Abstract
Aims
To develop the Discharge Planning of Ward Nurses (DPWN), a Japanese self-evaluation instrument for ward nurses' discharge planning practices.
Design
Cross-sectional survey.
Methods
Participants were 624 ward nurses from six hospitals in Japan with a discharge planning department. Items about discharge planning practices were collected from literature and interviews with nurses and researchers. Construct validity, concurrent validity, internal consistency and test–retest reliability were tested.
Results
Initially, 55 items were collected. Examination of the floor effect, item-total, good–poor analyses and exploratory factor analysis yielded a four-factor model with 24 items (‘teaching home-care skills with community/hospital professionals,’ ‘identifying clients’ potential needs early in the discharge process,’ ‘introducing social resources’ and ‘identifying client/family wishes and building consensus for discharge’). The four-factor structure was supported by confirmatory factor analysis. The DPWN correlated with scales ascertaining similar concepts, supporting concurrent validity. Internal consistency and test–retest reliability were generally satisfactory.
Introduction
Hospital admissions increase with advancing age (Hall et al. 2010) and so does total healthcare expenditure, especially in Japan where the ageing of the population is among the most rapid in the world (Ministry of Health, Labour and Welfare 2011). The health insurance system was reformed in 2003 to address the spiralling costs and the healthcare system has shifted from being hospital based to community based (Ministry of Health, Labour and Welfare 2003).
As part of this shift in the healthcare system, enormous efforts have been attempted to shorten the average length of hospital stay (Sato & Fushimi 2009). As a result of this shortened length of hospital stay, older adult patients often leave the hospital with altered independence levels and vulnerable health conditions. These older adults frequently have difficulty when leaving the hospital (Buurman et al. 2011, Coffey & McCarthy 2013). In Japan, older clients and their families often become anxious when leaving hospital and it has been reported that some may feel resentful because they feel they were rushed out of the hospital (Koyama & Kobayashi 2012).
In this climate, careful planning is vital for smooth discharge and there are various discharge planning systems worldwide. In Japan, independent discharge planning departments with nurses and/or medical social workers support patients who are a high risk of discharge delay (Ministry of Health, Labour and Welfare 2008). The staff assist the identified patient and family decide when they leave the hospital and where they go to (e.g. long-term care or hospitals, or home), search for long-term care facilities/hospitals on their behalf and coordinate smooth transition in cooperation with a variety of professionals, such as nurses or social workers in the community or in facilities/hospitals (Tomura et al. 2011). Other countries have discharge specialists, such as nurse practitioners or clinical nurse specialists, who play a similar role (Forster et al. 2005, Coleman et al. 2006), or a discharge specialist team may be available (Sheppard et al. 2010).
Regardless of the various arrangements for discharge planning, ward nurses also play a key role in efficient discharge planning (Foust 2007, Suzuki et al. 2012). They are at the frontline of patient care and they are the ones who ascertain the needs of those high-risk patients, take the initial action and refer them to the discharge planning department/specialist/team. However, ward nurses are still largely unfamiliar with discharge planning, especially in Japan where discharge planning is a rapidly introduced concept. Ways to help ward nurses provide more effective services for patient discharge have been explored in Japan and other countries (Ornstein et al. 2011, Sakai et al. 2011).
Several guidelines on discharge planning have been published (Lees 2010, Agency for Healthcare Research and Quality 2013), but guidelines themselves cannot be used for self-evaluation; rather, the use of self-evaluating instruments is to improve clinical practice (Campbell & Mackay 2001). However, the currently available self-evaluation instruments were either prepared for discharge planning departments (Tomura et al. 2013) or were developed before discharge planning departments were introduced (Chiba 2005). A new self-evaluation tool that better fits with the current discharge planning practices that guide ward nurses would be beneficial.
To date, many guidelines have been conducted in Western environments (e.g. Royal College of Nursing 2010, Agency for Healthcare Research and Quality 2013). Nurses in Japan and other countries outside Western culture might find it difficult to apply the Western idea of discharge planning in their cultural environments. For example, in Japan family ties and family involvement play a crucial role in decision-making about health-related issues. Caregiving is often perceived as an important familial and societal obligation, whereas in the United States greater emphasis is placed on maintaining clients’ independence and respecting their autonomy (Tanji et al. 2013). Client and healthcare personnels expectations of healthcare services and assistance in discharge planning might well differ from country to country (Sentell et al. 2013). The new self-evaluation instrument needs to reflect practice in Japan; the scale may also fit discharge planning in other non-Western countries.
Based on the above literature review, this study aimed to develop an instrument for ward nurses to self-evaluate their discharge planning practices in Japan, where many hospitals own an independent discharge planning department. It might enable ward nurses to self-evaluate their own discharge planning practices to improve them and assess the effectiveness of any educational programmes for ward nurses. It could also be used in other countries where hospitals have a discharge department/specialist/team.
Method
The study was conducted to develop the Discharge Planning of Ward Nurses (DPWN) scale, a Japanese instrument for ward nurses to self-evaluate their discharge planning practices. The study consists of item development and validity and reliability testing.
