Highlights
- We reviewed 185 PVC catheter ablation cases and identified 17 in which PVCs were successfully ablated in the aortic cusps.
- The MDI measured 0.53 ± 0.10 (median 0.50, IQR 0.47–0.60).
- In all (100%) cases MDI was > 0.40 and in 7 (41%) cases it was > 0.55.
- Pseudo-delta wave was absent in all but one PVC
- PVC origin in the aortic cusps should be considered along with the epicardium when MDI is in the vicinity of 0.55.
Keywords
Aortic cusps;Maximum deflection index;Premature ventricular complex
Electrocardiographic characteristics of premature ventricular complexes (PVC) can be suggestive of their anatomic origin which is pivotal for procedural planning before catheter ablation. The accurate identification of all likely ectopic foci is of even higher importance when an epicardial ablative approach is considered given the associated procedural complexities. Prior studies have identified characteristics associated with epicardial origin of ventricular tachycardia (VT) [1]; [2] ; [3]. Specifically, a large maximum deflection index (MDI) of the VT, which is a metric of the rapidity of depolarization of the myocardium, is thought to indicate epicardial foci. In the Daniels et al. [2] study, MDI ≥ 0.55 had 100% sensitivity and 98.7% specificity for epicardial VT. In the Valles et al. [3] study in patients with non-ischemic cardiomyopathy, however, there was no significant difference in MDI between epicardial and endocardial sites, and MDI ≥ 0.55 had poor sensitivity (33%) and moderate specificity (75%) for epicardial origin. It is possible that other non-epicardial anatomic locations may be characterized by ectopic ventricular foci with a large MDI. The aim of this study was to describe the MDI and morphology of PVCs with earliest point of activation in the aortic cusps.
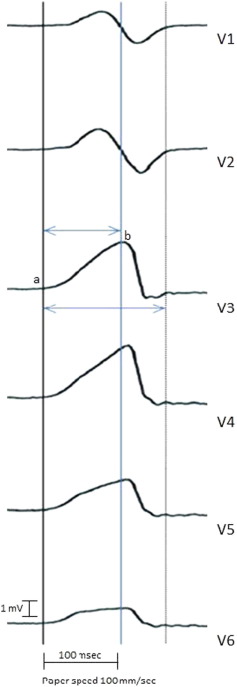
We identified all consecutive cases of idiopathic PVC catheter ablation procedures performed in our Electrophysiology laboratory in 2011–2013 and reviewed CARTO tracings, Prucka recordings and operative reports to identify those where successful ablation of a PVC focus was performed in the aortic cusps. PVC morphology and axis were used to identify the point of origin. Successful ablation was defined as elimination of the ventricular ectopy with intraprocedural observation and attempted induction with isoproterenol infusion. For each case we recorded patient demographic and clinical characteristics (gender, age), the exact anatomic site of successful ablation, and electrocardiographic characteristics based on the 12-lead surface electrocardiogram. Specifically, we documented QRS duration in sinus rhythm and in the PVC (interval between the earliest rapid deflection of the ventricular complex in any of the 12 leads to the latest offset in any lead), PVC QRS morphology in lead V1, net amplitude in leads I and aVF, precordial transition in sinus rhythm and PVC, presence of pseudo-delta wave in the PVC (determined by two independent investigators with 100% agreement), and the MDI of the PVC. The MDI was calculated by dividing the time from onset of the QRS complex to the earliest point of maximum deflection (positive or negative) in the precordial leads by the QRS duration (Fig. 1) [2] ; [3]. Electrocardiographic interval measurements were performed with electronic calipers that were placed manually on Prucka recordings. All assessments pertained to the dominant morphology high-density PVC that was repeatedly observed in the electrophysiology laboratory in isolation and not in couplets or VT runs. The above characteristics and electrocardiographic measurements are reported per patient and summarized as frequencies and percentages for categorical variables, and means and standard deviations (SD) or medians and interquartile ranges (IQR) for continuous variables. All patients had provided research consent. This study was approved by the Mayo Clinic Institutional Review Board.
