Abstract
Background
AL amyloidosis and multiple myeloma result in extracellular deposition of insoluble fibrillary protein in tissue and organs. Untreated median survival is very poor, and even worse with cardiac involvement. Chemotherapy and peripheral blood stem cell transplantation (PBSCT) have been shown to dramatically improve survival, with hematologic remission documented. Regression of cardiac changes has previously been shown, as assessed by echocardiography (TTE) and cardiac magnetic resonance imaging (CMR). This study is a comparison of TTE and CMR in long-term survivors of cardiac amyloidosis with regression.
Results
Four long-term survivors with cardiac amyloidosis and regression of cardiac features on TTE were identified. Mean age was 60 years and average survival was 139 months from the time of diagnosis of cardiac involvement. Statistically significant regression of the cardiac features of cardiac amyloidosis were demonstrated on TTE. In these survivors, post-PBSCT structural assessments were similar between TTE and CMR. Classical strain imaging features of cardiac amyloidosis were only present in 50%. All patients had diffuse, patchy gadolinium enhancement on CMR after PBSCT.
Conclusions
Treatment of cardiac amyloidosis with chemotherapy and PBSCT may result in regression of abnormalities on TTE with marked improvement in survival. Post treatment, TTE and CMR structural assessments appear similar. Gadolinium imaging suggests that microscopic residual infiltration persists despite macroscopic regression. Significant cardiac improvements with prolonged survival are seen nonetheless. Multimodality imaging has a vital role in the management of cardiac amyloidosis.
Keywords
Cardiac amyloidosis;Echocardiography;Cardiac magnetic resonance imaging;Regression;Treatment;Survival
1. Introduction
The systemic amyloidoses are rare diseases which result in production of insoluble proteins. Abnormal insoluble fibrils may be laid down in tissue and organs. These aberrant molecular deposits are often toxic and result in significant end-organ damage [1]; [2]; [3]; [4] ; [5]. Diseases in this spectrum include AL (primary) amyloidosis, multiple myeloma, monoclonal gammopathy of unknown significance (MGUS), and AA (secondary) amyloid [1]; [2]; [3]; [4] ; [5]. Before the 1990s, AL amyloidosis and multiple myeloma were shown to have a median survival from diagnosis of 12 months [1]. With the development of infiltrative cardiomyopathy (i.e. cardiac amyloidosis), survival was reduced to 5 months [1]. Early chemotherapy regimens did not significantly alter survival [5]. From the 1990s, some centres began to investigate high-dose chemotherapy, followed by peripheral blood stem cell transplantation (PBSCT). This therapy and more recent anti-plasma cell agents have resulted in sustained and deep hematologic remission in many patients, with dramatic improvement in survival [4]; [5]; [6]; [7] ; [8].
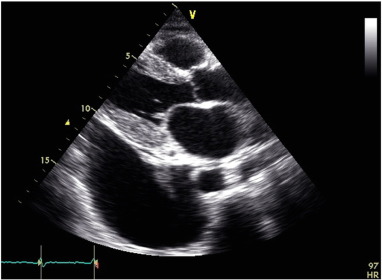
Cardiac amyloidosis results in characteristic changes on echocardiography (see Fig. B.1) [9]; [10]; [11] ; [12]. These include thickened, speckled ventricular walls (left and right ventricle), small ventricular cavities, dilated atria, thickening of valve leaflet tissue, small pericardial effusions, and advanced diastolic dysfunction. Global longitudinal strain as a more subtle measure of ventricular function may show early changes. Apical sparing strain patterns are thought to be pathognomonic in cardiac amyloidosis [9]; [10]; [11]; [12] ; [13]. Cardiac magnetic resonance imaging (CMR) demonstrates diffuse circumferential subendocardial, mid-wall to transmural enhancement in a non-vascular distribution in the acute phases of the disease [14]; [15]; [16] ; [17]. These changes make CMR an excellent tool for the detection of cardiac amyloidosis with high sensitivity and specificity [14]; [15]; [16] ; [17].
