Summary
Perforation of the vermiform appendix in a septic neonate with an Amyands hernia resulted in the formation of a scrotal enterocutaneous fistula. In conclusion from this exceptional complication, active parental awareness for any neonatal scrotal swelling is required, and an early operative policy for the neonatal inguinal hernia is significant.
Keywords
acute appendicitis;enterocutaneous fistula;neonatal hernia;perforated Amyands hernia;scrotal
1. Introduction
A vermiform appendix, normal or inflamed, that is present in the sac of an inguinal hernia is called an Amyands hernia. Claudius Amyand, in 1735, performed an appendectomy on 11-year-old Hanvil Anderson at St Georges Hospital, London.1 The inflamed appendix was located in the sac of a right-sided inguinal hernia, with the clinical manifestation of a fecal fistula discharging in the groin. The fistula was the result of perforation of the lumen of the vermiform appendix by a pin. After a ½-hour long successful appendectomy, which was actually the first appendectomy performed in the history of medicine, the patient was cured, although the hernia recurred.1 Herein, we present a unique case of a neonatal Amyands hernia, presented as an enterocutaneous fistula of the scrotum, as a result of perforation of the inflamed appendix.
2. Case report
A 25-day-old male neonate was referred to our institution because of an enterocutaneous fistula with discharge of fecal matter from the right hemiscrotum (Fig. 1). He was born at 36 weeks of gestation through normal delivery, and on admission he weighed 3100 g. The parents did not pay any attention to the swelling and the reddish color of the right inguinoscrotal region during the previous 5 days. The patient was in a septic status, with a pulse rate of 170 beats/minute, a blood pressure of 110/55 mmHg, and was breathing at a rate of 60 breaths/minute. He had fever (39°C), mottled skin on the trunk and extremities, and mild abdominal distention. The scrotum and penis were edematous. Fecal material drained from an ulcer at the right side of the scrotum. The right inguinal area was tender. Blood examination revealed anemia (hematocrit 20.7% and hemoglobin 7.3 g/dL), leukocytosis (white blood cells 15.600/μL, neutrophils 46.10%, and lymphocytes 31.3%), 211,000 platelets/μL, C-reactive protein 30.19 mg/L, glucose 79 mg/dL, urea 9 mg/dL, creatinine 0.22 mg/dL, Na 138.3 mmol/L, K 4.22 mmol/L, and Cl 107.1 mmol/L. Plain radiography performed with the patient in an upright position showed distended enteric loops in the abdomen and the presence of gas in the scrotum (Fig. 2).
|
|
|
Figure 1. Clinical presentation of an Amyands hernia as an enterocutaneous fistula of the scrotum. |
|
|
|
Figure 2. Abdominal radiography showing distended small bowel enteric loops and the presence of air in the scrotum. |
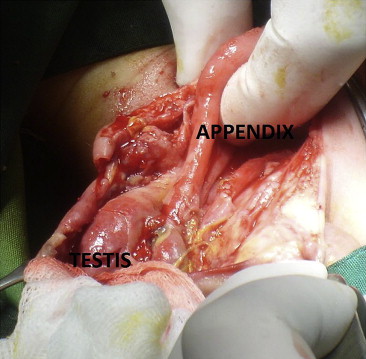
After resuscitation with intravenous crystalloid fluids, blood transfusion, and administration of broad spectrum antibiotics (ceftazidime, amikacin, and metronidazole), he was taken to the operating room with a preoperative diagnosis of strangulated inguinal hernia, complicated by bowel perforation and formation of an enterocutaneous fistula. The initial inguinal incision was extended to the fistula of the scrotum to facilitate dissection of the adhered and inflamed tissues. A perforated vermiform appendix was found in the scrotum, which was adhered to the testis (Fig. 3). An appendectomy was performed, the purulent material was removed, and the anatomy or the inguinal and scrotal areas were restored. Postoperative hospital stay lasted 10 days. During follow-up examination by scrotal Doppler ultrasound 3 months and 6 months after the operation, the right testis was viable. The hernia did not recur.
|
|
|
Figure 3. Perforated appendix in the inflamed scrotum. |
3. Discussion
Amyands hernia is an extremely rare condition. The rate of incidence of a normal appendix located in an inguinal hernia varies from 0.5% to 1%, whereas an inflamed appendix is found in 0.1% of herniotomies.2 ; 3 Amyands hernia, as a rule, occurs in the right inguinal region. If it is left sided, it may be due to mobile cecum, malrotation, or situs inversus.3; 4 ; 5
The presence of a noninflamed appendix in the inguinal hernia is three times more common in children than in adults.4 This is due to the persistent patency of the processus vaginalis in infancy and childhood.6 ; 7 A congenital band extending from the appendix into the scrotum and attached to the right testis,8 and the funnel-shaped tapering cecum of the neonate are two more possible pathogenetic factors.6
The pathophysiology of acute appendicitis in the inguinal canal is under controversy. It is not certain whether a relationship exists between incarceration and inflammation, or whether it is incidental.9 The mechanical entrapment, manipulation, and compression of the appendix, because of either the narrow inguinal ring or the attempt to reduce herniated content, are possible mechanisms that explain blood supply compromise, the resulting bacterial overgrowth, and inflammation.9; 10 ; 11 Park et al,4 who reported a case of incarcerated Amyands hernia in a neonate after circumcision, proposed the mechanism of epididymo-orchitis as a result of the circumcision, with secondary inflammation of the trapped appendix in the sac of the hernia.