|
|
|
Fig. 1. Calculation of the maximum deflection index. The maximum deflection index was calculated by dividing the time from onset of the QRS complex (point a) to the earliest point of maximum deflection (point b) in the precordial leads by the QRS duration (large double arrow). |
We identified 185 cases of successful or attempted catheter ablation of symptomatic PVCs of patients in whom pharmacologic management had failed. In 17 of those patients (mean age 56.9 ± 15 years, 8 females) PVCs were successfully ablated in the aortic cusps. Sustained elimination of ventricular ectopy as defined by Holter monitoring or symptom resolution was observed in 15 of 16 (94%) patients with available post-ablation follow-up (median 88 days). As shown in Table 1, the left coronary cusp (LCC) was the most common PVC origin (n = 12), followed by the right coronary cusp (RCC) (n = 4) and the RCC–LCC commissure (n = 1). rS was the most common QRS PVC morphology in V1 (in 14 cases). Mean QRS duration was 88 ± 8 ms in sinus rhythm and 137 ± 12 ms for the PVCs. Pseudo-delta wave was absent in all but one PVC, which originated from the RCC.
| Patient | Age (years) | Gender | Successful site | PVC V1 morphology | SR QRS width (ms) | PVC QRS width (ms) | Net amp I (mV) | Net amp aVF (mV) | Precordial transition SR | Precordial transition PVC | MDI | Pseudodelta |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 54 | F | LCC | rS | 82 | 148 | 0.24 | 1.32 | V3–V4 | V1 | 0.48 | No |
| 2 | 21 | F | LCC | rS | 86 | 128 | − 0.48 | 1.68 | V4 | V4 | 0.58 | No |
| 3 | 64 | F | LCC | rS | 86 | 146 | 0.16 | 1.60 | V3 | V4 | 0.68 | No |
| 4 | 64 | M | LCC | rS | 94 | 162 | 0.12 | 1.40 | V2 | V3 | 0.59 | No |
| 5 | 75 | F | LCC | qR | 86 | 125 | 0 | 1.24 | V4 | V2 | 0.45 | No |
| 6 | 42 | F | RCC–LCC commissure | rS | 82 | 123 | − 0.53 | 1.67 | V4 | V2 | 0.46 | No |
| 7 | 72 | F | LCC | qS | 92 | 146 | − 0.32 | 2.72 | V5 | V4 | 0.66 | No |
| 8 | 42 | M | RCC | rS | 94 | 128 | 1.36 | 1.36 | V2 | V2 | 0.61 | Yes |
| 9 | 65 | M | LCC | Rs | 88 | 146 | 0.64 | 1.32 | V4 | V1 | 0.49 | No |
| 10 | 59 | M | LCC | rS | 82 | 131 | 0.24 | 1.68 | V3 | V3 | 0.28 | No |
| 11 | 52 | M | RCC | rS | 84 | 125 | 1.24 | 1.79 | V4 | V3 | 0.66 | No |
| 12 | 72 | M | LCC | rS | Paced rhythm | 143 | 1.51 | 0.93 | V2 | V3 | 0.56 | No |
| 13 | 66 | M | LCC | rS | 96 | 130 | − 0.36 | 1.98 | V4 | V3 | 0.50 | No |
| 14 | 77 | M | RCC | rS | 108 | 131 | 0.12 | 1.56 | V3 | V2 | 0.50 | No |
| 15 | 42 | F | LCC | rS | 74 | 121 | − 0.12 | 1.64 | V4 | V3 | 0.46 | No |
| 16 | 57 | F | RCC | rS | 80 | 150 | 0.64 | 0.80 | V3 | V4 | 0.52 | No |
| 17 | 44 | M | LCC | rS | 90 | 140 | − 1.08 | 4.88 | V2 | V3 | 0.49 | No |
Abbreviations: PVC, premature ventricular complex; SR, sinus rhythm; MDI, maximum deflection index; RCC, right coronary cusp; LCC, left coronary cusp; M, male; F, female.