Item development
To develop the items for the DPWN, we first reviewed the literature in Japanese and international databases (i.e. PubMed, CINAHL and the Japan Medical Abstract Society database) using the keywords ‘discharge planning,’ ‘transitional care,’ ‘nursing’ and ‘cooperation.’ We also interviewed 19 registered nurses and two researchers specializing in discharge planning to obtain items on actual practices in discharge planning, asking ‘What would you do as a ward nurse to best support your clients during discharge?’ In this way, we attempted to collect a range of actual practices deemed necessary for ward nurses to give effective assistance. These nurses had more than 10 years’ ward experiences and had worked in a discharge planning department for more than 2 years. The literature review and interviews yielded 55 items for the DPWN and this list underwent statistical analyses using the survey data.
Validity and reliability testing
Participants
The survey participants were all ward nurses from six acute care general hospitals in central Japan (n = 624). These hospitals were a convenience sample, had 300–550 beds and an average length of hospital stay of 14 days, which showed that they were typical urban, middle-to-large-sized general acute care hospitals. All ward nurses at the six hospitals were contacted about possible participation in this study. Sample size was determined using the general rule for factor analytic procedure that requires a minimum of 10 respondents per item (Kline 1998).
Measures
The questionnaire included the following: (1) demographic and professional characteristics; (2) the 55 items for the DPWN; and (3) the Discharge Planning-Process Evaluation Measurement (DCP-PEM; Chiba 2005), the Oriented Problem Solving Behavior in Nursing Practice scale (OPSN; Sadahiro & Yamashita 2002) and a Visual Analogue Scale (VAS) evaluating their own discharge planning practices, all for concurrent validity testing.
The demographic and professional characteristics included age, gender, years of clinical experience, current position and educational background. The 55 items for the DPWN about self-evaluating discharge planning began with the stem ‘How do you evaluate your practice with regard to each of the following practices in discharge planning?’ with answers recorded on a 6-point Likert scale ranging from 1 (poor)–6 (excellent).
The following three scales were used for concurrent validity testing. The DCP-PEM was developed in Japanese by Chiba in 2005 to self-evaluate the discharge planning for the interdisciplinary team, not specific to ward nurses (Chiba 2005). The DCP-PEM was used because it was the best, currently available instrument to self-evaluate discharge planning practice; even though it was developed before discharge planning departments became common in Japan, the items included work that is now undertaken in Japans discharge planning departments. It consisted of 26 items using a 5-point Likert scale, with higher scores representing more effective discharge planning. Cronbachs alpha was 0·97 in this study.
The OPSN was developed by Sadahiro and Yamashita (2002) for ward nurses to self-evaluate nursing practice in general. The OPSN was used for concurrent validity testing because it was expected that good practices in general would correspond to good discharge planning practices. The OPSN consisted of 25 items with five domains and 5-point Likert scale and higher scores represented better practice. Cronbachs alpha was 0·97 in this study.
A VAS scale asking ‘How satisfied are you with your own discharge planning practices?’ was used because there is no gold standard to evaluate the discharge planning practices of ward nurses and it is simple, relatively easy to use and provides continuous data (De Vellis 2003, Coll et al. 2004). A continuous 100 mm rating scale ranging from ‘not satisfied at all’ to ‘completely satisfied’ was provided and scores were obtained by measuring the distance in millimetres from the left anchor to each participants mark on the line.
Data collection procedure
Researchers explained this study to the nursing managers. When they agreed to participate, the nursing managers were asked to forward questionnaires to their ward nurses. Once the ward nurses agreed to participate in this study, they completed the self-administered questionnaires, placed their completed questionnaires in a sealed envelope and returned it to the researcher. To evaluate test–retest reliability, ward nurses from two of the six hospitals (n = 195) were asked to complete the questionnaire again after an interval of 2 weeks. During the 2-week interval, participants did not participate in any trainings, seminars or educational activities. We collected data from November–December 2011.
Analysis
First, after examining the response distribution for extreme skewness (Tanimura et al. 2011), we conducted good–poor (G-P) analysis (Hou et al. 2011) and the item-total (I-T) (Ferketich 1991) and also examined internal correlations (Ushiro 2009). In these analyses, we eliminated items with extreme skewness, non-significance to distinguish good and poor groups, non-significant association to the total score and high internal correlation (>0·7). We then conducted exploratory factor analysis with the maximum-likelihood method and promax rotation to explore the underlying structure in discharge planning practice. Missing data were supplemented by the median of each item (Schaefer & Graham 2002). The number of factors was determined based on the interpretability of each factor, the number of eigenvalues greater than 1·0 and the scree plot. Items were further eliminated for parsimony when factor loadings were less than 0·45 and when communalities were less than 0·40 (Polit & Beck 2011). At this point, the final items and the subscales for the DPWN (with 24 items and a four-factor structure) were determined.