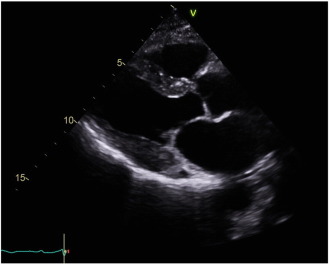
We have previously reported that with hematologic remission after PBSCT, some patients with cardiac amyloidosis had regression of the cardiac anatomical and functional manifestations, as assessed by echocardiography (see Fig. B.2) [18]. There are case reports and series in the literature suggesting that regression of CMR changes occur also, with faint residual enhancement described following stem cell treatment [19]; [20]; [21] ; [22]. Until recently, CMR had not been a routine component of our cardiac amyloidosis work-up, due to a lack of funding in the Australian private health care system. The diagnosis of cardiac amyloid does not require the use of CMR [23] but is certainly enhanced by this use of this technique [14]; [15]; [16] ; [17].
2. Methods
This study included a retrospective review of the ICON Cancer Care amyloidosis and myeloma database and the HeartCare Partners echocardiography database. All patients with amyloidosis or multiple myeloma who had had a PBSCT from 1998 to 2016 were reviewed. Patients with myeloma and AL amyloidosis were included as the effects on the heart and the treatment regimens are similar.
2.1. Echocardiographic methods
The echocardiogram and electrocardiograph (ECG) studies for these patients were assessed for the typical hallmarks of cardiac amyloidosis (thick, speckled walls, advanced diastolic dysfunction, dilated atria, and/or small pericardial effusions, and low voltages on ECG) [9]; [10]; [11] ; [12]. Global longitudinal strain and strain patterns were also recorded. Measurements were taken at the time of the echocardiogram, using the live images. The interventricular septum and posterior wall thicknesses (segments 2 and 5 in the 17-segment model) were calculated using the two-dimensional images in the parasternal long axis, at end diastole, based on mitral valve motion. Diastolic function grade and left atrial area and volume were assessed and recorded. Diastolic function was assessed using mitral inflow, pulmonary vein Doppler, and Doppler Tissue Imaging, and then graded from normal function to grade 3 diastolic dysfunction (restrictive pattern) [9]; [10]; [11] ; [12]. Left atrial areas and volumes were measured at end-systole (the largest dimension or the end of the T wave) from the apical 4-chamber and apical 2-chamber views. The left atrial outlines at both end-systole and end-diastole were traced and then averaged.
All of the echocardiograms were read by cardiologists with subspecialty training in echocardiography. Echocardiograms were recorded before PBSCT and typically at 6-month intervals after PBSCT. Time in months from diagnosis of cardiac amyloidosis to death was recorded, for all patients who had died. For survivors, the time in months was recorded from diagnosis to the date when the data points were collated. Initial images were recorded on a variety of echocardiography machines, including the General Electric e9, Vivid 7 and Vivid 3, Phillips Epic and ie33, Siemens SC2000, and Acuson Sequoia. Echocardiograms were repeated on the day of the CMR for direct comparison. All of these were done on a General Electric e9 machine, with strain capability. Strain imaging was only performed on scans done in the last 5 years.
2.2. CMR methods
Cardiac magnetic resonance imaging was performed to supplement echocardiographic findings due to its unique ability to define myocardial infiltration and enhancement. A 3T MRI scanner (Skyra, Siemens, Erlangen Germany) was used to acquire Cine short axis and axial views of the whole heart with additional 2-chamber, 3-chamber, and 4-chamber views. Functional parameters where acquired by means of ARGUS analytical Software (Siemens, Germany) with ejection fraction and volumes calculated for each ventricle and for the left atrium. Thickness of the left ventricle wall was measured in end-diastole in short axis view using the 17-segment model. Right ventricle and atrial septal wall thickness was measured in 4-chamber view. Post contrast imaging was obtained in the same planes as CINE images beginning 5 min after injection 0.2 mmol/kg of gadolinium with phase sensitive inversion recovery sequences. One patient was unable to receive contrast due to poor renal function. The presence and distribution of enhancement in each left ventricle segment and enhancement in the right ventricle and atria was also recorded. STIR images were not routinely performed as patients had been diagnosed with amyloidosis many years previously and were not in the acute phase of the disease process.
