Abstract
Objective
Closed reduction with percutaneous pinning is the treatment of choice for displaced supracondylar humerus fractures in children. In addition to configuration of pin fixation, many factors have been attributed to loss of reduction (LOR). The aim of the present study was to review potential factors that contribute to loss of reduction in the closed management of type III pediatric supracondylar fractures.
Methods
Treatment of 87 patients with type III supracondylar fractures was reviewed to determine factors associated with loss of reduction; 48 patients were treated with lateral pinning and 39 with crossed-pinning after closed reduction. Outcome parameters included radiographic maintenance of postoperative reduction.
Results
Lateral or crossed-pin configuration, pin spread at fracture site, pin-spread ratio (PSR), and direction of coronal displacement of the fracture were not associated with LOR. A significant difference (p = 0.01) was found between LOR rates of patients with medial wall communication and LOR.
Conclusion
Medial wall communication is a contributing factor to LOR in the management of type III supracondylar fractures. Cross-pinning should be preferred when medial wall communication is present, to provide more stable fixation.
Level of evidence
Level IV, Therapeutic study.
Keywords
Fracture ; Loss of reduction ; Supracondylar humerus ; Pin configuration
Introduction
Supracondylar fractures of the humerus are the most common type of elbow fracture in children, accounting more than 80% of all fractures.1 ; 2 Type III fractures according to Gartland classification are completely displaced.3 Surgical treatment of these fractures is complicated and requires orthopedic surgeons to perform technically difficult procedures. The standard treatment for type III extension supracondylar fractures is closed reduction and percutaneous pin fixation.4 ; 5 ; 6 However, there is ongoing debate about the use of crossed or parallel pin configuration for fixation of the fracture after closed reduction.7 ; 8 ; 9 ; 10
Though biomechanical studies have shown that crossed-pin is the most stable configuration, providing additional torsional rigidity, some clinical trials have shown good results with the lateral pin fixation method.11 ; 12 ; 13 ; 14 The advantage of lateral entry pin fixation is prevention of potential iatrogenic ulnar nerve injury, which may occur due to medial placement of the pin in as many as 12% of cases.15 ; 16
Stability of pin configuration in the management of type II and III extension fractures has been compared in clinical studies, the majority of which have reported comparable results. Many researchers primarily focused on pin configuration alone, without considering associated factors that may influence loss of reduction (LOR).7 ; 8 The aim of the present study was to compare LOR between medial and lateral pinning (crossed pinning) with lateral-entry pinning techniques for the treatment of Gartland type III extension fractures in children. An additional aim was to determine the potential factors affecting LOR after closed reduction and fixation of type III extension fractures.
Patients and methods
A total of 124 children were treated for displaced Gartland type III extension fracture at the present institution (a major tertiary care childrens hospital) between May 2013 and November 2014. Of these patients, 4 were excluded because they had undergone open reduction, 3 because preoperative skeletal traction was used, 3 because convergent pins were used, 6 because the fracture was found to be type II on evaluation, 5 because of the reduction quality was not postoperatively acceptable according to protocol, 8 due to inadequate quality of radiographs, and 8 due to the inadequate follow-up. Thus, 87 patients were enrolled, 48 of whom were in the lateral-entry group and 39 of whom were in the crossed-pin group. Local ethics committee approval was received.
Inclusion criteria included extension type III pediatric supracondylar fractures treated with closed reduction and percutaneous pinning in an emergent fashion (within 6 h of injury). Medical records were assessed regarding pinning technique, postoperative reduction quality, and LOR during follow-up. Postoperative complications including infection, nerve injury, and compartment syndrome were also recorded. Demographic preoperative data is shown in Table 1 .
| Crossed-pin technique | Lateral–entry pin technique | |
|---|---|---|
| Number of patients | 39 | 48 |
| Patient age (mean ± SD) (years) | 6.1 ± 2.8 | 6.2 ± 2.9 |
| Gender (male/female) | 27/12 | 35/13 |
| Displacement | ||
| Posteromedial | 11 | 16 |
| Posterolateral | 28 | 32 |
| Pulseless extremity | 2 | 0 |
| Neurologic deficit | ||
| AIN | 2 | 3 |
| Ulnar | 1 | 0 |
| PIN | 1 | 0 |
| Associated fractures | ||
| Distal radius | 2 | 1 |
| Ulna shaft | 1 | 0 |
SD: standard deviation; AIN: anterior interosseous nerve; PIN: posterior interosseous nerve.