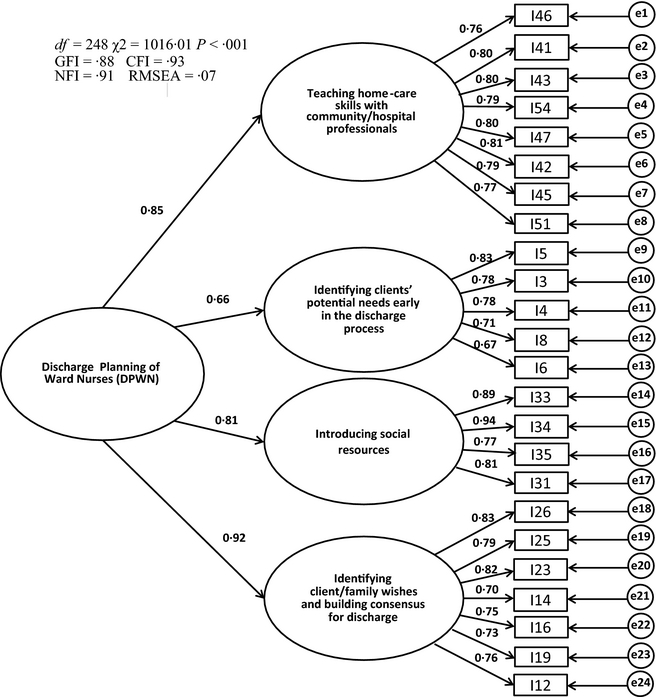
Next, we conducted a range of validity and reliability examinations: construct and concurrent validity, internal consistency and test–retest reliability. To examine construct validity, we assessed whether the subscales could be subsumed into the second-order, overall model of discharge planning practice using a confirmatory factor analysis. We used the goodness of fit index (GFI), comparative fit index (CFI), normed fit index (NFI) and root mean square error of approximation (RMSEA) (Kaariainen et al. 2011).
We examined concurrent validity by testing the associations of the subscale and total DPWN scores with the DCP-PEM, OPSN and VAS, using Pearsons correlation coefficients. Finally, we calculated Cronbachs alphas to assess internal consistency and intra-class correlation coefficients (ICC) for test–retest reliability (McDonald 1981). The ICC was calculated using a two-way random effects model (Terwee et al. 2007). All statistical analyses were performed using SPSS version 18.0J and AMOS version 20 (IBM SPSS Japan, Tokyo, Japan).
Ethics
Participants were informed of the purpose and methods of the study, risks and benefits of participation, confidentiality of their data and voluntary nature of participation. Written informed consent was obtained before the interviews for the item development and refinement study. The return of the anonymous questionnaire was taken as consent to participate in the main study. The study protocol conformed to the Declaration of Helsinki (as revised in Edinburgh 2000) and the study process was reviewed and approved by the ethics committee of Tokyo Womens Medical University and the administrators of the participating hospitals.
Results
Participant characteristics
In total, 772 questionnaires were distributed and 641 returned (response rate 83·0%). Among them, 624 questionnaires with missing data less than 5% of the total items were used (valid response rate 80·8%). Participants were on average 33·5 years old (sd 8·6), with an average of 9·3 years (sd 7·5) of nursing experience; 96% of them were female (Table 1).
| N | % | |
|---|---|---|
| Mean age, years (Mean, sd) | 33·5 | (8·6) |
| Mean nursing practice duration, years (Mean, sd) | 9·3 | (7·5) |
| Gender | ||
| Female | 600 | (96·2) |
| Male | 24 | (3·8) |
| Position | ||
| Staff nurses | 570 | (91·3) |
| Sub nursing chiefs | 37 | (5·9) |
| Nursing chiefs | 15 | (2·4) |
| Others | 2 | (0·3) |
| Academic background | ||
| Diploma | 497 | (79·7) |
| Associates degree | 52 | (8·3) |
| Bachelors degree | 54 | (8·7) |
| Graduate programme | 7 | (1·1) |
| Others | 14 | (2·2) |
| sd, Standard Deviation. | ||
Item selection and subscale development
Among the collected 55 items for the DPWN, no items were eliminated due to skewed distributions or through the G-P analyses. Pearsons correlation coefficients in the I-T analyses ranged from 0·50–0·79 except for one item that was dropped from the subsequent analyses. An additional 15 items were eliminated because of high correlations (>0·7) with other items. After these item-level analyses, 39 items remained.
In the following exploratory factor analyses, the scree plot and parallel analysis suggested four factors and they were considered appropriate conceptually as well. Using the four-factor model, we eliminated 11 items due to low factor loadings or communalities and further dropped four items due to content redundancy or item vagueness. The resultant final DPWN contained 24 items and the four subscales were named as follows: (1) ‘teaching home-care skills with community/hospital professionals’; (2) ‘identifying clients’ potential needs early in the discharge process’; (3) ‘introducing social resources’; and (4) ‘identifying client/family wishes and building consensus for discharge’ (Table 2). The DPWNs mean item scores were between 2·82-4·61 (Table 3).
