Abstract
The effect of the antioxidant gallic acid (GA) on Pb toxicity in blood, liver and kidney was investigated in the present study. Rats Wistar received Pb nitrate (50 mg/Kg/day, i.p., 5 days) followed by GA (13.5 mg/Kg, p.o., 3 days) or a chelating agent (EDTA, 55 mg/Kg, i.p.). As result, Pb decreased body weight, hematocrit and blood δ-aminolevulinic acid dehydratase (ALA-D) activity. In addition, high Pb levels were observed in blood and tissues, together with increased (1) lipid peroxidation in erythrocytes, plasma and tissues, (2) protein oxidation in tissues and (3) plasma aspartate transaminase (AST) levels. These changes were accompanied by decreasing in antioxidant defenses, like superoxide dismutase (SOD) activity in tissues and catalase (CAT) activity and reduced glutathione (GSH) in liver. GA was able to reverse Pb-induced decrease in body weight and ALA-D activity, as well as Pb-induced oxidative damages and most antioxidant alterations, however it did not decrease Pb bioaccumulation herein as EDTA did. Furthermore, EDTA did not show antioxidant protection in Pb-treated animals as GA did. In conclusion, GA decreased Pb-induced oxidative damages not by decreasing Pb bioaccumulation, but by improving antioxidant defenses, thus GA may be promising in the treatment of Pb intoxications.
Keywords
Antioxidant ; Chelating agent ; Gallic acid ; Lead ; Oxidative stress
1. Introduction
Lead (Pb) is a non essential toxic heavy metal and one of the most widely used metal in industries. Pb may be found in printing, rubber, batteries, ceramics, dye, porcelain manufacturing, in accumulator industry and as a gasoline additive. Especially, the workers of these industrial branches are exposed to Pb [10] and [43] . In addition, the general population may getting exposed to Pb by contaminated food and water and by air pollution caused by industrial emission [40] and [45] . Unfortunately, even small quantities of Pb in the organism may are harmful [5] and [42] .
The main body structures affect by Pb exposure includes erythrocytes, liver and kidney [46] . The erythrocytes have a high affinity for Pb and contain about 99% of the Pb present in the blood, which they can spread to different organs of the body [61] . Liver, organ responsible for maintaining the body’s metabolic homeostasis, has been considered as the target organ for the toxic effects of Pb [48] and the largest Pb repository of softy tissues followed by kidney [28] and [49] . It has been known that Pb accumulation in these structures can interfere with several bioelements, whole role is critical for physiological processes.
Actually, Pb toxicity is related with oxidative stress (OS), due the capacity of Pb in disturbance the oxidant and antioxidant balance that is found in cells [39] . Lipids, proteins and carbohydrates can be oxidized by reactive oxygen species (ROS) in OS situations [24] and [60] . To minimize the potential damages caused by OS, the body has a combination of antioxidants [41] , which can be enzymatic [e.g. superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase, and glutathione reductase] or non-enzymatic [e.g., non-protein thiol groups, reduzed glutathione (GSH) and vitamin C (VIT C) e E] [22] . Several studies had showed increase in oxidative damages parameters, like lipid peroxidation and protein oxidation, as well as decrease in antioxidant defenses, like CAT, SOD, GSH and ascorbic acid, in blood/tissues of Pb-exposed animals [9] , [13] , [15] , [31] , [32] , [34] , [46] , [53] and [64] . In these studies, antioxidants have been designed to mitigate Pb-induced toxicity.
The current therapeutic approved to Pb intoxications is realized with chelation agents [2] , like calcium disodium ethylenediamine tetraacetic acid (EDTA), 2,3-dimercaptopropanol (British Anti Lewisite, BAL) or meso 2,3-dimercaptosuccinic acid (DMSA), which increase the body excretion of Pb preventing the damages induced by this metal. However these compounds have a toxic potential in themselves [19] and cannot be used at therapeutically adequate dose for a prolonged period of time [16] .
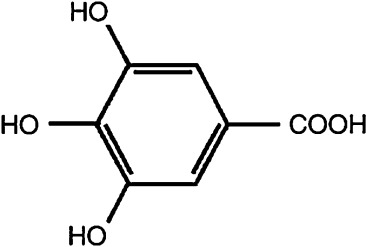
Gallic acid (3,4,5-trihydroxybenzoic acid, GA) (Fig. 1 ) is a natural phenolic antioxidant extractable from plants, especially green tea [33] , and is widely used in foods, drugs, and cosmetics. It received much attention because of its antioxidant actions and potent property of scavenge ROS, like superoxide anions, hydrogen peroxide, hydroxyl radicals and hypochlorous acid [52] , [26] and [51] , attenuating OS. In our previous study, gallic acid showed protective action against locomotor damage and brain OS induced by Pb in rats [53] , and against reserpine toxicity [54] . In this sense, the present study investigated the effect of GA in biochemical parameters of toxicity in blood, liver and kidney of Pb-treated rats.
|
|
|
Fig. 1. Chemical structure of gallic acid (3,4,5-trihydroxybenzoic acid). |
2. Materials and methods
2.1. Drugs
Drugs were purchased from Merck (Darmstadt, Germany). Pb and EDTA were dissolved in saline and protected from light until the use time. GA was dissolved in ultra-pure water and used until 10 min after preparation, thus ensuring its properties. All other chemicals and solvents used were of analytical or pharmaceutical and used as received.