All patients were subjected to operative treatment in the form of closed reduction and percutaneous pinning with either lateral or cross pinning technique. Fractures were treated by 1 of 6 full-time orthopedic surgeons. Choice of treatment primarily depended on surgeon preference and experience. Patients were divided into 2 groups. The lateral-entry pin group received 2 pins placed from the lateral side in a percutaneous, bi-cortical fashion. In this group only patients who had undergone either parallel or divergent lateral pinning techniques were enrolled. The medial or lateral addition of a third pin during surgery was also recorded.
Postoperative reduction quality was assessed after obtaining a comparison view taken early in the postoperative period to calculate Baumanns angle on the uninjured extremity.17 Baumanns angle difference of more than 12° between elbows on anterior-posterior (AP) radiographs was accepted as malposition. In addition, sagittal plane malreduction has been confirmed as a failure of the anterior humeral line to intersect the ossification center of the capitellum. AP radiographs were used to determine the communication of the medial or lateral columns.
Radiographic evaluation
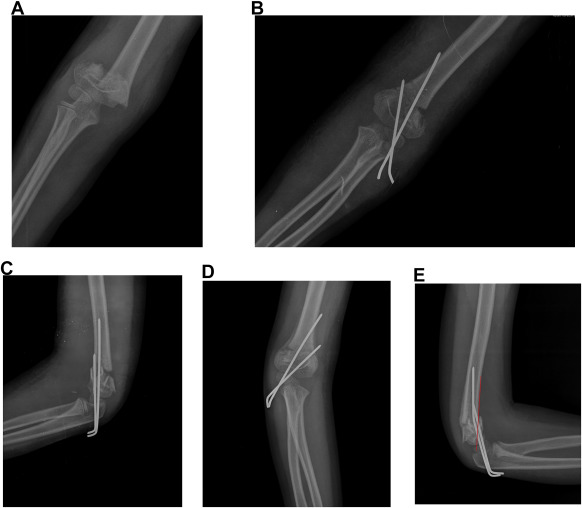
Direction of fracture displacement and fracture classification were assessed based on preoperative AP and lateral radiographs. Postoperative radiographic evaluation included true anterior-posterior radiograph and lateral radiograph of the elbow. Postoperative digital standard radiographs obtained after pin fixation at 3–4-week and 3-month follow-ups were postoperatively reviewed to determine LOR (Fig. 1 ).
|
|
|
Fig. 1. (A) Preoperative AP radiograph of type III supracondylar fracture. (B, C) Immediate postoperative AP and lateral radiographs revealing good reduction. Note medial wall comminution. (D, E) Radiographs taken at 4-week follow-up before pin removal showing reduction loss in coronal and sagittal planes. Red line indicates loss of reduction regarding the anterior humeral line. |
Baumanns angle was calculated on AP radiograph at 3-month follow-up, and change in Baumanns angle between the immediate postoperative radiograph and at 3-month follow-up was calculated. In addition, Baumanns angle of the contralateral side was assessed from the AP view of the normal elbow for comparison of postoperative reduction quality.17 LOR in coronal plane was assessed as described by Kocher et al.7 A change in Baumanns angle of <6° was defined as mild displacement, a change of 6°–12° was defined as major displacement in the coronal plane.
Reduction in the sagittal plane was assessed according to Skaggs et al as a failure of the anterior humeral line to intersect the ossification center of capitellum.12 This criteria was first assessed postoperatively to confirm anatomic fracture reduction, and was also reassessed at 3 months by control radiography in order to observe LOR in the sagittal plane.12 ; 13 All measurements were made by 3 pediatric orthopedists.
Pin-spread distance (PSD) and pin-spread ratio (PSR) at the fracture were measured using postoperative AP radiography. PSD is the measurement of the distance in the coronal plane between the pins at the fracture site (Fig. 2 ). When more than 2 pins were present, this distance was measured between the most distant pins. PSR was obtained by dividing PSD by the coronal length of the humerus at the fracture.18
|
|
|
Fig. 2. Pin-spread measurement at the level of the fracture. AB represents the coronal width of the humerus at the fracture site, while CD represents pin-spread distance. |
Long arm casts were postoperatively used, with the elbow at 70°–90° flexion. Patients were discharged within 2 days of the surgery, with pin care recommendations. All patients were both radiographically and clinically followed-up at 1 week, 3–4 weeks, and 3 months. Cast and pins were removed at the 3–4-week follow-ups as an outpatient procedure. Thereafter, full range of motion was initiated.