| Item | Subscale 1 | Subscale 2 | Subscale 3 | Subscale 4 | Communality | ||
|---|---|---|---|---|---|---|---|
| Subscale 1 Providing discharge guidance in cooperation with community support team and multidisciplinary team | |||||||
| I46 | Teaching a patient and his/her family medical treatment consistently with staff members. | 0·877 | 0·054 | −0·213 | 0·030 | 0·632 | |
| I41 | Working with a doctor and pharmacist to simplify the administration of intravenous drip injections and internal medicines to make it manageable for a patient and his/her family. | 0·851 | −0·001 | −0·116 | 0·048 | 0·655 | |
| I43 | Consulting with a nutritionist or nutrition support team (NST) about eating at home and nutrition. | 0·807 | −0·021 | 0·093 | −0·077 | 0·658 | |
| I54 | Preparing for home medical care (e.g. providing information about purchasing medical supplies, coordination with relevant medical institutions, etc.). | 0·755 | 0·024 | 0·122 | −0·079 | 0·636 | |
| I47 | Checking if a patient and his/her family understand what they should do in case of an abnormal condition or emergency at home. | 0·723 | −0·048 | −0·051 | 0·189 | 0·652 | |
| I42 | Working with a rehabilitation staff member to teach a patient and his/her family how to perform ADL in the environment after discharge. | 0·684 | 0·042 | 0·111 | 0·034 | 0·655 | |
| I45 | Working with a discharge coordinator to arrange medical treatment that is appropriate for a patients life. | 0·679 | −0·050 | 0·159 | 0·027 | 0·631 | |
| I51 | Passing information about a patients potential problems at home to the care manager, visiting doctor, visiting nurse, caregiver and public health nurse at a discharge case conference. | 0·614 | −0·046 | 0·198 | 0·050 | 0·606 | |
| Subscale 2 Collecting information from the client/family | |||||||
| I5 | Collecting information about a patients ADL, cognition and understanding level. | 0·127 | 0·947 | −0·056 | −0·184 | 0·771 | |
| I3 | Collecting information about a patients living conditions (ADL, cognitive level, dwelling environment, etc.) prior to hospitalization. | 0·000 | 0·822 | 0·116 | −0·142 | 0·605 | |
| I4 | Collecting information about a patients disease, progress and prognosis. | 0·000 | 0·674 | −0·076 | 0·194 | 0·611 | |
| I8 | Collecting information about a patients family make-up, relationship with them and (possibly informal) key person. | −0·072 | 0·586 | −0·020 | 0·227 | 0·497 | |
| I6 | Collecting information about a patients social background (life history, occupation, faith, hobbies, etc.). | −0·194 | 0·529 | 0·154 | 0·241 | 0·465 | |
| Subscale 3 Assisting to use social resources | |||||||
| I33 | Informing a patient and his/her family who can benefit from, how to apply for and what services are available through the Long-term Care Insurance System. | 0·074 | 0·090 | 0·892 | −0·121 | 0·808 | |
| I34 | Informing a patient and his/her family, as required, who is eligible for and how to apply for home visits by a doctor or nurse. | 0·095 | 0·019 | 0·848 | 0·018 | 0·872 | |
| I35 | Informing a patient and his/her family, as required, of the percentage of the medical payments paid by patients in the Public Assistance System. | −0·101 | −0·017 | 0·813 | 0·072 | 0·621 | |
| I31 | Finding out what services supporting in-home long-term medical care are available in the municipality where a patient resides. | 0·171 | −0·065 | 0·539 | 0·246 | 0·685 | |
| Subscale 4 Supporting decision-making process | |||||||
| I26 | Checking if there is any difference in the future directions that a patient, his/her family and medical staff have in mind. | 0·000 | −0·025 | 0·004 | 0·867 | 0·730 | |
| I25 | Informing a patient and his/her family of the function and role of their current hospital. | 0·009 | −0·078 | 0·151 | 0·740 | 0·649 | |
| I23 | Informing a patient and his/her family of prospective changes in life due to the disease. | 0·062 | 0·002 | 0·049 | 0·736 | 0·665 | |
| I14 | Providing an opportunity for a patient and his/her family to be informed of their condition by the doctor according to their level of understanding. | 0·056 | 0·190 | −0·129 | 0·616 | 0·514 | |
| I16 | Reviewing the potential problems that a patient is likely to encounter according to his/her ADL. | 0·095 | 0·223 | −0·033 | 0·552 | 0·582 | |
| I19 | Sharing the wishes of a patient and his/her family with the doctor and discussing future directions. | 0·143 | 0·087 | 0·030 | 0·543 | 0·533 | |
| I12 | Understanding how a patient and his/her family feel about discharge from hospital and how they wish to spend their life from now on. | 0·074 | 0·228 | 0·064 | 0·483 | 0·556 | |
The English translation of the items has not been psychometrically tested.