2.3. Hematologic treatment methods
Hematologic treatment typically involved induction with a variety of anti-plasma cell therapies, reflecting the introduction of immunomodulatory agents (thalidomide and lenalidomide) and protease inhibitors (botezomib). High-dose chemotherapy with melphalan 140–200 mg/m2 split over 2 days was given before PBSCT. Peripheral blood stem cell reinfusion was undertaken with the patient monitored in the coronary care unit. Inpatient care continued until engraftment and recovery were clinically apparent.
2.4. Statistical methods
Continuous data were analyzed comparing paired t tests of the means. Diastolic function was assessed parametrically using the chi-squared test. Statistical analysis was completed using MaxStat Pro version 3.6 statistical software.
3. Results
There were 30 patients with cardiac amyloidosis who underwent high-dose chemotherapy and PBSCT for AL amyloidosis or multiple myeloma. Of these, 15 patients were shown to have significant echocardiographic regression. At the time of the study, 14 patients were able to be reviewed, with one patient lost to follow-up. Five of 14 patients were still alive. One of these patients had an ICD that was not MRI compatible and was unable to participate. This left 4 patients for analysis.
The mean age of the surviving four patients was 49 years (+/− 8.0 years) at the time of the PBSCT. At the final analysis, it had increased to 60 years (+/− 5.6 years). On average, the patients had survived over 11.5 years (+/− 4.3 years) since diagnosis. It took a mean of 22 months from PBSCT for the patients to show regression of cardiac features on echocardiography (see Table A.1). All four patients were clinically well with New York Heart Association Class 1 symptoms (no limitations, ordinary physical activity does not cause undue dyspnea or fatigue) [24].
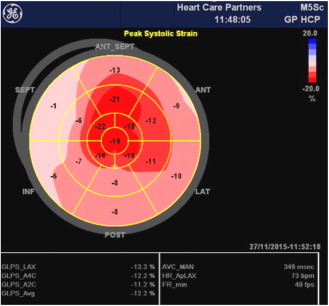
Echocardiography suggested statistically significant regression in the cardiac amyloid process, similar to what had previously been reported [18]. Wall thickness significantly reduced, atrial size shrunk, and measures of diastolic function improved (see Fig. B.1 ; Fig. B.2). The ejection fraction did not significantly change. Myocardial strain analysis at late follow-up suggested better global longitudinal strain in this highly selected group of survivors, than many cardiac amyloid studies have suggested (the global longitudinal strain was more negative than previously reported for cardiac amyloid patients) [13]; [25] ; [26]. The mean global longitudinal strain was − 16%. The classical bulls-eye pattern of cardiac amyloidosis was only seen in 50% of these patients [13] ; [26] (see Fig. B.3 and Table A.2). Strain had not been assessed before PBSCT for any of the patients in this study.
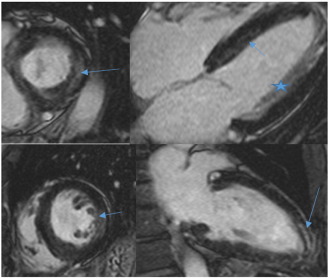
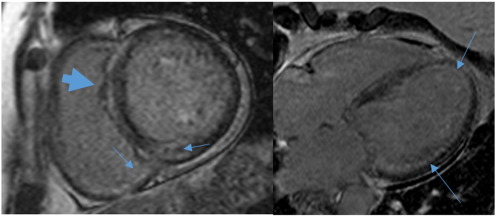
There was good correlation of the ejection fractions and left ventricular wall thicknesses between CMR and echocardiography (see Table A.2, Fig. B.4 ; Fig. B.5). All four of the CMR studies suggested persisting presence of patchy diffuse gadolinium enhancement, consistent with the ongoing presence of residual insoluble amyloid material. In each case on CMR, there was diffuse myocardial enhancement of both ventricles with relative ventricular apical sparing, a pattern typical for amyloidosis infiltration [14] ; [27]. The extent of enhancement in the majority of myocardial segments was subendocardial or involved the mid-wall with limited transmural enhancement (see Fig. B.4 ; Fig. B.5). On average, 3.5/17 segments demonstrated transmural enhancement, predominantly within the left ventricular free wall (segments 5, 6, 11, and 12 of the 17-segment model). There was also patchy enhancement within the right ventricle in each case and minimal patchy enhancement in the atrial walls. Ventricular wall thickness was in the normal range or near normal in each case, and there was no significant interatrial septal thickening [28].