2.2. Animals
The experiment was conducted with 32 male Wistar rats weighing 240 ± 10 g (about 2-month-old) at the start of the experiment. Groups of three or four animals were kept in plexiglas cages with free access to food and water in a room with controlled temperature (22–23 °C) and in 12 h light/dark cycles with lights on at 7:00 am The number of animals used was the minimum to obtain relevant results. The experimental protocol was approved by the ethical commission for animal use of Federal University of Santa Maria (process number 109/2010), which is in accordance with the international norms of animal care and maintenance. Animals were used after 7 days of acclimation.
2.3. Experimental design
The animals were treated with saline (1 mL/Kg, i.p., n = 14) or Pb (50 mg/Kg i.p., n = 21) once a day (9 a.m.) for 5 consecutive days [46] . From day 6, the saline-treated animals received water (1 mL/Kg, twice a day) or GA (6,75 mg/Kg/mL, twice a day) by gavage for 3 consecutive days. In addition, the Pb-treated animals received water (1 mL/Kg, twice a day, p.o.), GA (6,75 mg/Kg/mL, twice a day, p.o.) or EDTA (55 mg/Kg/mL, twice a day, i.p.) for 3 consecutive days at 9 a.m. and 5 p.m. Thus, the experimental groups of the present study were: control (C group, n = 7), GA group (n = 7), Pb group (n = 6), Pb-GA group (n = 6), Pb-EDTA group (n = 6). GA and EDTA treatments were in according with methodology described by Reckziegel et al. [53] .
Body weight variation of animals was monitored during the whole course of the experiment and they were expressed in% based on the weight recorded on the first day. The animals were sacrificed 15 h after the last dose under anesthesia with thiopental (50 mg/Kg body weight, i.p.) and euthanized by exsanguinations. Blood was collected by cardiac puncture and used to hematocrit and ALA-D activity and the remaining were centrifuged at 3000 rpm for 15 min to obtained plasma and erythrocytes, whose were also used for biochemical assays. The liver and kidney were removed and one part was stored at −20 °C for Pb quantification and the remaining were homogenized in 10 vols (w/v) of 0.1 M Tris-HCl buffer, pH 7.4, centrifuged at 3000 rpm for 10 min and the supernatants used for biochemical assays.
2.4. Biochemical assays
Lipid peroxidation was measured by TBARS levels in tissues [44] and in plasma and erythrocytes [25] and [29] . Results of TBARS were expressed as nmol MDA/g tissue, nmol MDA/mL plasma or nmol MDA/mL erythrocytes. Protein oxidation was determined by protein carbonyl levels [65] . Total carbonylation was calculated using a molar extinction coefficient of 22,000 M−1 cm−1 , according Levine et al. [30] and the results were expressed as nmol protein carbonyl/g tissue. The blood ALA-D activity was assayed according to Berlin and Schaller [6] and the results were expressed as nmol PBG (porphobilinogen)/h/mL blood. Plasma transaminases [alanine transaminase (ALT) and aspartate transaminase (AST)] were measured according to Reitman and Frankel [55] and Bessey et al. [8] and expressed as UI/L.
Antioxidant enzymatic defenses evaluated in the present study were SOD [38] and CAT [1] . SOD results were expressed as Units (U)/g tissue (1U = amount of enzyme required to produce 50% inhibition at 40 °C) and CAT activity as μmol H2 O2 /min/mL erythrocytes or μmol H2 O2 /min/g tissue. In addition, non enzymatic antioxidants measured were GSH levels in tissues and erythrocytes [11] and [25] and VIT C levels in plasma [18] and [25] . The results of GSH levels were expressed as μmol GSH/g tissue or nmol GSH/mL erythrocytes and of VIT C as μg VIT C/mL plasma.
For Pb quantification, wet tissue weight and blood volume were recorded. According to Mesko et al. [36] , after sample digestion with concentrated nitric acid using a microwave-assisted digestion system (Model Multiwave 3000, Anton Paar, Austria), digests were diluted to a constant volume with ultra pure water (Millipore, Billerica, USA). Determination Pb content was performed following the procedure of Peixoto et al. [50] with some modifications, using inductively coupled plasma optical emission spectrometer (ICP OES, Spectro Analytical Instruments, Model Spectro Ciros CCD, Germany) for tissues and inductively coupled plasma mass spectrometer (ICP-MS, PerkinElmer-SCIEX, Model Elan DRC II, Thornhill, Canada) equipped with a concentric nebulizer (Meinhard Associates, Golden, USA), a baffled cyclonic spray chamber (Glass Expansion, Inc., West Merbourne, Australia) and a quartz torch with a quartz injector tube (2 mm i.d.) for blood. The calibration standards were prepared from a multielemental standard solution by sequential dilution in 5% nitric acid in the range of 0.025–10 μg/L. The Pb detection limit was 0.2 ppm.
2.5. Statistical analysis
Data were analyzed by one-way ANOVA, followed by Duncan’s multiple range test when appropriate. Probability less than 0.05 were considered as statistically significant. Values were expressed as mean ± S.E.M.