The English translation of the items has not been psychometrically tested. a Maximum-likelihood method with promax rotation. The English translation of the items has not been psychometrically tested. a Maximum-likelihood method with promax rotation. DPWN, Discharge Planning of Ward Nurses. | |||||||
| Item | Mean | sd | |
|---|---|---|---|
| Subscale 1 Teaching home-care skills with community/hospital professionals | 28·67 | 8·16 | |
| I46 | Teaching a patient and his/her family medical treatment …….. | 4·06 | 1·09 |
| I41 | Working with a doctor and pharmacist to simplify …………… | 3·72 | 1·23 |
| I43 | Consulting with a nutritionist or nutrition support team………. | 3·40 | 1·28 |
| I54 | Preparing for home medical care (e.g. providing information…. | 3·52 | 1·29 |
| I47 | Checking if a patient and his/her family understand what……… | 3·65 | 1·14 |
| I42 | Working with a rehabilitation staff member to teach a patient… | 3·64 | 1·27 |
| I45 | Working with a discharge coordinator to arrange medical…….. | 3·42 | 1·23 |
| I51 | Passing information about a patients potential problems……. | 3·27 | 1·42 |
| Subscale 2 Identifying clients’ potential needs early in the discharge process | 22·14 | 3·31 | |
| I5 | Collecting information about a patients ADL and cognition…… | 4·61 | 0·76 |
| I3 | Collecting information about a patients living conditions……… | 4·45 | 0·86 |
| I4 | Collecting information about a patients disease, progress and…. | 4·39 | 0·78 |
| I8 | Collecting information about a patients family make-up……… | 4·53 | 0·83 |
| I6 | Collecting information about a patients social background……. | 4·17 | 0·88 |
| Subscale 3 Introducing social resources | 12·45 | 4·30 | |
| I33 | Informing a patient and his/her family who can benefit from…… | 3·21 | 1·26 |
| I34 | Informing a patient and his/her family, as required, who is…….. | 3·13 | 1·23 |
| I35 | Informing a patient and his/her family, as required…………….. | 2·82 | 1·17 |
| I31 | Finding out what services supporting in-home long-term…….. | 3·29 | 1·17 |
| Subscale 4 Identifying client/family wishes and building consensus…. | 27·63 | 5·58 | |
| I26 | Checking if there is any difference in the future directions that…. | 3·85 | 0·96 |
| I25 | Informing a patient and his/her family of the function and role…. | 3·67 | 1·06 |
| I23 | Informing a patient and his/her family of prospective changes….. | 3·91 | 0·99 |
| I14 | Providing an opportunity for a patient and his/her family to be….. | 4·13 | 1·02 |
| I16 | Reviewing the potential problems that a patient is likely to……… | 4·16 | 0·89 |
| I19 | Sharing the wishes of a patient and his/her family with the doctor.. | 3·86 | 1·08 |
| I12 | Understanding how a patient and his/her family feel about……… | 4·05 | 0·95 |
| Total score | 90·89 | 18·22 | |
| sd, standard deviation; DPWN, Discharge Planning of Ward Nurses. | |||
Validity and reliability testing
For construct validity testing, the confirmatory factor analysis was performed. The chi-square value was significant (χ2 = 1016·01, d.f. = 248, P < 0·001). The GFI, CFI, NFI and RMSEA were 0·88, 0·93, 0·91 and 0·07 respectively (Figure 1). Concurrent validity was examined by testing the associations of the DPWN scores with the DCP-PEM, OPSN and VAS (Table 4). The subscale and total DPWN showed a statistically significant, positive correlation with the DCP-PEM (r = 0·53–0·81, P < 0·001). They also showed significant correlation with the OPSN (r = 0·28–0·55, P < 0·001); however, the correlation was marginal for the subscale ‘introducing social resources’ (r = 0·28). The subscale and total DPWN had significant correlation with the VAS (r = 0·32–0·53, P < 0·001); again, the correlation was marginal for the subscale ‘identifying clients’ potential needs early in the discharge process’ (r = 0·32).
|
|
|
Figure 1. Model of the 24-item Discharge Planning of Ward Nurses with standardized regression weights and correlations. |
| DCP-PEM | OPSN | Satisfaction (VAS) | |
|---|---|---|---|
| DPWN (total score) | 0·81a | 0·51a | 0·53a |
| Subscale 1: Teaching home-care skills with community/hospital professionals | 0·78a | 0·43a | 0·51a |
| Subscale 2: Identifying clients’ potential needs early in the discharge process | 0·53a | 0·55a | 0·32a |
| Subscale 3: Introducing social resources | 0·63a | 0·28a | 0·43a |
| Subscale 4: Identifying client/family wishes and building consensus for discharge | 0·71a | 0·49a | 0·50a |
|
a P < 0·001, Pearsons correlation coefficient (two-tailed). a P < 0·001, Pearsons correlation coefficient (two-tailed). DPWN, Discharge Planning of Ward Nurses; DCP-PEM, Discharge Planning-Process Evaluation Measurement; OPSN, Oriented Problem Solving Behavior in Nursing Practice; VAS, Visual Analogue Scale. | |||
Cronbachs alpha for the total DPWN was 0·95 and those for the subscale scores ranged from 0·86–0·93 (Table 5). Test–retest reliability by ICC based on the data from 182 nurses was 0·74 (P < 0·001) for the total score and ranged from 0·55–0·69 for the four subscales. The subscales ‘identifying clients’ potential needs early in the discharge process’ and ‘introducing social resources’ did not meet ICC standards (ICC > 0·64) for test–retest reliability (Yen & Lo 2002).
