Summary
Pseudomelanosis duodeni is a rare endoscopic finding that manifests as dark speckled spots in the duodenum. It is considered a benign condition and is associated with certain diseases and the use of certain medications. This study reports a case of a 74-year-old woman, with end-stage renal disease under maintenance hemodialysis, hypertension under regular medical control, iron deficiency anemia under oral iron supplement, and progressive anemia with suspicious occult gastrointestinal bleeding. Upper gastrointestinal endoscopy revealed multiple tiny brownish-black pigmentation throughout the proximal second portion of the duodenum. The histopathological examination showed pigment-laden macrophages with positive iron stain and negative melanin stain in the lamina propria of the mucosal villi.
Keywords
Antihypertensive drugs ; Chronic renal failure ; Pseudomelanosis duodeni
Introduction
Bisordi and Kleinman [1] first described pseudomelanosis duodeni as melanosis duodeni in 1976. It denotes a benign condition characterized by the rare endoscopic appearance of discrete speckled black pigmentation of the duodenal mucosa. Because the pigment is not produced by melanocytes, the term melanosis is justifiably taken to mean pseudomelanosis [2] . The majority of patients with this condition are female and aged over 60 years. Although the mechanism and clinical significance remain unclear, it is believed to be associated with certain diseases such as chronic heart failure, chronic renal failure, hypertension, diabetes mellitus, gastrointestinal bleeding, and the use of certain drugs, such as ferrous sulfate, hydralazine, propranolol, thiazide, furosemide, methyldopa, and digoxin [3] .
Case report
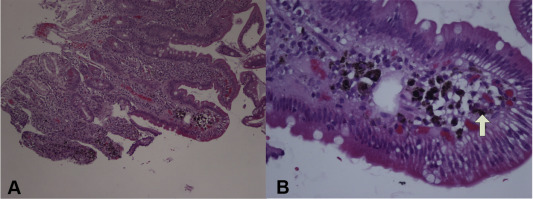
A 74-year-old woman had nephrosclerosis-related, end-stage renal disease treated with maintenance hemodialysis for 6 months, hypertension, and iron deficiency anemia, and underwent regular follow-up in the nephrology outpatient department of our hospital. The woman was undergoing long-term treatment with hydralazine, enalapril, furosemide, and ferrous sulfate for 2 years. The woman was referred to our gastroenterology outpatient department for further assessment of suspicious occult gastrointestinal bleeding owing to progressively decreasing hemoglobin index and positive fecal occult blood test. There was no history of vomiting, regurgitation, abdominal pain, hematemesis, melena, or abdominal lump. The upper gastrointestinal endoscopy revealed some antral hyperemic patches and multiple discrete speckled black pigmentation throughout the proximal second portion of the duodenum (Fig. 1 ). Antral and duodenal biopsies were performed. The histopathological examination of antral biopsy revealed gastritis without Helicobacter pylori infection, whereas duodenal biopsy revealed pigment-laden macrophages in the lamina propria of the mucosal villi that were focally positive for Perls' Prussian blue stain but negative for Masson–Fontana stain ( Fig. 2 ). The colonoscopy revealed a sigmoid colon polyp that was proven histologically to be a tubular adenoma with low-grade dysplasia and no melanosis was evident.
|
|
|
Figure 1. Upper gastrointestinal endoscopy disclosed multiple discrete speckled black pigmentation throughout the proximal second portion of the duodenum. |
|
|
|
Figure 2. Histological examination revealed pigmented granules within the lamina propria of macrophages (arrow) in the duodenal villi (hematoxylin and eosin stain; A: 100×; B: 400×). |
Discussion
Pseudomelanosis duodeni is a rare but harmless condition, and is more common in middle-aged to elderly female adults. Generally, it is asymptomatic, and is incidentally found to have pigment deposition in the duodenal mucosa on upper endoscopy [4] . The endoscopic differential diagnoses include melanoma and other pigmentations such as exogenous ingested charcoal [5] . Histology reveals the accumulation of dark pigmented granules and iron deposits within the macrophage lysosomes in the lamina propria near the tips of the duodenal villi [6] . Although no available study has reported the incidence, from 1978 to 2012, a total of 33 articles (22 duodenum, 6 jejunum and ileum, 2 stomach, 2 colon, and 1 esophagus) were published to describe patients with gastrointestinal pseudomelanosis. It seems to occur more frequently in the duodenum.