4. Discussion
Previous research had shown that about 50% of cardiac amyloidosis patients who complete chemotherapy and PBSCT with hematological remission achieve marked regression of cardiac involvement [18]. These patients were shown to have longer survival than those who did not achieve cardiac regression [18]. Remission of cardiac infiltration as assessed by gadolinium enhancement on CMR imaging has been shown in one reported case [19].
Repeat echocardiography on the day of the CMR at late follow-up confirmed that patients still had macroscopic regression of cardiac infiltration, based on the echocardiographic images. There was marked improvement in echocardiographic anatomical and functional parameters compared to the pre-PBSCT echocardiograms. The post-PBSCT echocardiograms showed near normal global longitudinal strain. The classical bulls-eye pattern of cardiac amyloidosis [13] was seen in 50% of these echocardiograms. The CMR scans in this study showed similar wall thicknesses to that shown on echocardiography, supporting the suggestion that disease regression can occur in cardiac amyloidosis.
CMR had not been performed before PBSCT for these patients. Persistent reversal of the cardiac changes on echocardiography suggests significant regression of the infiltrative process in these patients. It was therefore surprising to see gadolinium uptake with CMR, indicating persistent amyloid infiltration of the myocardium. Myocardial enhancement in amyloidosis has been described as a very poor prognostic indicator, with pathophysiological studies suggesting that the enhancement is secondary to amyloid protein deposition in the extracellular matrix of the heart [16] ; [28]. The pattern of enhancement following treatment with PBSCT remained typical for amyloid, with a subendocardial or mid-wall distribution. This CMR pattern has been associated with milder disease [14]. The enhancement pattern was not associated with myocardial thickening, which suggests reduced protein deposition and an associated decrease in myocardial oedema. Previous case reports and series have demonstrated a decrease in myocardial wall thickness and enhancement following PBSCT [19]; [20] ; [21].
These data suggest that modern treatments for cardiac amyloidosis can result in macroscopic regression of the infiltrative process in the heart. Complete resolution of the cardiac process does not appear to occur. Current hematologic opinion is that remission is possible with AL amyloidosis, but that “cure” is unlikely [29] ; [30]. This study suggests that remission is also possible for the cardiac process. Whilst infiltration appears to regress macroscopically and functionally on echocardiography, CMR gadolinium imaging suggests that amyloid protein deposition does not completely resolve. This would add weight to the belief that the disease is not cured, but is suppressed. This pattern of gadolinium enhancement may represent residual insoluble amyloid infiltration, after remission of the hematologic and cardiac processes. The insoluble nature of the amyloid fibrils may mean that complete resolution is difficult. Physiologically, such persistence of amyloid in the extracellular matrix would result in weakening of the integrity of the myocyte structure and predispose the heart to torsional strain [31]. This may explain why the greatest extent of transmural enhancement is occurring in each of these cases in the left ventricular free wall—the site of maximal torsional strain [32]. It has been proposed that after treatment, the toxic light chains may resolve, leaving a non-toxic amyloid protein [33]. It may be these residual protein deposits that are shown on CMR.
