Abstract
Few studies have reported the differences between transthoracic echocardiography (TTE) and 64-slice multidetector CT (64-MDCT) in identifying left atrium (LA) thrombi. I report the case of a 70 year old man with coronary artery disease and angina who was diagnosed with a thrombus in the left lower pulmonary vein extending to the LA using a non-invasive 64-MDCT scan and TTE. TTE was unable to clearly identify a thrombus in the pulmonary veins, whereas a 64-MDCT scan identified a thrombus in the pulmonary vein but was unable to detect a moving thrombus attached to the mitral valves. The 64-MDCT images of LA thrombi are smaller than those of TTE and the video created using TTE demonstrated a moving thrombus connected to the mitral valve, which was underdiagnosed by a 64-MDCT scan. This case illustrates the complementary role for both TTE and 64-MDCT in the noninvasive diagnosis of left atrial-pulmonary vein thrombi.
Keywords
Pulmonary vein thrombosis;Left atrial thrombus;64-MDC;Transthoracic echocardiography
1. Introduction
Stroke is the second leading cause of death worldwide and is also the leading cause of disability. Atrial fibrillation (AF) affects 3–5% of the population older than 65 years. In addition, AF is responsible for 15–20% of ischemic strokes [1] and is a powerful, independent risk factor for ischemic stroke [2]. Overall, the risk of stroke in patients with non-rheumatic AF is approximately 5% per year [3]. The most common location of thrombus formation is the left atrial appendage (LAA) in non-valvular AF patients, and 90% of cardiac thrombi are located in the LAA, whereas 10% are located in the left atrium (LA).
Pulmonary vein thrombosis (PVT) has been observed in several scenarios, such as after catheter ablation for AF patients, lung cancer, and after lung transplantation. The symptoms of PVT can be non-specific and subtle before the observation of systemic thrombosis, such as cerebral infarction; therefore, the disease often goes underdiagnosed. Since 2012, I have reported some cases of pulmonary vein thrombosis, which were diagnosed in the patients without lung cancer, thoracic surgery or catheter ablation using 64-slice multidetector CT (64-MDCT) noninvasively.
Transoesophageal echocardiography (TOE) is a semi-invasive tool and is usually used to detect a thrombus in the LAA and the LA. A 64-MDCT scan is a noninvasive tool and becomes an option to assess coronary artery plaque. Furthermore, 64-MDCT scans can identify LAA thrombi and pulmonary vein thrombi automatically. Pulmonary vein thrombosis is thought to be rare, and little is known about the relationship between left atrial thrombi and pulmonary vein thrombi. Few studies have reported the differences between transthoracic echocardiography (TTE) and 64-MDCT in identifying LA thrombi. We reported an uncommon case of a LA thrombus connected to a left lower pulmonary vein (LLPV) thrombus using 64-MDCT scan and TTE, which showed a thrombus in the LA only by motionless images [4]. We have video images of the LA thrombus using TTE, which demonstrated the moving thrombus in detail.
By comparing the images obtained by 64-MDCT scan and TTE, it is possible to make a non-invasive diagnosis of a left atrial-pulmonary vein thrombus and initiate appropriate treatment to avoid serious thromboembolic complications such as ischemic stroke.
2. Case presentation
A 70-year-old male with angina pectoris, who had 4 stents in his coronary artery (#1, #6, #11 and high lateral), was referred to our hospital for the evaluation of restenosis in the coronary artery because he had recently experienced chest pain. The patient exhibited no symptoms of tachypnoea, fever, cough, sputum or cerebral infarction. The lung examination did not reveal decreased breath sounds, lung crackles or wheezing. The cardiac examination did not demonstrate a heart murmur or arrhythmia.
The chest roentgenogram revealed no obvious opacities to suggest lung cancer and no cardiomegaly. The patient had smoked 1 pack of cigarettes per day for approximately 20 years, from 20 to 40 years old. Laboratory investigation revealed anaemia with a haemoglobin level of 10.8 g/dl (normal range; 13.5–17.6 g/dl), hyperuricacidaemia with a uric acid level of 8.9 mg/dl (normal range; 3.0–7.2 mg/dl), hypoproteinaemia with a total protein of 6.1 g/dl (normal range; 6.5–8.0 g/dl), and normal electrolytes.