The pigment accumulation contains iron, sulfur, or melanin-like substances, such as hemosiderin, lipomelanin, and lipofuscin, and the pigment color represents various degrees of auto-oxidation of ferrous sulfide [7] ; [8] . The exact pathogenesis remains unclear. The analysis of epithelial cells and macrophages using electron probe X-ray has shown that absorbed iron is coupled with sulfur in pseudomelanosis duodeni, and this coupling is proposed to cause difficulty in iron transport and the accumulation of ferrous sulfide in macrophages of the duodenal lamina propria [9] . Therefore, oral iron supplement and sulfur-containing medications, such as furosemide and hydrochlorothiazide, are believed to be linked but not the sole factor with pseudomelanosis duodeni. As a matter of fact, most patients taking oral iron, but without other clinical diseases, do not develop pseudomelanosis duodeni. The underlying clinical disorders, especially chronic renal failure and diabetes mellitus, have a stronger association than above medications [6] .
Unlike iron or other heavy metal deposits elsewhere in the body, which may develop a fibroinflammatory reaction, pseudomelanosis duodeni has not been proved to cause fibrosis, stricture, or erosive duodenitis. The prognostic significance remained unknown, and no therapeutic chelating or regular upper endoscopy survey protocol is recommended in currently available literature, although long-term follow-up studies are still lacking. Among 46 patients in some case reports [10] , after cessation of ferrous sulfate and certain antihypertensive drugs for about 12 months, there were only three cases with complete and one case with partial disappearance of duodenal pigmentation. However, the actual time needed for complete regression of this pigmentation is not clear.
Old age, female sex, certain underlying diseases (including chronic heart failure, chronic renal failure, hypertension, diabetes mellitus, and gastrointestinal bleeding), and use of certain medications (including ferrous sulfate, hydralazine, propranolol, thiazide, furosemide, methyldopa, and digoxin) were believed to be the risk factors of pseudomelanosis duodeni. The cases reviewed in Table 1 show that the clinical characteristics were similar to cases in Western countries [11] ; [12] ; [13] ; [14] ; [15] , except that none had underlying renal disease and oral iron supplement. The patient reported here was an elderly woman, with end-stage renal disease and hypertension, and taking antihypertensive drugs and oral iron supplements. The biopsy specimens were positive for Perls' Prussian blue stain but not reactive for Masson–Fontana stain. Although Perls' Prussian blue stain is commonly used to reveal iron in tissues, a false-negative reaction is possible if an iron oxide compound is present rather than iron sulfide [8] .
| Study | Sex; Age (y) | Major comorbidity | Medication | Symptom | Endoscopic appearance | Iron staina | Melanin stainb |
|---|---|---|---|---|---|---|---|
| Lin et al, 1988 [11] | M; 64 | HTN, DM | — | Abdominal pain | Diffusely scattered small black spots over duodenal bulb and second portion | Weak positive | Strong positive |
| Kuo and Wu, 1988 [12] | F; 64 | HTN, DM | Furosemide Propranolol | None | Diffuse, scattered, black pigmentation over duodenal bulb and second portion | Negative | Strong positive |
| Wang et al, 1995 [13] | 6 M 2 F; 64.6 ± 9.1 | HTN (8/8) DM (1/8) | Thiazide (6/8) Propranolol (7/8) Hydralazine (8/8) Methyldopa (1/8) | Abdominal pain (4/8) Hiccup (1/8) None (3/8) | Diffuse, discrete, flat, small brownish-black spots in the duodenal mucosa (1 case with malignant gastric ulcer) | Strong positive (3/7) Weak positive (4/7) | Strong positive (7/7) |
| Kuo et al, 1999 [14] | — | — | — | — | Diffuse, discrete, flat, small brownish-black spots in the duodenal mucosa | — | Positive |
| Yen et al, 2009 [15] | M; 54 | HTN | Hydralazine Enalapril | None | Diffuse, discrete black pigmentation from the duodenal bulb to the second portion | — | — |
– = not mentioned; DM = diabetes mellitus; F = female; HTN = hypertension; M = male.
a. Perls' Prussian blue stain.
b. Masson–Fontana stain.