3. Results
The effects of Pb exposure and GA and EDTA treatments on the variation (gain/loss) of body weight are show inTable 1 . Pb exposure decreased the body weight when compared to control group in sixth (end Pb exposure) and ninth (end treatment) days of protocol [F(4,30) = 52.87 and F(4,30) = 30.00, respectively; P < 0.001]. The GA, but no EDTA, was able to reverse partially this alteration in the ninth day.
| GROUP | Body weight variation (%) Pb-exposure End | Body weight variation (%) Treatments End |
|---|---|---|
| C | +4.1±1.1 | +7.9±1.8 |
| GA | +3.8±1.6 | +6.0±1.9 |
| Pb | −17.5±1.2** | −19.4±2.9** |
| PbGA | −14.8±3.9**,° | −12.2±4.1**,#,°° |
| PbEDTA | −15.8±1.6** | −13.4±2.6** |
Body weights in sixth and ninth days were expressed in relation to the initial weight. Data are expressed as mean ± S.E.M.
- . difference from C group (P < 0.001).
- . difference from Pb group (P < 0.05).
°. difference from GA group (P < 0.05).
°°. difference from GA group (P < 0.001).
The results of Pb exposure and GA and EDTA treatments on hematocrit levels and ALA-D activity are show inTable 2 . It was observed a decrease in hematocrit levels (9.6%) in Pb exposed animals in relation to the controls; and this effect was not reversed by any treatment employed (GA or EDTA) [F(4,30) = 7.26; P < 0.001]. Pb exposure also decreased blood ALA-D activity in relation to control group (5 times). GA alone had no effects on this variable, but the co-treatments Pb plus GA and Pb plus EDTA partially reversed the effects of Pb on the ALA-D activity. Comparing these two treatments, EDTA reversed the ALA-D activity more effectively than GA did, whose values differed significantly [F(4,30) = 76.35; P < 0.001].
| GROUP | C | GA | Pb | PbGA | PbEDTA |
|---|---|---|---|---|---|
| Hematocrit | 41.5±0.8 | 41.2±0.6 | 37.5±1.6* | 36.0±0.3**,° | 37.6±0.6* |
| ALA-D | 543.3±24.9 | 568.3±26.9 | 107.8±6.6** | 303.8±7.0**,-,+,° | 301.7±26.3**,# |
ALA-D activity (nmol PBG/h/mL blood). Data are expressed as mean ± S.E.M.
- . difference from C group (P < 0.05).
- . difference from C group (P < 0.001).
- . difference from Pb group (P < 0.05).
-. difference from Pb group (P < 0.001).
+. difference from PbEDTA group (P < 0.05).
°. difference from GA group (P < 0.05).
The results of Pb exposure and GA and EDTA treatments in blood, liver and kidney oxidative stress parameters and liver damage parameters are show inTable 3 . Pb exposure increased TBARS levels in erythrocytes (48.6%) and plasma (42.7%) when compared to the control group [F(4,30) = 8.11 and F(3,30) = 12.53, respectively, P < 0.001]. These effects were completely reversed by the treatment with GA. The EDTA treatment partially reversed the TBARS erythrocytes levels in erythrocytes, but no changed plasma TBARS levels in relation to Pb group. In tissues, Pb exposure also increased TBARS levels (35.2% in liver and 47.1% in kidney) in relation to the control group; GA and EDTA treatments reverted its partially in liver and completely in kidney [F(3,30) = 11.13 and F(3,30) = 15.78, respectively; P < 0.001].
| GROUP | C | GA | Pb | PbGA | PbEDTA | |
|---|---|---|---|---|---|---|
| TBARS | Erythrocytes | 17.88±0.77 | 19.25±1.69 | 26.57±1.68** | 17.05±1.03-,+ | 22.23±1.20*,# |
| Plasma | 12.42±0.51 | 13.61±0.68 | 17.73±0.37** | 12.84±0.75-,++ | 17.45±1.10** | |
| Liver | 18.6±0.8 | 18.1±1.1 | 25.2±1.2* | 13.8±1.0*,- | 13.8±2.3*,- | |
| Kidney | 25.7±0.9 | 22.6±0.6 | 37.8±1.7** | 28.7±1.9- | 24.9±2.0- | |
| CARBONYL | Liver | 2042.6±235.7 | 2247.8±115.0 | 3153.1±191.4** | 1862.3±150.1-,+ | 2798.2±184.8* |
| Kidney | 2209.3±98.6 | 2020.7±178.3 | 3664.7±533.9** | 1770.9±95.8- | 1432.7±170.3*,- | |
| AST | Plasma | 21.4±0.4 | 21.5±0.4 | 27.2±0.6** | 25.5±0.2**,#,° | 24.3±0.7**,- |
| ALT | Plasma | 19.2±0.5 | 19.6±0.3 | 18.2±0.4 | 18.1±0.5 | 18.4±0.3 |
TBARS levels (nmol MDA/g tissue); protein carbonyl levels (nmol protein carbonyl/g tissue). Data are expressed as mean ± S.E.M.
- . difference from C group (P < 0.05).
- . difference from C group (P < 0.001).
- . difference from Pb group (P < 0.05).
-. difference from Pb group (P < 0.001).
+. difference from PbEDTA group (P < 0.05).
++. difference from PbEDTA group (P < 0.001).
°. difference from GA group (P < 0.05).