MDI ranged from 0.28 to 0.68 (mean 0.53 ± 0.10, median 0.50, IQR 0.47–0.60). In all (100%) cases MDI was > 0.40 and in 7 (41%) cases it was > 0.55. There was no statistically significant difference in the MDIs of PVCs originating from the LCC and the RCC. The MDI in the PVC with a pseudo-delta wave was 0.61.
MDI values exceeding 0.55 are considered suggestive of epicardial VT sites. It should be cautioned, however, that endocardial sites may have similarly large MDIs under certain circumstances due to delayed initial conduction, such as in cases of VT foci distant from the His-Purkinje system (i.e. lateral left ventricle) [3]. The value of such an MDI cut-off in distinguishing epicardial from endocardial sites may be limited in these cases. Herein we demonstrate that PVCs originating in the aortic cusps can also be characterized by large MDIs, occasionally resembling the characteristics of epicardial sites. The large MDI of aortic cusp VT may be suggestive of delayed conduction through the aortic valve apparatus to the myocardium. Our finding of large MDI in aortic cusp PVCs is in concordance with a previous report by Yamada et al. [4] In this report of 29 patients with idiopathic VT or PVCs from the LCC, MDI was > 0.55 in 27% cases, and on average MDIs of LCC ectopic foci were larger than those of the aortomitral continuity but smaller than epicardial ones. Also, in agreement with a recent study where pseudo-delta waves were significantly more common in epicardial than endocardial VT [5], a pseudo-delta wave was absent in almost all PVCs arising from the aortic cusps in our case series. Among the limitations of our study are the small sample size and the possibility that some of the PVCs targeted endocardially in the aortic cusps could have in fact represented epicardial foci. Other groups have demonstrated that it is possible to eliminate epicardial foci with endocardial ablation and thus this possibility cannot be eliminated [6].
In conclusion, PVC origin in the aortic cusps should be considered along with the epicardium when MDI is in the vicinity of 0.55, especially in the absence of a pseudo-delta wave.
Conflict of interest
None.
Funding
None.
Acknowledgments
None.
References
- [1] A. Berruezo, L. Mont, S. Nava, E. Chueca, E. Bartholomay, J. Brugada; Electrocardiographic recognition of the epicardial origin of ventricular tachycardias; Circulation, 109 (2004), pp. 1842–1847
- [2] D.V. Daniels, Y.Y. Lu, J.B. Morton, P.A. Santucci, J.G. Akar, A. Green, et al.; Idiopathic epicardial left ventricular tachycardia originating remote from the sinus of valsalva: electrophysiological characteristics, catheter ablation, and identification from the 12-lead electrocardiogram; Circulation, 113 (2006), pp. 1659–1666
- [3] E. Valles, V. Bazan, F.E. Marchlinski; ECG criteria to identify epicardial ventricular tachycardia in nonischemic cardiomyopathy; Circ Arrhythm Electrophysiol, 3 (2010), pp. 63–71
- [4] T. Yamada, H.T. McElderry, T. Okada, Y. Murakami, H. Doppalapudi, N. Yoshida, et al.; Idiopathic left ventricular arrhythmias originating adjacent to the left aortic sinus of valsalva: electrophysiological rationale for the surface electrocardiogram; J Cardiovasc Electrophysiol, 21 (2010), pp. 170–176
- [5] S.R. Piers, R. Silva Mde, G.F. Kapel, S.A. Trines, M.J. Schalij, K. Zeppenfeld; Endocardial or epicardial ventricular tachycardia in nonischemic cardiomyopathy? The role of 12-lead ECG criteria in clinical practice; Heart Rhythm, 11 (2014), pp. 1031–1039
- [6] Y. Komatsu, M. Daly, F. Sacher, H. Cochet, A. Denis, N. Derval, et al.; Endocardial ablation to eliminate epicardial arrhythmia substrate in scar-related ventricular tachycardia; J Am Coll Cardiol, 63 (2014), pp. 1416–1426
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?