The differential for myocardial enhancement includes myocardial fibrosis or scar from other causes such as an ischemic insult. However, in our case series, the enhancement was a non-coronary distribution. Fibrosis is said to have different imaging characteristics on CMR [14]; [16] ; [17]. These changes are subtle, and fibrosis as a cause of the changes seen cannot be excluded. The patients did not have a medical history that would suggest an ischemic or alternative cause of enhancement. Cardiac biopsy could be considered for these cases to provide a definitive tissue diagnosis. This would require an invasive test with procedural risk for patients who are otherwise healthy, and in long-term remission. Despite being the gold standard, sampling errors are seen [3]; [22] ; [25]. These patients have had long-term survival. Before the routine use of PBSCT, cardiac patients on average survived less than 6 months from diagnosis [1]. With modern treatment regimens, mean survival in patients who did not have a cardiac response has been extended to 49 months in one series [18]. For these patients with cardiac regression, very long-term survival with a mean of 139 months has been achieved. This represents an increase from half a year in the 1990s to over 11 years now.
An ongoing, prospective study of new patients with cardiac amyloidosis is also being conducted. Matched echocardiograms and CMR before and after PBSCT will be performed. The repeat CMR will be done at the time that echocardiography suggests regression of the amyloid process in the heart. This will hopefully provide more clarity on what is happening in the hearts of these patients.
There are a number of limitations with this research. Cardiac amyloidosis is a rare condition. This is a highly selected group of patients. The patients included were identified retrospectively. The observation of cardiac improvement was only made many years after BMT had been completed. The CMR was not conducted before PBSCT, and comparison therefore could not be done. Strain echocardiography was not done before PBSCT. The diagnosis of cardiac amyloidosis was made by echocardiography and ECG rather than with cardiac biopsy, raising the possibility that the patients did not have true cardiac involvement. It is possible that this cohort contains patients with hypertensive left ventricular hypertrophy or other infiltrative processes, whose echocardiograms have regressed with medical therapy. However, the low-voltage ECGs of these patients would argue against a diagnosis of hypertensive heart disease. Additionally, patients with hypertension tend to have lower grades of diastolic dysfunction and smaller atria than cardiac amyloid patients [9]. Another infiltrative process should not have responded to the treatment of chemotherapy and BMT. A variety of different echocardiography machines were used for the diagnostic study before PBSCT, reflecting real-world practice. Ideally, a single machine brand and model would have been used, to maximize reproducibility. This was done with the subsequent echocardiograms done the day of the CMR. The reviewers were not blinded to the clinical results. Measurement bias could occur when the echocardiographic and MRI results were reviewed. This paper is an observational study. It is a single-centre experience. The numbers of patients involved are small. As a result, it is possible that the findings shown are due to chance. Nonetheless, the results are extremely interesting.
5. Conclusions
Multiple myeloma and amyloidosis are rare and serious conditions, with significant morbidity and mortality. Cardiac involvement makes a guarded prognosis even more limited. High dose chemotherapy and PBSCT have resulted in hematologic remission in some patients. This study demonstrates that highly selected patients may achieve cardiac regression also. Multimodality cardiac imaging plays a vital role in diagnosis and management. Echocardiography appears to produce similar structural changes to that seen with CMR, reaffirming its role as a screening test and for progress studies. The superior tissue analysis available with CMR confirms its role as a confirmatory test. It is often done as a substitute for cardiac biopsy. Additional structural data are also provided, making it a very complementary investigation to TTE. Based on these new CMR data, the previous expectation of complete reversal of the cardiac process in selected patients would not appear to occur. These CMR findings suggest residual insoluble amyloid fibrils in the myocardium in the setting of disease remission. However, these patients do achieve very prolonged longevity with significantly improved survival in these rare and deadly diseases.
Conflict of interest
There are no conflicts of interest.
Acknowledgments
The CMR studies were performed with funding provided by a research grant from the Wesley Medical Research (HREC Register No. 1304, WRI 2011-21).