Pb exposure increased carbonyl levels in liver (54.4%) and kidney (65.8%) in relation to control group [F(3,30) = 8.50 and F(3,30) = 14.22, respectively; P < 0.001]. GA was able to reverse completely these alterations, but EDTA just partially in kidney and no in liver.
In addition, an increase of AST levels in Pb exposed animals in relation to control group was observed (27.1%) [F(3,30) = 24.36, P < 0.001]. This effect was partially reverted by GA and EDTA treatments. No alterations were found in ALT levels.
The results of Pb exposure and GA and EDTA treatments in antioxidant parameters are show inTable 4 . SOD activity was decreased in liver and kidney of Pb exposed animals in relation to the control group (18.5% and 40%, respectively) and these events were partially reverted in liver by GA and EDTA treatments and completely in kidney just by GA treatment.
| GROUP | C | GA | Pb | PbGA | PbEDTA | |
|---|---|---|---|---|---|---|
| SOD | Liver | 2.7±0.1 | 2.8±0.1 | 2.2±0.1* | 2.5±0.1 | 2.4±0.2 |
| Kidney | 1.4±0.1 | 1.5±0.1 | 1.0±0.1* | 1.4±0.1# | 1.3±0.1 | |
| CAT | Erythrocyte | 26.1±1.0 | 28.9±1.3 | 24.4±1.2 | 31.3±0.9*,- | 28.2±2.4 |
| Liver | 3017.4±178.3 | 2917.8±87.3 | 2284.0±202.8* | 2837.4±222.1# | 2470.3±137.5* | |
| Kidney | 1354.0±39.7 | 1349.4±15.5 | 1475.4±90.7 | 1518.5±22.7 | 1468.9±61.3 | |
| GSH | Erythrocyte | 2664.5±121.5 | 2687.1±124.5 | 2913.0±44.2 | 2547.9±67.8 | 2844.6±209.5 |
| Liver | 8.9±0.4 | 8.8±0.6 | 5.2±0.8** | 8.4±0.5- | 6.9±0.3*,# | |
| Kidney | 4.3±0.3 | 3.8±0.4 | 3.9±0.4 | 3.2±0.5 | 4.4±0.8 | |
| VIT. C | Plasma | 19.3±0.4 | 19.3±1.1 | 19.2±2.1 | 22.4±0.5 | 21.7±1.6 |
SOD activity (U/g of tissue); CAT activity (μmol H2 O2 /min/mL erythrocytes or μmol H2 O2 /min/g tissue); GSH levels (nmol GSH/mL erythrocytes or mmol GSH/g tissue); plasma VIT C levels (mg VIT C/mL plasma). Data are expressed as mean ± S.E.M.
- . difference from C group (P < 0.05).
- . difference from C group (P < 0.001).
- . difference from Pb group (P < 0.05).
-. difference from Pb group (P < 0.001).
It was observed changes in erythrocyte CAT activity just in Pb exposed animals treated with GA (PbGA group) in relation to control group (increase of 19.9%) [F(3,30) = 3.11, P < 0.05). In liver, CAT activity decreased in Pb-exposed animals in relation to control group (24.3%), and this effect was completely reversed by GA treatment [F(3,30) = 3.40, P < 0.05]. No changes were observed in kidney CAT activity.
GSH levels were decreased in liver of Pb exposed animals in relation to control group (41.5%) [F(3,30) = 7.65, P < 0.001]. GA treatment reversed completely this effect and EDTA treatment, partially. No changes were observed in erythrocytes and kidney GSH levels, as well as in plasma VIT C levels.
The effects of Pb exposure and GA and EDTA treatments in Pb levels are show inTable 5 . It was observed an increase in Pb levels in blood, liver and kidney [F(4,20) = 2.91, P < 0.05; F(4,20) = 3.55, P < 0.05 and F(4,20) = 68.53, P < 0.001; respectively] in Pb-exposed animals in relation to control group. This effect was reverted by EDTA treatment and not by GA treatment.
| GROUP | C | GA | Pb | PbGA | PbEDTA |
|---|---|---|---|---|---|
| Blood Pb | 0.03±0.00 | 0.02±0.00 | 2.98±1.54* | 2.69±0.77* | 0.82±0.28 |
| Liver Pb | ND | ND | 129.66±48.85* | 149.22±57.72*,° | 89.42±36.56 |
| Kidney Pb | ND | ND | 135.60±11.56** | 161.50±16.94**,++ | 37.14±3.17*,- |
Lead levels (ppm). ND (no detectable, levels below 0.2 ppm). Data are expressed as mean ± S.E.M.
- . difference from C group (P < 0.05).
- . difference from C group (P < 0.001).
-. difference from Pb group (P < 0.001).
++. difference from PbEDTA group (P < 0.001).
°. difference from GA group (P < 0.05).
Statistical analyses revealed a significant correlation between ALA-D activity and blood Pb levels and hematocrit levels (r = 0.57, P < 0.001 and r = 0.55, P < 0.001, respectively).
4. Discussion
This study showed that rats treated with Pb decrease the body weight in relation to control animals. This result is in agreement with several studies [7] , [12] , [23] , [37] , [57] and [64] , which suggested that less body weight was due to reduced food consumption via Pb effects on the satiety set-point. After the treatment time, only the animals that received GA showed reversion partial of this less body weight, due probably the improvement of behavior and biochemical parameters.