In conclusion, the long-term clinical impact of pigment on the duodenum remains unknown, and no specific treatment or follow-up is recommended for these endoscopic findings [16] .
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] W.M. Bisordi, M.S. Kleinman; Melanosis duodeni; Gastrointest Endosc, 23 (1976), pp. 37–38
- [2] J. Banai, A. Fenyvesi, G. Gonda, I. Peto; Melanosis jejuni; Gastrointest Endosc, 45 (1997), pp. 432–434
- [3] J.Y. Kang, A.Y. Wu, J.L. Chia, A. Wee, I.H. Sutherland, R. Hori; Clinical and ultrastructural studies in duodenal pseudomelanosis; Gut, 28 (1987), pp. 1673–1681
- [4] S. Ganju, J. Adomavicius, K. Salgia, F. Steigmann; The endoscopic picture of melanosis in the duodenum; Gastrointest Endosc, 26 (1980), pp. 44–45
- [5] J. Kim, J.K. Hwang, W.S. Choi, B.J. Lee, J.-J. Park, J.S. Kim, et al.; Pseudomelanosis ilei associated with ingestion of charcoal: case report and review of literature; Dig Endosc, 22 (2010), pp. 56–58
- [6] D. Giusto, S. Jakate; Pseudomelanosis duodeni: associated with multiple clinical conditions and unpredictable iron stainability – a case series; Endoscopy, 40 (2008), pp. 165–167
- [7] F.N. Ghadially, V.M. Walley; Pigments of the gastrointestinal tract: a comparison of light microscopic and electron microscopic findings; Ultrastruct Pathol, 19 (1995), pp. 213–219
- [8] H. Yamase, M. Norris, C. Gillies; Pseudomelanosis duodeni: a clinicopathologic entity; Gastrointest Endosc, 31 (1985), pp. 83–86
- [9] S. Fernando; Pseudomelanosis duodeni: a case report with electron-probe X-ray analysis; Pathology, 22 (1990), pp. 169–172
- [10] D.K. Rex, R.A. Jersild; Further characterization of the pigment in pseudomelanosis duodeni in three patients; Gastroenterol, 95 (1988), pp. 177–182
- [11] H.J. Lin, S.H. Tsay, H. Chiang, Y.T. Tsai, S.D. Lee, Y.S. Yeh, et al.; Pseudomelanosis duodeni: case report and review of literature; J Clin Gastroenterol, 10 (1988), pp. 155–159
- [12] Y.C. Kuo, C.S. Wu; Duodenal melanosis; J Clin Gastroenterol, 10 (1988), pp. 160–164
- [13] K. Wang, H.J. Lin, C.L. Perng, H. Chiang, C.T. Lee, F.Y. Chang, et al.; Pseudomelanosis duodeni: report of eight cases; J Formos Med Assoc, 94 (1995), pp. 632–634
- [14] Y.C. Kuo, P.H. Lee, T.H. Lo; Melanosis duodeni: a case report; Endoscopy, 31 (1999), p. S51
- [15] H.H. Yen, Y.Y. Chen, M.S. Soon; Pseudomelanosis duodeni: an unusual find from upper gastrointestinal endoscopy; Clin Gastroenterol Hepatol, 7 (2009), p. e68
- [16] M.H. de Magalhães Costa, G. Fernandes Pegado Mda, C. Vargas, M.E.C. Castro, K. Madi, T. Nunes, et al.; Pseudomelanosis duodeni associated with chronic renal failure; World J Gastroenterol, 18 (2012), pp. 1414–1416
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?