Patients were evaluated for humeral-ulnar angle as the carrying angle, and clinically evaluated for flexion and extension degrees according to Flynns criteria at 3-month follow-up.19
Statistical evaluation
All statistical analyses were conducted using SPSS software (version 21.0; SPSS Inc., Chicago, IL, USA). Data of all variables was analyzed to determine differences in characteristics between the LOR group and the group without loss of reduction. Multinomial logistic regression analysis was used to identify factors predictive of LOR. The level of significance was set at p < 0.05. Descriptives (mean ± SD) and 95% confidence intervals were calculated for continuous variables.
Results
Overall, 12 patients had LOR during follow-up, all of whom were in the lateral-entry group. Two patients with lateral entry pin configuration had major LOR in the coronal plane, and 3 of the 39 patients treated with medial and lateral entry method had LOR. No significant difference regarding LOR among the pinning groups was found (p = 0.14). Nine patients had a third pin either medially or laterally placed. Of these 9 patients, 6 had an additional medial pin placed (configuration: 1 medial and 2 lateral), and the other 3 had an additional lateral pin placed (configuration: 3 lateral entry pins). The patients with only (2 or 3) lateral pins were included into the lateral-entry group, while those who received an additional medial pin were included in the crossed-pin group.
Comparison of PSD at the fracture site among patients with and without LOR showed no significant difference (p = 0.34). Neither was significant difference found regarding the ratio of width of pin-spread to width of humerus at the fracture site (PSR) (p = 0.73). No significant difference was found upon comparison of PSR and PSD among groups with different pin configuration. Fractures that lost reduction had an average pin-spread of 12.4 mm (4.8–23.4) and 39% of humerus width, compared to 14.2 mm (6.8–31.7) and 41% of humerus width of those without LOR. Among the 9 patients with an additional third pin, 1 patient with an additional lateral pin placement (3 lateral configuration) had sagittal LOR.
Cosmetic and functional outcomes were similar between the groups at 3-month follow-up, according to the Flynn criteria. On the other hand, significant difference between patients with and without LOR regarding the association of medial wall comminution was found (p = 0.01). There was also significant difference in the lateral-entry group with regard to LOR and association of medial wall community (p = 0.01). However, in the crossed-pin group, no significant association of LOR with medial comminution was found (p = 0.48). Detailed statistical data is shown in Table 2 .
| Loss of reduction n:12 | Without loss of reduction n:75 | p value | Odds Ratio | %95 CI | |
|---|---|---|---|---|---|
| Number of patients (Cross-pinned/Lateral-entry) | 3/9 | 36/39 | 0.14 | 0.361 | 0.090–1.439 |
| Age (mean ± SD) (min–max) (years) | 5.3 ± 2.6 (1–10) | 6.3 ± 2.9 (1–13) | 0.28 | 0.884 | 0.705–1.109 |
| Gender (male/female) | 8/4 | 51/24 | 0.92 | 0.9412 | 0.257–3.434 |
| Displacement (Posteromedial/Posterolateral) | 3/9 | 24/51 | 0.62 | 0.708 | 0.175–2.854 |
| Medial comminution (present/absent) | 6/6 | 12/63 | 0.01 | 5.25 | 1.446–19.054 |
| Lateral entry (medial comminution, present/absent) | 5/4 | 6/33 | 0.01 | 6.875 | 1.421–33.261 |
| Cross-pinned (medial communituon, present/absent) | 1/2 | 6/30 | 0.48 | 2.50 | 0.194–32.19 |
| Baumanns angle (mean ± SD) (min–max) | 73.9 ± 6.7 (62.4–84) | 74.3 ± 5.1 (59.5–86) | 0.79 | 0.985 | 0.880–1.104 |
| Change in Baumanns angle (mean ± SD) (min–max) | −0.39 ± 3.1 (−6.4–5.8) | 0.02 ± 4.4 (−8–25.5) | 0.76 | 0.975 | 0.825–1.152 |
| Pin-spread distance (mean ± SD) (min–max) (mm) | 12.4 ± 5.6 (4.8–23.4) | 14.2 ± 4.2 (6.8–31.7) | 0.34 | 0.946 | 0.843–1.062 |
| Pin-spread distance (>10 mm/<10 mm) | 7/5 | 55/20 | 0.29 | 0.509 | 0.144–1.788 |
| Pin-spread distance (>13 mm/<13 mm) | 5/7 | 38/37 | 0.56 | 0.695 | 0.202–2.388 |
| Pin-spread distance/fracture line length (mean ± SD) (min–max) | %39 ± 15 | %41 ± 15 | 0.73 | 0.49 | 0.08–28.795 |
| Pin-spread distance/fracture line length (>30%/<30%) | 9/3 | 59/16 | 0.77 | 0.8136 | 0.196–3.361 |
SD: standard deviation; n: number; min: minimum; max: maximum; mm: millimeters.