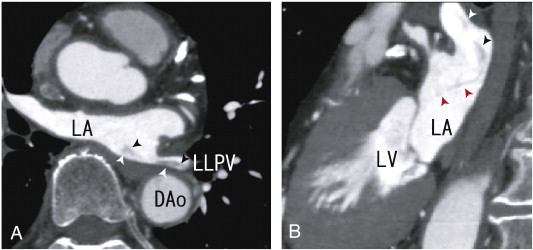
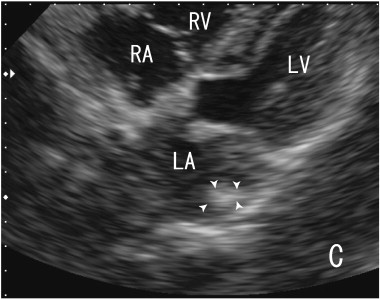
The patient was treated with 100 mg of aspirin without warfarin. The EKG indicated normal sinus rhythm, a normal axis and no ST-T changes, and the patients heart rate was 59 beats/min. A 64-MDCT scan was performed to assess the stenosis of the coronary artery because of recent chest pain. Although the stenosis of the coronary artery was not diagnosed, a large thrombus in LLPV and in LA was noninvasively identified as a defect in enhancements by 64-MDCT scan, which was shown in my previous paper [4]. A pulmonary vein thrombus was identified in LLPV as a defect in contrast enhancements (Fig. 1A and B). The thrombus was visualised using transthoracic echocardiography (TTE) in Fig. 2. In video images using TTE, a thrombus in the LA was demonstrated to be a large bright echodensity, suggesting a thrombus with a highly fibrinous component. The shape of the thrombus in video images was a wavelike, which indicated that the thrombus exhibited flexibility and was rather strong. Some parts of the thrombus attached to the mitral valve were not identified by a 64-MDCT. The volume of the LA was 39 ml, and the patient exhibited no thrombi in the LAA. In this case, TEE can assess the quality and quantity of a left atrial thrombus, but it cannot identify a pulmonary vein thrombus, which is well assessed by a 64-MDCT scan.
|
|
|
Fig. 1. A. 64-MDCT axial images demonstrating a thrombus from the left lower pulmonary vein to the left atrium (LA) (arrowheads) as the defect of enhancement. The middle parts of the thrombus were illustrated weakly. DAo; descending aorta, LA; left atrium, LLPV; left lower pulmonary vein. B. 64-MDCT sagittal images demonstrating the thrombus from the left lower pulmonary vein to the left atrium (LA) (arrowheads). The merge of the thrombus was vague. A vague, thin line-like defect was observed (red arrowheads). This thin line may represent a thrombus connecting mitral valve. A part of the thrombi seemed to be attached to the posterior wall of LA. DAo; descending aorta, LA; left atrium. |
|
|
|
Fig. 2. Images of transthoracic echocardiography (TTE). The thrombus in the left atrium (LA) was surrounded by arrowheads, which was located at the posterior wall side in the LA. The echodensity of the thrombi was high, which indicated that the thrombus was fibrous. LA; left atrium, LV; left ventricle, RA; right atrium, RV; right ventricle. |
3. Discussion
This is the first case to demonstrate a pulmonary vein thrombus connecting to a moving left atrial thrombus using TTE. The present case is the first to report this condition in the absence of lung cancer, thoracic surgery, or catheter ablation.
This case highlights the complementary role for the imaging modalities of TTE and 64-MDCT in the non-invasive diagnosis and characterization of left atrial-pulmonary vein thrombus. In our previous report, there was no video of the thrombus, which showed the motion of the thrombus. In this manuscript, we present the video images obtained using TTE, which demonstrated a moving thrombus in the LA. However, TTE images cannot identify pulmonary vein thrombi. The thrombus in the present case was a large bright echodensity thrombus, which indicates that the thrombus was highly fibrous. The shape of the thrombus resembled a wave, which means that the thrombus was flexible and strong.
These video images demonstrated that the thrombus in the left atrium appeared to be connected to the mitral valve, which could not be observed by 64-MDCT scan images. The reason why the thrombus could not be illustrated by the 64-MDCT scan may be small in size and the motion of the thrombus connected to the mitral valve. When we check the thrombus using 64-MDCT, we had better think the thrombus may be smaller than the real one and the motion of the mitral valve might make the attached portion of the left atrial thrombus invisible. Both the thick portion of the left atrial thrombus as well as the thin portion seemed to have disappeared when the thrombus was examined using 64-MDCT. Some parts of the thrombus attached to the mitral valve were not observed by 64-MDCT. 64-MDCT can illustrate a thrombus in the pulmonary vein, LA and left atrial appendage, but it is unable identify thrombi attached to the mitral valve because of small size and movings.
4. Conclusion
TTE and 64-MDCT have complementary roles in the non-invasive diagnosis of pulmonary vein and left atrial thrombi. To the best of our knowledge, this is the first reported case of pulmonary vein thrombus connected to a moving left atrial thrombus using TTE. A left atrial thrombus depicted by TTE gives us a clue to identify a thrombus in the pulmonary vein. TTE can characterize the location, motion, and consistency of thrombi with the LA. 64-MDCT can identify thrombus in the pulmonary vein.
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
Appendix A. Supplementary data
Supplementary video.
References
- [1] E. Crystal, S.J. Connolly; Role of oral anticoagulation in management of atrial fibrillation; Heart, 90 (2004), pp. 813–817
- [2] P.A. Wolf, R.D. Abbott, W.B. Kannel; Atrial fibrillation as an independent risk factor for stroke: the Framingham Study; Stroke, 22 (1991), pp. 983–988
- [3] Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: analysis of pooled data from five randomized controlled trials; Arch Intern Med, 154 (1994), pp. 1449–1457
- [4] H. Takeuchi; 64-MDCT can depict the thrombi expanded from the left lower pulmonary vein to the left atrium in the patient with angina pectoris; BMJ Case Rep (Apr 3 2013) https://doi.org/10.1136/bcr-2013-008750 [pii:bcr2013008750]
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?