Anemia observed in this study in Pb-exposed animals by decrease in hematocrit can be result by Pb property of inhibit many stages in the heme synthesis, while, for example, the enzyme δ-aminolevulinic acid dehydratase (ALA-D). ALA-D catalyses the formation of porphobilinogen from δ-aminolevulinic acid (ALA) [20] and it is used as one of the most reliable indicators of Pb intoxication [35] and [47] . In the present study, this enzyme was reduced in Pb-treated animals, as well as showed negative correlation to Pb blood levels and positive correlation to hematocrit, proving the involving between Pb, ALA-D and hematocrit. However, the GA and EDTA treatments reverted partially the ALA-D inhibition but not restored hematocrit levels, probably because the Pb also shortening of erythrocyte life span due the direct toxic effect of Pb upon the cell membrane [27] and is required about 3 months for regeneration of circulating erythrocytes.
OS has been involved in Pb toxicity [17] and [39] . According, the Pb may cause OS by two separate, although related, pathways: (1) the generation of ROS, including hydroperoxides, singlet oxygen, and hydrogen peroxide, and (2) the depletion of antioxidant reserves [14] . These events were observed in the present study.
The increase in ROS generation can be induced by Pb at different levels: (i) the Pb-induced inhibition of ALA-D may lead to accumulation of its substrate ALA, which can oxidize, and (ii) Pb per se has the capacity to stimulate ferrous ion [3] , [4] and [21] . In the present study, the oxidative damages caused by ROS can be observed by the increase in lipid peroxidation (TBARS levels) in erythrocytes, plasma, liver and kidney and protein oxidation (carbonyl levels) in liver and kidney in Pb-exposed animals, confirming previous studies [9] , [56] , [58] , [59] and [64] . Moreover, Pande et al. [46] did the same our Pb treatment protocol and observed increase in lipid peroxidation in liver. Whereas, GA markedly reversed Pb-induced OS damages, and EDTA too, but EDTA was less effective than GA. Reckziegel et al. [53] observed similar results in brain of rats treated with Pb and GA. Furthermore, aminotransferases (AST and ALT) represent enzymes that are regarded as markers of liver injury. In this study it was observed a modest increase in plasma AST levels, besides it is not biologically significant for liver injury, which was partially reverted by GA and EDTA treatments.
The antioxidant potential of the body can be enzymatic and non-enzymatic. The antioxidant enzymes evaluated, SOD and CAT, form the first line of defense against ROS and the decrease in their activities contribute to the OS [5] . Pb reduced the activity of SOD in liver and kidney and of CAT in liver. Interestingly, GA could markedly renew the activities of these antioxidant enzymes of Pb-exposed rats and significantly enhanced the antioxidant capacity of the body. In erythrocytes, GA increased the CAT activity probably as a compensatory mechanism to eliminate hydroperoxides produce during Pb exposure.
GSH is a tripeptide containing cysteine that has a reactive thiol group with reductive potency and can act as a non-enzymatic antioxidant by direct interaction of thiol group with ROS. Pb binds exclusively to the thiol groups which decrease the GSH levels thereby interfering with the antioxidant activity [62] . In this study, GSH levels decreased in liver only and the treatment with GA reverted completely this decrease and with EDTA, partially. It was observed that liver was the tissue with antioxidant potential most affected by Pb, probably by its involvement in Pb detoxification. Surprisingly, other non-enzymatic antioxidant evaluated, the VIT C, a low molecular mass antioxidant that scavenges the aqueous free radicals, no change in plasma.
Certainly the higher concentration of Pb in blood and tissues, following experimental exposure, was associated with increased oxidative reaction, which might be responsible, at least in part, for Pb-induced toxic effects. In the present study, it was observed an increase in Pb concentrations in blood, liver and kidney in Pb-exposed animals in relation to the control ones. We observed that EDTA, a conventional chelating agent which is used in Pb poisonings, was able to reverse the high Pb concentrations in all structures evaluated, proving it chelating property. In according, Patra et al. [48] found a significant higher level of Pb in liver of rats exposed to Pb for 4 weeks and a significant reduction of Pb levels after treatment with EDTA during fifth week. However, besides its proved chelating property, we observed that EDTA cannot reverse effectively the antioxidants parameters changed by Pb (SOD and CAT activities and GSH levels). In this sense, we believed that EDTA oxidative protection, observed in TBARS and carbonyl levels, can be due the chelating action, which decrease Pb body concentrations. On the other hand, GA no decreased body Pb concentrations, but reverted oxidative parameters and antioxidants alterations. This results show that GA reversion in oxidative damages induced by Pb cannot be attributed by chelating property while EDTA, but to its antioxidant potential and capacity of improve the body antioxidant defenses.
Data from literature showed that GA antioxidant property proven here is due its capacity to scavenge ROS, like superoxide anions, hydrogen peroxide, hydroxyl radicals and hypochlorous acid [26] and [51] . Its molecular structure has tri-hydroxyl groups, thereby verifying a previous report that phenolic hydroxyl groups are important in showing a potent radical scavenging effect [63] . Lu et al. [33] showed that the hydroxyl group at the para position to the carboxylic group is especially effectual for GA antioxidant activity ( Fig. 1 ).
5. Conclusion
GA is able to reverse oxidative damages induced by Pb due it antioxidant potential and capacity of improve body antioxidant status and not by chelating property. In addition, the results showed here confirm the beneficial of antioxidants use in Pb intoxications. Further studies are needed to evaluate the use of GA together of a chelating agent in Pb-treated rats.