| No. of items | Cronbachs alpha | ICC | |
|---|---|---|---|
| DPWN (Total score) | 24 | 0·95 | 0·74 |
| Subscale 1: Teaching home-care skills with community/hospital professionals | 8 | 0·93 | 0·67 |
| Subscale 2: Identifying clients’ potential needs early in the discharge process | 5 | 0·86 | 0·55 |
| Subscale 3: Introducing social resources | 4 | 0·91 | 0·62 |
| Subscale 4: Identifying client/family wishes and building consensus for discharge | 7 | 0·91 | 0·69 |
| DPWN, Discharge Planning of Ward Nurses; ICC, intra-class correlation coefficients. | |||
Discussion
In this study, the four-factor, 24-item DPWN was developed for the self-evaluation of ward nurses’ discharge planning practices in hospitals with discharge planning departments. The DPWN was developed based on literature review and interviews with practising nurses and researchers and its validity and reliability were examined based on data from 624 nurses. To our knowledge, this is the first attempt to a self-evaluation instrument for ward nurses’ discharge planning practices in Japan.
Validity and reliability
First, the DPWNs content validity was maintained according to the literature review and interviews with practising nurses regarding their actual daily discharge planning. Construct validity was examined by the confirmatory factor analysis and the chi-square test and GFI were marginal while other indices supported the model fit. This is potentially because the chi-square test is very sensitive and can easily reject the model (P < 0·05) when the sample size is large (n > 500–600) (Kaariainen et al. 2011); the GFI is also affected by sample size (Sharma et al. 2005). Given the results for the other fit indices, we considered that the four-factor model of the DPWN showed acceptable construct validity.
Concurrent validity testing revealed that the DCP-PEM and OPSN subscales and the VAS had moderate-to-high correlations with the DPWN, except for the subscale ‘introducing social resources’ and the OPSN and the subscale ‘identifying clients’ potential needs early in the discharge process’ and the VAS. The possible reason is that the OPSN focuses more on traditional inpatient care rather than the issues related to discharge planning. The DPWN might reflect Japans contemporary healthcare situation requiring hospital ward nurses to introduce patients and their families to social resources in addition to providing individual assessment and care. The lack of strong correlation between ‘identifying clients’ potential needs early in the discharge process’ and the VAS may be because participant ward nurses have not learnt enough to consider this subscales contents in relation to discharge planning; this suggests an area of future education for ward nurses.
Finally, Cronbachs alphas were high to adequate for both total and subscale scores. Although we removed some items, Cronbachs alpha remained high. We chose to keep some items so that the ward nurses could self-learn from the items needed in discharge planning practice. The low ICC for the two subscales might be due to the limited number of items in these subscales. The ICC of the total score confirmed the temporal stability of the overall DPWN. Taken together, the results suggest satisfactory overall validity and reliability of the DPWN.
DPWN components
The DPWN contains several important new items that were not used in previous instruments to self-evaluate discharge planning practices, such as discussing anticipated health-related lifestyle changes, sharing information with physicians about the wishes of older clients and their families and discussing future directions with clients. These items belonged to the subscale ‘identifying client/family wishes and building consensus for discharge.’ It has been suggested that ward nurses often need to assess the clients’ situations and competently assist them in the decision-making process before the discharge planning department is involved (Watts et al. 2007, Naylor et al. 2009). The result underlined the importance of ward nurses deliberately taking time to sit with clients and their families and patiently identifying their wishes. They needed to discuss future directions together with clients until they accept the situation and truly agree with the plan. This would allow clients to leave hospital without feeling ‘kicked out.’ Thus, the new items reveal important components of the discharge planning practices of the ward nurses.
Another new key component in the DPWN is ‘introducing social resources.’ This new component also seems to be important, explaining to clients and their families how to apply for resources under the long-term care insurance system. In Japan, 64·8% of clients in acute care hospitals are older people (Ministry of Health, Labour and Welfare 2011), who are most likely to need assistance for discharge planning. Introducing older clients and their families to social resources and reducing the burden of care are vital to help this clientele feel safe when they are home. Ward nurses are reported to have limited knowledge and understanding of the community care system (Robinson & Street 2004, Nakanishi & Morishita 2008). The DPWN should therefore help ward nurses recognize the importance of having knowledge about community care services.
Some components of the DPWN overlap with the existing literature and guidelines for discharge planning, showing that the DPWN encompasses these fundamental needs of the clients at the time of discharge: ‘identifying clients’ potential needs early in the discharge process’ and ‘teaching home-care skills with community/hospital professionals’ (Royal College of Nursing 2010, Agency for Healthcare Research and Quality 2013). Thus, the DPWN has both unique and common for evaluating ward nurses' discharge planning practices.
Study limitations and future research implications
This study has several limitations. First, participants were limited to nurses from the conveniently sampled six hospitals, although we made an effort to collect data from typical general acute care hospitals and nurses with various backgrounds. Future research is needed with nurses from various locations and hospital functions. Second, the DPWN was based solely on self-evaluation; future studies should include objective evaluations by clients and families as well as third parties. Further research is also needed to confirm the DPWNs responsiveness to any interventions and its applicability in other countries.
Conclusion
The study purpose was to develop a new instrument, the DPWN, for use in the self-evaluation of ward nurses' discharge planning. The DPWN showed acceptable validity and reliability.
