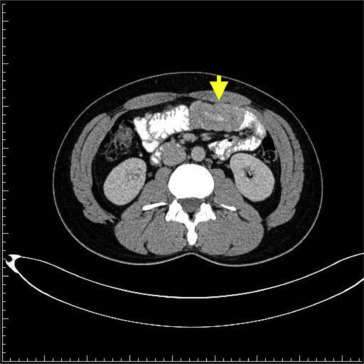
A 28-year-old man without any underlying disease presented with dizziness and general malaise for 6 months. He came to the clinic for help initially. Vital signs and physical examination were normal. Blood tests revealed only the following abnormality: hemoglobin 8.6 g/dL. His fecal occult blood test result was positive. Esophagogastroduodenoscopy and colonoscopy showed nonspecific findings. Ferrous sulfate was prescribed for suspected iron-deficiency anemia. Owing to refractory anemia, he was transferred to our hospital for further evaluation. Small bowel series showed a jejunal polypoid lesion with increasing folds and lumen dilatation in the jejunum (Fig. 1 ). Computed tomography of abdomen and pelvis showed soft tissue mass (4.8 cm × 2.5 cm) within a proximal jejunal loop and intussusception of jejunal loops (Fig. 2 , yellow arrow). This patient received surgical resection. A long-stalk mass (about 4 cm in size) at the proximal jejunum, 25 cm distal to the Treit'z ligament (Fig. 3 ), was found during the operation, and this tumor caused intussusception of the jejunum. After surgery, his anemia improved gradually and he was well until recently.
|
|
|
Figure 1. Jejunal polypoid lesion (red arrow) with increasing folds and lumen dilatation (yellow arrow). |
|
|
|
Figure 2. Intussusception of jejunal loops (yellow arrow). |
|
|
|
Figure 3. Long-stalk mass at proximal jejunum. |
What is this mans unifying diagnosis?
- Intestinal polypoid adenoma or villous adenoma
- Intestinal carcinoid tumor
- Intestinal lymphoma
- Peutz–Jeghers polyposis (PJP) or Peutz–Jeghers syndrome (PJS)
Answer
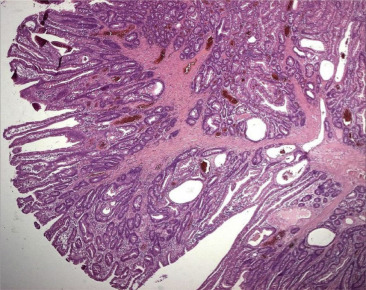
On histopathology, this polypoid lesion shows a hamartomatous intestinal polyposis with the distinct feature of an arborizing framework of smooth muscle within the muscularis mucosae (Fig. 4 ), a typical finding of the polyp of PJS. Owing to the absence of involved family members of the PJS patient, a lack of mucocutaneous pigmentation, and the presence of a solitary polyp with the characteristic histopathologic appearance of PJS, solitary or sporadic PJP is identified [1] .
|
|
|
Figure 4. Arborizing framework of smooth muscle within the muscularis mucosae. |
PJP usually occurs in the context of PJS, and a recent case series doubted whether sporadic PJP exists or is incomplete or is the initial form of PJS [2] . One case series revealed that frequent abdominal complications of PJS included gastrointestinal hemorrhage (78.6%) and intussusception (64.3%) [3] . Another case series showed that the most frequent complication of PJS in younger patients is intussusception (reported in nearly half of the patients), primarily involving the small intestine [4] . Our patient had gastrointestinal bleeding and jejunal intussusception, consistent with complications, which resulted from PJS (or PJP). This patient has been asymptomatic since surgery.
Two small studies investigated the correlation between solitary or sporadic PJP and cumulative lifetime risk of cancer, but drew different conclusions. Oncel et al [5] recruited eight cases with solitary PJP, and this study demonstrated no additional bowel polyps and no malignancy after polypectomy and 11.5 years of median follow-up (range 3–22 years). Burkart et al [2] reviewed eight cases with sporadic PJP and suggested that individuals with single PJP may have a cumulative lifetime risk of cancer similar to those with the syndrome.
Therefore, the lifetime risk of cancer in solitary or sporadic PJP is not yet well known, and the need for surveillance endoscopy to look for polyp recurrence after polypectomy has also not been established. An initial screening colonoscopy and small-bowel studies, such as small-bowel series, balloon enteroscopy, or capsule enteroscopy, are usually performed when a Peutz–Jeghers polyp has been histologically classified, to look for other polyps in the bowel, but the need for specific high-risk screening is still under investigation.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] B. Acea Nebril, L. Taboada Filgueira, A. Parajó Calvo, R. Gayoso García, D. Gómez Rodríguez, F. Sánchez González, et al.; Solitary hamartomatous duodenal polyp, a different entity: report of a case and review of the literature; Surg Today, 23 (1993), pp. 1074–1077
- [2] A.L. Burkart, T. Sheridan, M. Lewin, H. Fenton, N.J. Ali, E. Montgomery; Do sporadic Peutz–Jeghers polyps exist? Experience of a large teaching hospital; Am J Surg Pathol, 31 (2007), pp. 1209–1214
- [3] M.T. Weng, Y.H. Ni, Y.N. Su, J.M. Wong, S.C. Wei; Clinical and genetic analysis of Peutz–Jeghers syndrome patients in Taiwan; J Formos Med Assoc, 109 (2010), pp. 354–361
- [4] F.M. Giardiello, J.D. Trimbath; Peutz–Jeghers syndrome and management recommendations; Clin Gastroenterol Hepatol, 4 (2006), pp. 408–415
- [5] M. Oncel, F.H. Remzi, J.M. Church, J.R. Goldblum, M. Zutshi, V.W. Fazio; Courses and follow-up of solitary Peutz–Jeghers polyps: a case series; Int J Colorectal Dis, 18 (2003), pp. 33–35
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?