References
- [1] H. Aebi; Catalase in vitro; Meth. Enzymol., 105 (1984), pp. 121–126
- [2] M. Ahamed, M.K.J. Siddiqui; Low levels lead exposure and oxidative stress: current opinions; Clin. Chim. Acta, 383 (2007), pp. 57–64
- [3] M. Ahamed, M.K. Siddiqui; Environmental lead toxicity and nutritional factors; Clin. Nutr., 26 (2007), pp. 400–408
- [4] M. Ahamed, P.K. Mehrotra, P. Kumar, M.K.J. Siddiqui; Placental lead-induced oxidative stress and preterm delivery; Ecotoxicol. Environ. Saf., 27 (2009), pp. 70–74
- [5] M.T. Antonio-García, E.L. Massó-Gonzalez; Toxic effects of perinatal lead exposure on the brain of rats: involvement of oxidative stress and the beneficial role of antioxidants; Food Chem. Toxicol., 46 (2008), pp. 2089–2095
- [6] A. Berlin, K.H. Schaller; European standardized method for the determination of delta-aminolevulinic acid dehydratase activity in blood; Z. Klin. Chem. Klin. Biochem., 12 (1974), pp. 389–390
- [7] A.A. Berrahal, A. Nehdi, N. Hajjaji, N. Gharbi, S. El-Fazâa; Antioxidant enzymes activities and bilirubin level in adult rat treated with lead; C.R. Biol., 330 (2007), pp. 581–588
- [8] O.A. Bessey, O.H. Lowry, M.J.J. Brock; A method for the rapid determination of alkaline phosphatase with five cubic millimetres of serum; J. Biol. Chem., 164 (1946), pp. 321–329
- [9] E. Caylak, M. Aytekin, I. Halifeoglu; Antioxidant effects of methionine α-lipoic acid, N-acetylcysteine and homocysteine on lead-induced oxidative stress to erythrocytes in rats; Exp. Toxicol. Pathol., 60 (2008), pp. 289–294
- [10] Center for Disease Control Prevention (CDC); Adult blood lead epidemiol-ogy and surveillance—United States: 2008–2009; MMWR—Morb. Mortal Wkly. Rep., 60 (2011), pp. 841–845
- [11] G.L. Ellman; Tissue sulfhydryl groups; Arch. Biochem., 82 (1959), pp. 70–77
- [12] A.A. El-Nekeety, A.A. El-Kady, M.S. Soliman, N.S. Hassan, M.A. Abdel-Wahhab; Protective effect of Aquilegia vulgaris (L.) against lead acetate-induced oxidative stress in rats ; Food Chem. Toxicol, 47 (2009), pp. 2209–2215
- [13] G.H. El-Sokkary, G.H. Abdel-Rahman, E.S. Kamel; Melatonin protects against lead-induced hepatic and renal toxicity in male rats; Toxicology, 213 (2005), pp. 25–33
- [14] N. Ercal, H. Gurer-Orhan, N. Aykin-Burns; Toxic metals and oxidative stress part I: mechanism involved in metal induced oxidative damage; Curr. Top. Med. Chem., 1 (6) (2001), pp. 529–539
- [15] S.J.S. Flora, M. Pande, G.M. Kannan, A. Mehta; Lead induced oxidative stress and its recovery following co-administration of melatonin or N-acetylcysteine during chelation with succimer in male rats; Cell. Mol. Biol, 50 (2004), pp. OL543–OL551
- [16] S.J. Flora, G. Saxena, P. Gautam, P. Kaur, K.D. Gill; Response of lead-induced oxidative stress and alterations in biogenic amines in different rat brain regions to combined administration of DMSA and MiADMSA; Chem. Biol. Interact, 170 (2007), pp. 209–220
- [17] S.J.S. Flora, D. Mishra, A. Mehta, G. Saxena, V. Pachauri; Combinational chelation therapy abrogates lead-induced neurodegeneration in rats; Toxicol. Appl. Pharmacol., 240 (2009), pp. 255–264
- [18] H. Galley, M.J. Davies, N.R. Webster; Ascorbil radical formation in patients with sepsis: effects of ascorbate loading; Free Radic. Biol. Med., 20 (1996), pp. 139–143
- [19] Gilman, A.G., Rall, T.W., Nies, A.S., Taylor, P., 1991. Goodman & Gilman’s the Pharmacological Basis of Therapeutics, Pergamon, New York, pp. 1592–1614.