Appendix A
| Age at PBSCT | 49 years | +/− 8.0 years |
|---|---|---|
| Age at the final study data point | 60 years | +/− 5.6 years |
| Total survival (from diagnosis) | 139 months (11.5 years) | +/− 4.3 years |
| Time to cardiac regression (from PBSCT) | 22 months | +/− 4.7 months |
| TTE pre PBSCT | TTE Post | p value | CMR | p value | |
|---|---|---|---|---|---|
| Ejection fraction | 64% | 63% | 0.80 | 66% | 0.80 |
| Diastolic function | Grade 2–3 | Normal to Grade 1 | |||
| IVS | 17 mm | 12 mm | 0.036 | 13 mm | 0.88 |
| PW | 16 mm | 11 mm | 0.043 | 11 mm | 0.88 |
| LAA | 28 cm2 | 18 cm2 | 0.073 | 22 cm2 | |
| LAV | 39 ml/m2 | 38 ml/m2 | 0.38 | ||
| Strain | —15.6% | ||||
| Bullseye pattern | 2/4 (50%) | ||||
| Gadolinium enhancement | 4 out of 4 (100%) |
TTE, transthoracic echocardiogram; PBSCT, peripheral blood stem cell transplant; CMR, cardiac magnetic resonance imaging; IVS, Interventricular septal wall thickness (segment 2–17), PW, posterior wall thickness (segment 5), LAA – Left atrial area, LAV – Left atrial volume
Appendix B
|
|
|
Fig. B.1. Pre-PBSCT echocardiogram. |
|
|
|
Fig. B.2. Post-PBSCT echocardiogram. |
|
|
|
Fig. B.3. “Bulls-eye” strain pattern of cardiac amyloidosis. |
|
|
|
Fig. B.4. CMR. CMR short axis, 4-chamber and 2-chamber views in a 65-year-old female, 8 years post successful PBSCT of AL amyloidosis. CMR shows patchy mid-wall enhancement in a non-coronary distribution (arrows). Myocardial wall thickness is within the normal range, correlating with the echocardiogram findings of reduced myocardial thickness following treatment. Prominent papillary muscles are also seen laterally in the 4-chamber view (star), with associated blood pooling. The changes correspond to the patients clinical improvement. |
|
|
|
Fig. B.5. CMR. Cardiac MRI mid-ventricle short axis and 4-chamber views performed on a 58-year-old female, 19 years following treatment and clinical regression. MRI demonstrates myocardial wall thickness in the normal range and diffuse subendocardial enhancement of the left ventricle (thin arrows) and right ventricular aspect of the interventricular septum (broad arrow). The enhancement is in a non-coronary distribution which would support residual areas of amyloid protein deposition following treatment. |
References
- [1] R.H. Falk, R.L. Comenzo, M. Skinner; The systemic amyloidoses; N. Engl. J. Med., 337 (1997), pp. 898–909
- [2] R.A. Kyle; Amyloidosis: a convoluted story; Br. J. Haematol., 114 (2001), pp. 529–538
- [3] A.D. Cohen, R.L. Comenzo; Systemic light-chain amyloidosis: advances in diagnosis, prognosis, and therapy; Hematology, 2010 (2010), pp. 287–294
- [4] Oxford Textbook of Medicine; (fifth ed.)Oxford University Press, Oxford (2010)
- [5] R.H. Falk; Cardiac amyloidosis—a treatable disease, often overlooked; Circulation, 124 (2011), pp. 1079–1085
- [6] M.A. Gertz, M.Q. Lacy, A. Dispenzieri; Myeloablative chemotherapy with stem cell rescue for the treatment of primary systemic amyloidosis: a status report; Bone Marrow Transplant., 25 (2000), pp. 465–470
- [7] M. Attal, J.L. Harousseau, A.M. Stoppa, J.J. Sotto, J.G. Fuzibet, J.F. Rossi, P. Casassus, H. Maisonneuve, T. Facon, N. Ifrah, C. Payen, R. Bataille; A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma; N. Engl. J. Med., 335 (1996), pp. 91–97