Bold indicates significant values.
Discussion
LOR of 13.7% was found in the present study a result well-correlated with the related literature. Incidence of LOR is reported between 10 and 20% in the management of type III extension fractures, most of which presented with minor loss of reduction in the coronal plane, and were seen in lateral entry groups.7 ; 8 Some authors claim that 2 lateral pins alone provide adequate stabilization in completely displaced type III supracondylar fractures and avoid injury to the ulnar nerve.7 ; 8 ; 14 Though no significant difference between the groups regarding LOR was presently determined, 2 major displacements occurred in the coronal plane in the lateral-entry group. The number of patients with LOR (9) in the lateral-entry group was more than the double that of patients in the crossed pining group. We believe this finding to be remarkable, considering the small numbers of patients with LOR in the present study. On the other hand, the number of patients reported with LOR in other relevant clinical studies has been even smaller. Studies with a large number of patients are needed in order to draw conclusions.
The main limitation of the present study was its retrospective design. However, as a major tertiary care childrens hospital, medical records, and radiological and clinical follow-up protocols in the management of supracondylar fractures are well-established, as more than 200 fractures are treated per year.
It is believed that a strength of the present study was the exclusion of patients without acceptable reduction. One can speculate that fractures with initial displacement are prone to LOR. According to Gaston et al, a fracture that is pinned in a malreduced position that does not lose further reduction must be differentiated from a fracture pinned in an anatomic position that subsequently loses reduction.8 Moreover, the homogeneity of the groups with regard to pinning techniques was well-established; no patient with additional medial pin was included in the lateral-entry group.
In a surgeon-randomized prospective study by Gaston et al, patients who received an additional pin were included in the lateral-entry group.8 As a result of which, some lateral pin configurations were changed to crossed-pin. On the other hand, Kocher et al designed a prospective randomized trial with a relatively small number of patients and compared the configurations in type III supracondylar fractures.9 The authors excluded some patients due to additional pin placement. The exclusion of these patients may have had an effect on their results, considering the small number of patients with LOR. We may speculate that fractures requiring an additional medial pin placement possibly posed as fractures with more rotational instability. In the present study, all patients in the crossed-pin group who received an additional medial pin were included, regardless of the initial procedure.
No significant difference in characteristics between patients with and without LOR was found. Neither were differences found regarding pin configuration or presence of LOR in clinical evaluation of groups. It was determined that fracture characteristics may contribute to LOR, as fractures with medial wall comminution were at a higher risk. This was the only important factor contributing to LOR presently found. Larson et al stated in a biomechanical study that medial comminution decreases fracture stability significantly, and that the most stable pin configuration against the torsional forces is 2 lateral and 1 medial. It was also presently found that association of medial column comminution had significant relation to LOR in the lateral-entry group, though not in the crossed-pin group, in accordance with the findings of Larson et al. It is presently believed that crossed-pin fixation should be preferred when medial cortex comminution is present and stability cannot be obtained with 2 lateral pins.11
Pennock et al recently reported that pin spread is an important factor in the prevention of LOR, with a target pin spacing of at least 13 mm, or 1/3 the width of the humerus at the level of the fracture.18 However, Aarons reported that PSR, the distance between the pins at fracture level divided by the fracture width, was not associated with LOR.20 It was presently determined that PSD and PSR were not associated with LOR. However, the average PSD presently obtained was over 12 mm in both the lateral entry and crossed pining groups. This is an acceptable spread distance, suggested by many authors in order to avoid LOR. In addition, average PSRs were over 35% in both groups. These parameters are in agreement with Pennock suggestion that pin spacing should be at least 13 mm or 1/3 the width of the humerus at the level of the fracture in order to prevent LOR. Nevertheless, we agree with Sankar and Pennock et al that PSD and PSR are important technical considerations that aid in the provision of more stable constructs in order to protect reduction.18 ; 21
It is presently believed that stability in type III supracondylar fractures can be achieved regardless of pin configuration (lateral or crossed), unless medial wall communication is present. When medial comminution is present, crossed pinning configuration should be preferred, in order to protect the reduction. Pins with spread of approximately 1/3 the width of the fracture in bi-cortical fashion is the most important point of reduction control, as has been suggested.20 ; 21
This study is a retrospective type 3 original article.