The DPWN might be used for various purposes, such as to enable ward nurses to self-evaluate their own practices and to assess the effectiveness of educational programmes for ward nurses. Additionally, it might be useful in creating educational tools aimed at developing nurses' discharge planning competencies; moreover, new nurses may also be mentored using the tools, thus aiding the development of an educational pathway. Furthermore, assessing discharge outcomes such as patient/family satisfaction might be possible. More studies are needed to further examine the clinical utility of the DPWN both nationally and internationally.
Implications for practice
- We developed the DPWN, which is expected to contribute to the self-evaluation of ward nurses' discharge planning where the hospital owns the discharge planning department.
- The DPWN might serve as a self-evaluation tool to help ward nurses improve their discharge planning and as an evaluation tool for educational programmes for ward nurses.
Acknowledgments
The researchers thank Dr. T. Mizuno, Professor of Tokyo Womens Medical University, Dr. K. Takasaki, Commissioner of the Japan Academy for the Prevention of Elder Abuse, and the nurses who participated in this study.
Conflict of interest
No conflict of interest has been declared by the author.
Author contributions
All authors have agreed on the final version and meet at least one of the following criteria [recommended by the ICMJE (http://www.icmje.org/recommendations/)]:
- substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content.
References
- Agency for Healthcare Research and Quality (2013) Care Transitions from Hospital to Home: IDEAL Discharge Planning Implementation Handbook. Retrieved from http://www.ahrq.gov/professionals/systems/hospital/engagingfamilies/strategy4/Strat4_Implement_Hndbook_508_v2.pdf on 25 March 2014.
- Buurman B.M., Hoogerduijn J.G., De Haan R.J., Abu-Hanna A., Lagaay A.M., Verhaar H.J., Schuurmans M.J., Levi M. & De Rooij S.E. (2011) Geriatric conditions in acutely hospitalized older patients: prevalence and one-year survival and functional decline. PLoS ONE6(11), e26951.
- Campbell B. & Mackay G. (2001) Continuing competence: an Ontario nursing regulatory program that supports nurses and employers. Nursing Administration Quarterly25(2), 22–30.
- Chiba Y. (2005) Development and validation of the discharge planning-process evaluation measurement. Japan Academy of Nursing Science25(4), 39–51. (in Japanese).
- Coffey A. & McCarthy G.M. (2013) Older peoples perception of their readiness for discharge and postdischarge use of community support and services. International Journal of Older People Nursing8, 104–115.
- Coleman E.A., Parry C., Chalmers S. & Min S.J. (2006) The care transitions intervention: results of a randomized controlled trial. Archives of Internal Medicine166(17), 1822–1828.
- Coll A.M., Ameen J.R. & Mead D. (2004) Postoperative pain assessment tools in day surgery: literature review. Journal of Advanced Nursing46, 124–133.
- De Vellis R.F. (2003) Scale Development: Theory and Applications, 2nd edn. Sage Publications, Thousand Oaks, CA.
- Ferketich S. (1991) Focus on psychometrics. Aspects of item analysis. Research in Nursing & Health14, 165–168.
- Forster A.J., Clark H.D., Menard A., Dupuis N., Chernish R., Chandok N., Khan A., Letourneau M. & van Walraven C. (2005) Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. The American Journal of Medicine118(10), 1148–1153.
- Foust J.B. (2007) Discharge planning as part of daily nursing practice. Applied Nursing Research20, 72–77.
- Hall M.J., Defrances C.J., Williams S.N., Golosinskiy A. & Schwartzman A. (2010) National Hospital Discharge Survey: summary 2007. National Health Statistics Reports.24, 1–20.
- Hou X., Zhu D. & Zheng M. (2011) Clinical Nursing Faculty Competence Inventory – development and psychometric testing. Journal of Advanced Nursing67, 1109–1117.
- Kaariainen M., Kanste O., Elo S., Polkki T., Miettunen J. & Kyngas H. (2011) Testing and verifying nursing theory by confirmatory factor analysis. Journal of Advanced Nursing67, 1163–1172.
- Kline R.B. (1998) Principles and Practice of Structural Equation Modeling. Guilford Press, New York.
- Koyama H. & Kobayashi K. (2012) Study of discharge planning offered by medical professionals to elderly patients with cerebrovascular diseases and preferred discharge destinations confirmed by primary nurses. Journal of Japan Academy of Home Care16(1), 100–106. (in Japanese).
- Lees L. (2010) Exploring the principles of best practice discharge to ensure patient involvement. Nursing Times106(25), 10–14.
- McDonald R.P. (1981) The dimensionality of tests and items. British Journal of Mathematical and Statistical Psychology34, 100–117.
- Ministry of Health, Labour and Welfare (2003) Reform health-care delivery system. Retrieved from http://www.mhlw.go.jp/houdou/2003/04/h0430-3a.html (in Japanese) on 25 March 2014.
- Ministry of Health, Labour and Welfare (2008) Shinryouhoushuu no Senteihouhou. Retrieved from http://www.mhlw.go.jp/topics/2008/03/tp0305-1.html (in Japanese) on 25 March 2014.