- [8] M. Skinner, V. Sanchorawala, D.C. Seldin, L.M. Dember, R.H. Falk, J.L. Berk, J.J. Anderson, C. O'Hara, K.T. Finn, C.A. Libbey, J. Wiesman, K. Quillen, N. Swan, D.G. Wright; High-dose melphalan and autologous stem-cell transplantation in patients with AL amyloidosis: an 8-year study; Ann. Intern. Med., 140 (2004), pp. 85–93
- [9] B.T. Fitzgerald, G.M. Scalia, P.A. Cain, M.J. Garcia, J.D. Thomas; Left atrial size—another differentiator for cardiac amyloidosis; Heart Lung Circ., 20 (2011), pp. 574–578
- [10] Principles and Practice of Echocardiography; (second ed.)Lea & Febiger, Philadelphia (1994)
- [11] The Practice of Clinical Echocardiography; (second ed.)WB Saunders, Philadelphia (2002)
- [12] A.L. Klein, O. JH, F.A. Miller, J.B. Seward, A.J. Tajik; Two-dimensional and Doppler echocardiographic assessment of infiltrative cardiomyopathy; J. Am. Soc. Echocardiogr., 1 (1988), pp. 48–59
- [13] D. Phelan, P. Collier, P. Thavendiranathan, Z.B. Popović, M. Hanna, J.C. Plana, T.H. Marwick, J.D. Thomas; Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis; Heart, 98 (2012), pp. 1442–1448
- [14] M. Fontana, S. Pica, P. Reant, A. Abdel-Gadir, T.A. Treibel, S.M. Banypersad, V. Maestrini, W. Barcella, S. Rosmini, H. Bulluck, R.H. Sayed, K. Patel, S. Mamhood, C. Bucciarelli-Ducci, C.J. Whelan, A.S. Herrey, H.J. Lachmann, A.D. Wechalekar, C.H. Manisty, E.B. Schelbert, P. Kellman, J.D. Gillmore, P.N. Hawkins, J.C. Moon; Prognostic value of late gadolinium enhancement cardiovascular magnetic resonance in cardiac amyloidosis; Circulation, 132 (2015), pp. 1570–1579
- [15] G. Di Bella, F. Pizzino, F. Minutoli, C. Zito, R. Donato, G. Dattilo, G. Oreto, S. Baldari, G. Vita, B.K. Khandheria, S. Carerj; The mosaic of the cardiac amyloidosis diagnosis: role of imaging in subtypes and stages of the disease; Eur. Heart J. Cardiovasc. Imaging, 15 (2014), pp. 1307–1315
- [16] R.Q. Migrino, R. Christenson, A. Szabo, M. Bright, S. Truran, P. Hari; Prognostic implication of late gadolinium enhancement on cardiac MRI in light chain (AL) amyloidosis on long term follow up; BMC Med. Phys., 9 (2009), pp. 1–7
- [17] B.A. Austin, W.H. Tang, E.R. Rodriguez, C. Tan, S.D. Flamm, D.O. Taylor, R.C. Starling, M.Y. Desai; Delayed hyper-enhancement magnetic resonance imaging provides incremental diagnostic and prognostic utility in suspected cardiac amyloidosis; JACC Cardiovasc. Imaging, 2 (2009), pp. 1369–1377
- [18] B.T. Fitzgerald, J. Bashford, G.M. Scalia; The return of the normal heart: resolution of cardiac amyloidosis after chemotherapy and bone marrow transplantation; Heart Lung Circ., 22 (2013), pp. 655–660
- [19] V. Brahmanandam, S. McGraw, O. Mirza, A.A. Desai, A. Farzaneh-Far; Regression of cardiac amyloidosis after stem cell transplantation assessed by cardiovascular magnetic resonance imaging; Circulation, 129 (2014), pp. 2326–2328
- [20] G. Reich, T. Held, W. Siegert, D. Kampf, B. Dörken, G. Maschmeyer; Four patients with AL amyloidosis treated with high-dose chemotherapy and autologous stem cell transplantation; Bone Marrow Transplant., 27 (2001), pp. 341–343