Conflict of interest
None declared.
References
- 1 N.Y. Otsuka, J.R. Kasser; Supracondylar fractures of the humerus in children; J Am Acad Orthop Surg, 5 (1997), pp. 19–26
- 2 M.W. Shrader; Pediatric supracondylar fractures and pediatric phaseal elbow fractures; Orthop Clin North Am, 39 (2008), pp. 163–171
- 3 J.J. Gartland; Management of supracondylar fractures of the humerus in children; Surg Gynecol Obstet, 109 (1959), pp. 145–154
- 4 J.M. Abzug, M.J. Herman; Management of supracondylar humerus fractures in children: current concepts; J Am Acad Orthop Surg, 20 (2012), pp. 69–77
- 5 M. Aksakal, C. Ermutlu, B. Sarisozen, B. Akesen; Approach to supracondylar humerus fractures with neurovascular compromise in children; Acta Orthop Traumatol Turc, 39 (4) (2013), pp. 244–249
- 6 R. Omid, P.D. Choi, D.L. Skaggs; Supracondylar humeral fractures in children; J Bone Jt Surg Am, 90 (2008), pp. 1121–1132
- 7 M.S. Kocher, J.R. Kasser, P.M. Waters, et al.; Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial; J Bone Jt Surg Am, 89 (4) (2007), pp. 706–712
- 8 R.G. Gaston, T.B. Cates, D. Devito, et al.; Medial and lateral pin versus lateral—entry pin fixation for Type 3 supracondylar fractures in children: a prospective, surgeon randomized study; J Pediatr Orthop, 30 (8) (2010), pp. 799–806
- 9 J.G. Zhao, J. Wang, P. Zhank; Is lateral pin fixation for displaced supracondylar fractures of the humerus better than crossed pins in children?; Clin Orthop Relat Res, 471 (9) (2013), pp. 2942–2953
- 10 Y. Öztürkmen, M. Karamehmetoglu, I. Azboy; Closed reduction and percutaneous lateral pin fixation in the treatment of displaced supracondylar fractures of the humerus in children; Acta Orthop Traumatol Turc, 39 (5) (2005), pp. 396–403
- 11 L. Larson, K. Firoozbakhsh, R. Passarelli, P. Bosch; Biomechanical analysis of pinning techniques for pediatric supracondylar humerus fractures; J Pediatr Orthop, 26 (5) (2006) 573–8
- 12 D.L. Skaggs, J.M. Hale, J. Bassett, et al.; Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement; J Bone Jt Surg Am, 83-A (2001), pp. 735–740
- 13 L.E. Zionts, H.A. McKellop, R. Hathaway; Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children; J Bone Jt Surg Am, 76 (1994), pp. 253–256
- 14 D.L. Skaggs, M.W. Cluck, A. Mostofi, et al.; Lateral–entry pin fixation in the management of supracondylar fractures in children; J Bone Jt Surg Am, 86 (2004), pp. 702–707
- 15 J.P. Lyons, E. Ashley, M.M. Hoffer; Ulnar nerve palsies after percutaneous cross–pinning of supracondylar fractures in childrens elbows; J Pediatr Orthop, 18 (1998), pp. 43–45
- 16 A. Ozcelik, A. Tekcan, H. Ömeroglu; Correlation between iatrogenic ulnar nerve injury and angular insertion of the medial pin in supracondylar humerus fractures; J Pediatr Orthop B, 15 (2006), pp. 58–61
- 17 W.N. Keenan, J. Clegg; Variation of Baumanns angle with age, sex, side: implications for its use in radiological monitoring of supracondylar fracture of the humerus in children; J Pediatr Orthop, 16 (1996), pp. 97–98
- 18 A.T. Pennoc, M. Charles, M. Moor, T.P. Bastrom, P.O. Newton; Potential causes of loss of reduction in supracondylar humerus fractures; J Pediatr Orthop, 34 (7) (2014), pp. 691–697
- 19 J.C. Flynn, J.G. Matthews, R.L. Benoit; Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years' experience with long—term follow—up; J Bone Jt Surg Am, 56 (1974), pp. 263–272
- 20 C.E. Aarons, C. Lobts, D.B. Chan, D.C. Landy; Repair of supracondylar humerus fractures in children: does pin spread matter?; J Pediatr Orthop B, 21 (6) (2012), pp. 499–504
- 21 W.N. Sankar, N.M. Hebela, D.L. Skaggs, J.M. Flynn; Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention; J Bone Jt Surg Am, 89 (4) (2007), pp. 713–717
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?