- [20] R.A. Goyer, B.C. Rhyne; Pathological effects of lead; Int. Rev. Exp. Pathol., 12 (1973), pp. 1–77
- [21] H. Gurer-Orhan, H.U. Sabir, H. Ozgunes; Correlation between clinical indi-cator of lead poisoning and oxidative stress parameters in controls and lead exposed workers; Toxicology, 195 (2004), pp. 147–154
- [22] B. Halliwell, J.M.C. Gutteridge; Free Radicals in Biology and Medicine; (3rd ed.)Oxford, UK (2000)
- [23] P.B. Hammond, D.J. Minnema, R. Shukla; Lead lowers the set point for food consumption and growth in wealing rats; Toxicol. Appl. Pharmacol., 106 (1990), pp. 80–87
- [24] A. Helen, K. Krishnakumar, P.L. Vijayammal, K.T. Augusti; Antioxidant effect of onion oil (Allium cepa . Linn) on the damages induced by nicotine in rats as compared to alpha-tocopherol ; Toxicol. Lett., 116 (1–2) (2000), pp. 61–68
- [25] M.C. Jacques-Silva, C.W. Nogueira, L.C. Broch, E.M.M. Flores, J.B.T. Rocha; Diphenyl diselenide and ascorbic acid changes deposition of selenium and ascorbic acid in liver and brain of mice; Pharmacol. Toxicol., 88 (2001), pp. 119–125
- [26] Y. Kim; Antimelanogenic and antioxidant properties of gallic acid; Biol. Pharm. Bull., 30 (6) (2007), pp. 1052–1055
- [27] C.D. Klassen; Heavy metals and heavy metal antagonists; Goodman and Gilman’s Pharmacological Basis of Therapeutics, McGraw-Hill Ed., USA (1996)
- [28] V. Kumar, K.A. Abul, F. Nelson, N.M. Richard; Robbins Basic Pathology; (8th ed.)Elsevier, New Delhi, India (2007)
- [29] D. Lapenna, G. Ciofani, S.D. Pierdomenico, M.A. Giamberardino, F. Cuccurullo; Reaction conditions affecting the relationship between thiobarbituric acid reactivity and lipid peroxides in human plasma; Free Radic. Biol. Med., 31 (2001), pp. 331–335
- [30] R.L. Levine, D. Garland, C.N. Oliver, A. Amici, I. Climent, A.G. Lenz, B.W. Ahn, S. Shaltiel, E.R. Stadtman; Determination of carbonyl content in oxidatively modified proteins; Methods Enzymol., 186 (1990), pp. 464–478
- [31] C. Liu, J. Ma, Y. Sun; Quercetin protects the rat kidney against oxidative stress-mediated DNA damage and apoptosis induced by lead; Environ. Toxicol. Pharmacol., 30 (3) (2010), pp. 264–271
- [32] C. Liu, Y. Zheng, J. Lu, Z. Zhang, S. Fan, D. Wu, J. Ma; Quercetin protects rat liver against lead-induced oxidative stress and apoptosis; Environ. Toxicol. Pharmacol., 29 (2010), pp. 158–166
- [33] Z. Lu, G. Nie, P.S. Belton, H. Tang, B. Zhao; Structure-activity relationship analysis of antioxidant ability and neuroprotective effect of gallic acid derivatives; Neurochem. Int., 48 (2006), pp. 263–274
- [34] E.E. Mehana, M.A. Meki, K.M. Fazili; Ameliorated effects of green tea extract on lead induced liver toxicity in rats; Exp. Toxicol. Pathol. (2010) http://dx.doi.org/10.1016/j.etp.2010.09.001
- [35] P.A. Meredith, H.L. Elliott, B.C. Campbell, M.R. Moore; Changes in serum aluminium, blood zinc, blood lead and erythrocyte δ-aminolaevulinic acid dehydratase activity during haemodialysis; Toxicol. Lett., 4 (1979), pp. 419–424
- [36] M.F. Mesko, D.P. de Moraes, J.S. Barin, V.L. Dressler, G. Knapp, E.M.M. Flores; Digestion of biological materials using the microwave-assisted sample combustion technique; Microchem. J., 82 (2006), pp. 183–188
- [37] D.J. Minnema, P.B. Hammond; Effect of lead exposure on patterns of food intake in weanling rats; Neurotoxicol. Teratol., 16 (1994), pp. 623–629
- [38] H.P. Misra, I. Fridovich; The role of superoxide anion in the autoxidation of epinephrine and simple assay for superoxide dismutase; J. Biol. Chem., 247 (1972), pp. 3170–3175
- [39] H.M. Mousa, A.A. Al-Qarawi, B.H. Ali, H.A.A. Rahman, S.A. ElMougy; Effect of lead exposure on the erythrocytic antioxidant levels in goats; J. Vet. Med. A, 49 (2002), pp. 531–534
- [40] A. Mudipalli; Lead hepatotoxicity & potential health effects; Indian J. Med. Res., 126 (6) (2007), pp. 518–527
- [41] S.R. Naik; Antioxidants and their role in biological functions: an overview; Indian Drugs, 40 (2003), pp. 501–516
- [42] R.Y. Niu, Z.L. Sun, Z.T. Cheng, Z.G. Li, J.D. Wang; Decreased learning ability and low hippocampus glutamate in offspring rats exposed to fluoride and lead; Environ. Toxicol. Pharmacol., 28 (2009), pp. 254–258
- [43] T.D. Oberley, A.L. Friedman, R. Moser, F.L. Siegel; Effects of lead administration on developing rat kidney: functional morphologic, and immunohistochemical studies; Toxicol. Appl. Pharmacol., 131 (1995), pp. 94–107
- [44] H. Ohkawa, N. Ohishi, K. Yagi; Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction; Anal. Biochem., 95 (1979), pp. 351–358
