Keywords
64-MDCT;Pulmonary vein thrombosis;Hidden small pulmonary vein
1. Background
Stroke is a leading cause of serious long-term disability and the third-leading cause of death [1]. Acute ischemic stroke accounts for approximately 70% of all strokes, and cardiac embolism accounts for approximately 15% of embolic strokes.
Atrial fibrillation (AF), which is responsible for 10% of all ischemic strokes and half of all cardioembolic strokes, increases the risk of stroke by 4- to 5-fold in nonrheumatic patients. The left atrial appendage (LAA) is the most common location in which a thrombus forms in the left atrium (LA). Transesophageal echocardiography is a routine clinical procedure that is frequently used prior to cardioversion to detect an LA thrombus.
Pulmonary vein thrombosis is a potentially life threatening condition that can lead to thromboembolic stroke, but the occurrence of this type of thrombosis is believed to be rare and often goes undiagnosed and untreated.
The primary causes of pulmonary vein thrombi formation are thought to be lung surgery [2], lung transplantation [3] ; [4], and increased expansion of lung cancer [5]. The signs and symptoms of this condition are generally atypical, thus resulting in its underdiagnosis.
Since 2012, I have published many cases of pulmonary vein thromboses in elderly patients who present without traditional clinical conditions. In 2014, I reported that 35 (61%) of 57 elderly patients with chest pain had a pulmonary vein thrombus [6], indicating that pulmonary vein thromboses are more common in elderly populations. In 2015, I reported that a small thrombus in the visible small pulmonary vein was connected to a larger thrombus in the pulmonary vein [7]. However, the method by which the small pulmonary vein thrombus became completely occluded is unknown. Here, I describe a case report identifying a smaller pulmonary vein involved in the formation of smaller thrombi.
2. Case reports
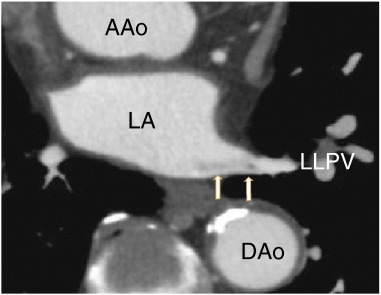
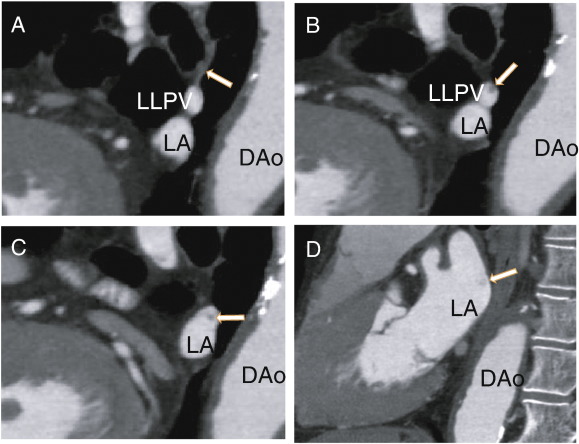
The patient was a 78-year-old male who presented with chest pain and had no previous treatment with warfarin. D-dimer was less than 0.5 μg/ml (normal value < 1.0 μg/ml), protein S activity was 91% (normal range 60–150%), and protein C activity was 66% (normal range 64–146%). He was treated with aspirin (82 mg i.d.) as an antiplatelet therapy. The patient was referred to our hospital for the evaluation of coronary artery stenosis. The chest roentgenogram was negative for lung cancer. The patient had no symptoms of cough, cerebral infarction or cancer, and the patient had no history of either catheter ablation or lung surgery. A 64-MDCT scan showed a pulmonary vein thrombus (Fig. 1); however, there were no thrombi in the left lower pulmonary vein (LLPV) at first. A non-contrast enhanced vessel, which might have been completely occluded, approached from the upper side (Fig. 2A). There, a non-contrasted branch of the pulmonary vein at the upper side of the LLPV was observed (Fig. 2B), which extended proximally in keeping the position on the upper side of LLPV (Fig. 2C). The contrast enhancement defects did not diffuse and enter the LA (Fig. 2D).