- Ministry of Health, Labour and Welfare (2011) Patients' Survey. Retrieved from http://www.mhlw.go.jp/stf/shingi/2r985200000264pr-att/2r98520000026500.pdf (in Japanese) on 25 March 2014.
- Nakanishi J. & Morishita M. (2008) Awareness of the roles of nurses in regional collaboration and their motivation and self-efficacy. Health Science Research20(2), 9–18. (in Japanese).
- Naylor M.D., Feldman P.H., Keating S., Koren M.J., Kurtzman E.T., Maccoy M.C. & Krakauer R. (2009) Translating research into practice: transitional care for older adults. Journal of Evaluation in Clinical Practice15, 1164–1170.
- Ornstein K., Smith K.L., Foer D.H., Lopez-Cantor M.T. & Soriano T. (2011) To the hospital and back home again: a nurse practitioner-based transitional care program for hospitalized homebound people. Journal of the American Geriatrics Society59, 544–551.
- Polit D.F. & Beck C.T. (2011) Nursing Research, International Edition: Generating and Assessing Evidence for Nursing Practice, 9th edn. Lippincott Williams & Wilkins, Philadelphia, PA.
- Robinson A. & Street A. (2004) Improving networks between acute care nurses and an aged care assessment team. Journal of Clinical Nursing13, 486–496.
- Royal College of Nursing (2010) Discharge Planning. Retrieved from http://rcnpublishing.com/userimages/ContentEditor/1373367855606/Discharge-planning.pdf on 25 March 2014.
- Sadahiro W. & Yamashita N. (2002) Development of an instrument ‘Self-evaluation Scale of Oriented Problem Solving Behavior in Nursing Practice (OPSN)’. Japan Journal of Nursing Research35(6), 15–26. (in Japanese).
- Sakai S., Nakada H., Ryu S., Inukai K., Hattori M. & Ohori Y. (2011) How nurses at special functioning hospitals perform in-home care: analysis of years of nursing experience and comparison of ward nurses and outpatient nurses. Journal of Nursing Research Colloquium of Tokyo Womens Medical University6(1), 41–51. (in Japanese).
- Sato E. & Fushimi K. (2009) What has influenced patient health-care expenditures in Japan?: variables of age, death, length of stay and medical care. Health Economics18(7), 843–853.
- Schaefer J.L. & Graham J.W. (2002) Missing data: our view of the state of the art. Psychological Methods7, 147–177.
- Sentell T.L., Ahn H.J., Juarez D.T., Tseng C.W., Chen J.J., Salvail F.R., Miyamura J. & Mau M.L. (2013) Comparison of potentially preventable hospitalizations related to diabetes among Native Hawaiian, Chinese, Filipino and Japanese elderly compared with whites, Hawai'i, December 2006-December 2010. Preventing Chronic Disease10, E123.
- Sharma S., Mukherjee S., Kumar A. & Dillon W.R. (2005) A simulation study to investigate the use of cutoff values for assessing model fit in covariance structure models. Journal of Business Research58, 935–943.
- Sheppard L.A., Anaf S. & Gordon J. (2010) Patient satisfaction with physiotherapy in the emergency department. International Emergency Nursing18(4), 196–202.
- Suzuki S., Nagata S., Zerwekh J., Yamaguchi T., Tomura H., Takemura Y. & Murashima S. (2012) Effects of a multi-method discharge planning educational program for medical staff nurses. Japan Journal of Nursing Science9, 201–215.
- Tanimura C., Morimoto M., Hiramatsu K. & Hagino H. (2011) Difficulties in the daily life of patients with osteoarthritis of the knee: scale development and descriptive study. Journal of Clinical Nursing20, 743–753.
- Tanji H., Koyama S., Wada M., Kawanami T., Kurita K., Tamiya G., Saito N., Suzuki K., Kato T., Anderson K.E., Gruber-Baldini A.L., Fishman P.S., Reich S.G., Weiner W.J. & Shulman L.M. (2013) Comparison of caregiver strain in Parkinsons disease between Yamagata, Japan and Maryland, the United States. Parkinsonism & Related Disorders19, 628–633.
- Terwee C.B., Bot S.D., de Boer M.R., van der Windt D.A., Knol D.L., Dekker J., Bouter L.M. & de Vet H.C. (2007) Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology60, 34–42.
- Tomura H., Yamamoto-Mitani N., Nagata S., Murashima S. & Suzuki S. (2011) Creating an agreed discharge: discharge planning for clients with high care needs. Journal of Clinical Nursing20, 444–453.
- Tomura H., Nagata S., Murashima S. & Suzuki S. (2013) Development of a scale to evaluate professional discharge planning ability among nurses. Japan Academy of Nursing Science33(3), 3–13. (in Japanese).
- Ushiro R. (2009) Nurse-Physician Collaboration Scale: development and psychometric testing. Journal of Advanced Nursing65, 1497–1508.
- Watts R., Pierson J. & Gardner H. (2007) Co-ordination of the discharge planning process in critical care. Journal of Clinical Nursing16, 194–202.
- Yen M. & Lo L.H. (2002) Examining test-retest reliability: an intra-class correlation approach. Nursing Researchs 51, 59–62.
Document information
Published on 09/06/17
Submitted on 09/06/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?