- [45] M. Pande, S.J.S. Flora; Lead induced oxidative damage and its response to combined administration of α-lipoic acid and succimers in rats; Toxicology, 177 (2002), pp. 187–196
- [46] M. Pande, A. Mehta, B.P. Pant, S.J.S. Flora; Combined administration of chelating agent and antioxidant in the prevention and treatment of acute lead intoxication in rats; Environ. Toxicol. Pharmacol., 9 (2001), pp. 173–184
- [47] J.B. Pappas, J.T. Ahlquist, E.M. Allen, W. Banner; Oral dimercaptosuccinic acid and ongoing exposure to lead: effects on heme synthesis and lead distribution in a rat model; Toxicol. Appl. Pharmacol., 133 (1995), pp. 121–129
- [48] R.C. Patra, D. Swarup, S. Dwivedi; Antioxidant effects of a-tocopherol, ascorbic acid and L-methionine on lead-induced oxidative stress to the liver, kidney and brain in rats; Toxicology, 162 (2001), pp. 81–88
- [49] L. Patrick; Lead toxicity part II: the role of free radical damage and the use of antioxidants in the pathology and treatment of lead toxicity; Altern. Med. Rev., 11 (2006), pp. 114–127
- [50] N.C. Peixoto, L.C. Rocha, D.P. Moraes, M.J. Bebianno, V.L. Dressler, E.M.M. Flores, M.E. Pereira; Changes in levels of essential elements in suckling rats exposed to zinc and mercury; Chemosphere, 72 (2008), pp. 1327–1332
- [51] K. Polewski, S. Kniat, D. Slawinska; Gallic acid a natural antioxidant, in aqueous and micellar environment: spectroscopic studies; Curr. Top. Biophys., 26 (2002), pp. 217–227
- [52] D.H. Priscilla, P.S.M. Prince; Cardioprotective effect of gallic acid on cardiac troponin-T cardiac marker enzymes, lipid peroxidation products and antioxidants in experimentally induced myocardial infarction in Wistar rats; Chem. Biol. Interact., 179 (2009), pp. 118–124
- [53] P. Reckziegel, V.T. Dias, D. Benvegnú, N. Boufleur, R.C.S. Barcelos, H.J. Segat, C.S. Pase, C.M.M. Santos, E.M.M. Flores, M.E. Bürger; Locomotor damage and brain oxidative stress induced by lead exposure are attenuated by gallic acid treatment; Toxicol. Lett., 203 (2011), pp. 74–81
- [54] P. Reckziegel, L.R. Peroza, L.F. Scheffer, M.C. Ferrari, M.E. Burguer, R. Fachinetto; Gallic acid decreases vacuous chewing movements induced by reserpine in rats; Pharmacol. Biochem. Behav., 104 (2013), pp. 132–137
- [55] S. Reitman, S. Frankel; A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminase; Am. J. Clin. Pathol., 28 (1957), pp. 8–15
- [56] A. Rendón-Ramirez, J. Cerbón-Solórzano, M. Maldonado-Veja, M.A. Quintanar-Escorza, J.V. Calderón-Salinas; Vitamin-E reduces the oxidative damage on δ-aminolevulinic dehydratase induced by lead intoxication in rat erythrocytes; Toxicol. In Vitro, 21 (2007), pp. 1121–1126
- [57] M. Sabbar, C. Delaville, P. de Deurwaerdère, A. Benazzouz, N. Lakhdar-Ghazal; Lead intoxication induces noradrenaline depletion, motor nonmotor disabilities, and changes in the firing pattern of subthalamic nucleus neurons; Neuroscience, 210 (2012), pp. 375–383
- [58] G. Saxena, U. Pathak, S.J.S. Flora; Beneficial role of monoesters of meso -2,3-dimercaptosuccinic acid in the mobilization of lead and recovery of tissue oxidative injury in rats ; Toxicology, 214 (2005), pp. 39–56
- [59] V. Sharma, A. Sharma, L. Kansal; The effect of oral administration of Allium sativum extracts on lead nitrate induced toxicity in male mice ; Food Chem. Toxicol., 48 (2010), pp. 928–936
- [60] H. Sies; Oxidative stress: oxidants and antioxidants; Exp. Physiol., 82 (1997), pp. 291–295
- [61] R. Sivaprasad, M. Nagaraj, P. Varalakshmi; Combined efficacies of lipoic acid and meso-2,3-dimercaptosuccinic acid on lead induced erythrocyte membrane lipid peroxidation and antioxidant status in rats; Hum. Exp. Toxicol, 22 (2003), pp. 183–192
- [62] R. Sivaprasad, M. Nagaraj, P. Varalakshmi; Combined efficacies of lipoic acid and 2,3-dimercapto succinic acid against lead-induced lipid peroxidation in rat liver; J. Nutr. Biochem., 15 (2004), pp. 18–23
- [63] S. Son, B.A. Lewis; J. Agric. Food Chem., 50 (2002), pp. 468–472
- [64] D. Xia, X. Yu, S. Liao, Q. Shao, H. Mou, W. Ma; Protective effect of Smilax glabra extract against lead-induced oxidative stress in rats ; J. Ethonopharmacol., 130 (2) (2010), pp. 414–420
- [65] L.J. Yan, M.G. Traber, L. Packer; Spectrophotometric method for determination of carbonyls in oxidatively modified apolipoprotein B of human low-density lipoproteins; Anal. Biochem., 228 (1995), pp. 349–351
Document information
Published on 12/05/17
Accepted on 12/05/17
Submitted on 12/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?