|
|
|
Fig. 1. Axial images showing the left lower pulmonary vein thrombus (arrows). AA; ascending aorta, DAo; descending aorta, LA; left atrium, LLPV; left lower pulmonary vein. |
|
|
|
Fig. 2. A: Sagittal images showing the left lower pulmonary vein and the non-contrast small pulmonary vein (arrow). B: Sagittal images showing the thrombus in the left lower pulmonary vein as a defect of small enhancements (arrow). C: Sagittal images showing the larger pulmonary vein thrombus, which was separate from the wall of the left lower pulmonary vein (arrow). D: Sagittal images showing the thrombus in the left atrium (arrow). DAo: descending aorta, LA: left atrium, LLPV: left lower pulmonary vein. |
3. Discussion
Although I have published the detection of a thrombus in the visible fine pulmonary vein with contrast, enhancements have contributed to the recognition of a pulmonary vein thrombus [7]. However, it is a novel notion to diagnose a completely occluded small pulmonary vein thrombus, which requires new methodology that is not generally recognized at present. In this report, I showed a completely occluded small pulmonary vein thrombus, which flew into the LLPV, as assessed using 64-MDCT.
Ischemic stroke is a serious clinical problem. Although cardioembolic stroke generally results in more severe disability because of the larger affected area compared to other types of ischemic stroke, pulmonary vein thrombosis is undiagnosed. As I have reported, 49% (17 patients) of 35 patients with pulmonary vein thrombosis extended into the left atrium [8], which also applies to the case described here.
Warfarin and recently developed anticoagulants such as dabigatran are used to prevent ischemic stroke in patients with AF. If health care providers fail to recognize the dangers of pulmonary vein thrombosis, it could be difficult to accurately evaluate the risk of cerebral infarction.
Another critical problem is that left lower pulmonary vein thrombosis results in hypoxia and malnourishment of the left lower pulmonary vein, the effects of which are unclear. Hypoxia activates hypoxia inducible factors (HIFs), which are transcription factors that may be associated with genetic regulations.
Hypoxia and malnourishment manifest in various pulmonary diseases, including some types of asthma and lung cancer, via loss of normal cell function in the lungs and live under such conditions. Additionally, these symptoms affect pulmonary vein structure such as the pulmonary vein myocardium by activating HIFs, which may be associated with the progression and maintenance of AF [9].
To prevent these unfavorable effects, we needed to assess the existence of a thrombus in the small pulmonary vein. If detected, the thrombus must be dissolved by either warfarin or NOACs such as dabigatran. It is an important to determine whether a completely occluded pulmonary vein thrombus could be dissolved to avoid its injurious effects on lung cells and pulmonary vein myocardium.
The appearance of a small thrombus in the pulmonary vein indicates the existence of a small hidden pulmonary vein, which may extend into the left atrium and be a source of thrombus formation in the pulmonary vein and in the left atrium.
Conflict of interest
The author reports no relationships that could be construed as a conflict of interest.
References
- [1] G.J. Hankey, C.P. Warlow; Treatment and secondary prevention of stroke: evidence, costs, and effects on individuals and populations; Lancet, 354 (1999), pp. 1457–1463
- [2] H. Hovaguimian, J.F. Morris, H.L. Gately, H.S. Floten; Pulmonary vein thrombosis following bilobectomy; Chest, 99 (1991), pp. 1515–1516
- [3] M.A. Sarsam, N.A. Yonan, D. Beton, D. McMaster, A.K. Deiraniya; Early pulmonary vein thrombosis after single lung transplantation; J Heart Lung Transplant, 12 (1993), pp. 17–19
- [4] D.R. McIlroy, A.C. Sesto, M.R. Buckland; Pulmonary vein thrombosis, lung transplantation and intraoperative transesophageal echocardiography; J Cardiothorac Vasc Anesth, 20 (5) (2006), pp. 712–715
- [5] E. Nelson, J.S. Klein; Pulmonary infarction resulting from metastatic osteogenic sarcoma with pulmonary venous tumour thrombus; AJR, 174 (2000), pp. 531–533
- [6] H. Takeuchi; High prevalence of pulmonary vein thrombi in elderly patients with chest pain, which has relationships with aging associated diseases; IJC Heart Vessels, 4 (2014), pp. 129–134 https://doi.org/10.1016/j.ijchv.2014.05.006 [Published online: 6-JUN-2014]
- [7] H. Takeuchi; A long and narrow pulmonary vein thrombus attached to the wall of pulmonary vein; IJC Heart Vasc, 7 (2015), pp. 49–50
- [8] H. Takeuchi; Nearly all left atrial thrombi may be extended from pulmonary vein thrombi; IJC Heart Vasc, 7 (2015), p. 9
- [9] H. Takeuchi; Pulmonary vein thrombi in a patient with paroxysmal atrial fibrillation; IJC Heart Vasc, 5 (2014), pp. 63–64 https://doi.org/10.1016/j.ijcha.2014.10.006
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?