- [21] H.K. Meier-Ewert, V. Sanchorawala, J. Berk, K.T. Finn, M. Skinner, D.C. Seldin, F.L. Ruberg; Regression of cardiac wall thickness following chemotherapy and stem cell transplantation for light chain (AL) amyloidosis; Amyloid, 18 (2011), pp. 130–131
- [22] C.R. Bonnichsen, J.F. Glockner, M. Grogan; Improvement in myocardial delayed enhancement after autologous stem cell transplant in a patient with light chain amyloidosis; Circ. Heart Fail., 5 (2012), p. e55
- [23] M.A. Gertz, R. Comenzo, R.H. Falk, J.P. Fermand, B.P. Hazenberg, P.N. Hawkins, G. Merlini, P. Moreau, P. Ronco, V. Sanchorawala, O. Sezer, A. Solomon, G. Grateau; Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004; Am. J. Hematol., 79 (2005), pp. 319–328
- [24] C.W. Yancy, M. Jessup, B. Bozkurt, J. Butler, D.E. Casey Jr., M.H. Drazner, G.C. Fonarow, S.A. Geraci, T. Horwich, J.L. Januzzi, M.R. Johnson, E.K. Kasper, W.C. Levy, F.A. Masoudi, M.B. PE, M.M. JJ, J.E. Mitchell, P.N. Peterson, B. Riegel, F. Sam, L.W. Stevenson, W.H. Tang, E.J. Tsai, B.L. Wilkoff; 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines; Circulation, 128 (2013), pp. e240–e327
- [25] S.J. Buss, M. Emami, D. Mereles, G. Korosoglou, A.V. Kristen, A. Voss, D. Schellberg, C. Zugck, C. Galuschky, E. Giannitsis, U. Hegenbart, A.D. Ho, H.A. Katus, S.O. Schonland, S.E. Hardt; Longitudinal left ventricular function for prediction of survival in systemic light-chain amyloidosis: incremental value compared with clinical and biochemical markers; J. Am. Coll. Cardiol., 60 (2012), pp. 1067–1076
- [26] M.C. Porciani, F. Cappelli, F. Perfetto, M. Ciaccheri, G. Castelli, I. Ricceri, M. Chiostri, B. Franco, L. Padeletti; Rotational mechanics of the left ventricle in AL amyloidosis; Echocardiography, 27 (2010), pp. 1061–1068
- [27] P. Lu, H. Van Acker, P. Waer; Cardiac Amyloidosis Diagnosed on Mri. JBR-BTR : organe de la Societe royale belge de radiologie; 98 (2015), pp. 48–49
- [28] N. Kawel, E.B. Turkbey, J.J. Carr, J. Eng, A.S. Gomes, W.G. Hundley, C. Johnson, S.C. Masri, M.R. Prince, R.J. van der Geest, J.A. Lima, D.A. Bluemke; Normal left ventricular myocardial thickness for middle-aged and older subjects with steady-state free precession cardiac magnetic resonance: the multi-ethnic study of atherosclerosis; Circ. Cardiovasc. Imaging, 5 (2012), pp. 500–508
- [29] E. Muchtar, F. Buadi, A. Dispenzieri, M.A. Gertz; Immunoglobulin light-chain amyloidosis: from basics to new developments in diagnosis, prognosis and therapy; Acta Haematol., 135 (2016), pp. 172–190
- [30] E. Kastritis, M.A. Dimopoulos; Recent advances in the management of AL Amyloidosis; Br. J. Haematol., 172 (2016), pp. 170–186
- [31] I. Kholova, H.W. Niessen; Amyloid in the cardiovascular system: a review; J. Clin. Pathol., 58 (2005), pp. 125–133
- [32] G. Buckberg, J.I. Hoffman, A. Mahajan, S. Saleh, C. Coghlan; Cardiac mechanics revisited: the relationship of cardiac architecture to ventricular function; Circulation, 118 (2008), pp. 2571–2587
- [33] D.B. Richards, L.M. Cookson, A.C. Berges, S.V. Barton, T. Lane, J.M. Ritter, M. Fontana, J.C. Moon, M. Pinzani, J.D. Gillmore, P.N. Hawkins, M.B. Pepys; Therapeutic clearance of amyloid by antibodies to serum amyloid p component; N. Engl. J. Med., 373 (2015), pp. 1106–1114
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?