Clinical presentation of an Amyands hernia may be that of a normal, obstructed, or strangulated inguinal hernia, irrespective of whether the appendix is inflamed or not.12 Acute scrotum and abdominal pain are possible clinical presentations.12 ; 13 Testicular torsion, especially when there is an undescended testis; inguinal lymphadenitis; epididymo-orchitis; and hydrocele of the spermatic cord are conditions that an Amyands hernia may mimic.6; 12 ; 14 The diagnosis of an Amyands hernia is made during surgical exploration of the groin as a rule, although in some cases ultrasound, computed tomography, and testicular scan have been proved helpful.2; 4 ; 12
Even though appendectomy can be performed through an inguinal incision or with laparoscopy, many authors prefer to save the appendix when it is not inflamed, because of the importance of the lymphoid tissue, complications of an appendectomy, and risk of wound infection and for possible later use in urinary diversion, biliary tract reconstruction, and antegrade bowel enemas.13 ; 14
Neonatal appendicitis is extremely rare (0.1% of appendicitis cases in infancy, which constitutes 2% of pediatric appendicitis).10 Premature neonates account of 50% of these cases, and only in one-third of these, the inflamed appendix lies within a hernia.10 ; 12 This low frequency rate and the fact that only 20 neonatal cases of Amyands hernia have been reported in English publications render the cases of perforated appendix in premature neonates extremely rare.3; 10; 12 ; 13 Kumar et al12 reported neonatal pyoscrotum and perforated appendicitis in a 26-day-old male with undescended testis, who was initially diagnosed to have testicular torsion. Iuchtman et al7 reported a case of scrotal abscess following perforated appendicitis in a 6-day-old male.
Enterocutaneous fistula secondary to appendicitis in an Amyands hernia is extremely rare. A case of fistula formation in an Amyands hernia has been reported recently, in a 1-year-old patient with a chronic enteroscrotal sinus.15 We did not find any other similar case reported in the English medical literature. Acute appendicitis complicated by the formation of a fistula in a neonate renders the case presented here unique.
In conclusion, prompt diagnosis of an enterocutaneous fistula in the groin or scrotum of a neonate depends on two important parameters. The first is the awareness of the family. In our case, the parents did not pay enough attention to the initial phase of the scrotal swelling and did not seek medical advice promptly. The second parameter involves the surgeon who should adopt an early repair policy for neonatal hernia. If there is a lack of parental awareness or a delay in the repair process, prognosis may be grave. Timely operative intervention reduces both morbidity and mortality.
References
- 1 C. Amyand; Of an inguinal rupture, within a pin in the appendix caeci, incrusted with stone, and some observations on wounds in the guts; Philos Transact R Soc Lon, 39 (1736), pp. 329–336
- 2 A. Kaymakci, I. Akillioglou, I. Akkoyun, S. Guben, A. Ozdemir, S. Gulen; Amyands hernia: a series of 30 cases in children; Hernia, 13 (2009), pp. 609–612
- 3 K. Singh, R.R. Singh, S. Kaur; Amyands hernia; J Indian Assoc Pediatr Surg, 16 (2011), pp. 171–172
- 4 J. Park, M. Hemani, S.S. Milla, R. Rivera, E. Nadler, J.P. Alukal; Incarcerated Amyands hernia in a premature infant associated with circumcision: a case report and literature review; Hernia, 14 (2010), pp. 639–642
- 5 H.G. Johari, S. Paydar, S.Z. Davani, S. Eskandari, M.G. Johari; Left-sided Amyand hernia; Ann Saudi Med, 29 (2009), pp. 321–322
- 6 J.A. Milburn, G.G. Youngson; Amyands hernia presenting as neonatal testicular ischaemia; Pediatr Surg Int, 22 (2006), pp. 390–392
- 7 M. Iuchtman, M. Kirshon, M. Feldman; Neonatal pyoscrotum and perforated appendicitis; J Perinatol, 19 (1999), pp. 536–537
- 8 P. Oguzkurt, F. Kayaselcuk, S. Oz, I.S. Arda, L. Oguzkurt; Sliding appendiceal inguinal hernia with a congenital fibrovascular band connecting the appendix vermiformis to the right testis; Hernia, 5 (2001), pp. 156–157
- 9 L. Cankorkmaz, H. Ozer, C. Guney, M.H. Atalar, M.S. Arslan, G. Koyluoglu; Amyands hernia in the children: a single center experience; Surgery, 147 (2010), pp. 140–143
- 10 E. Livaditi, G. Mavridis, G. Christopoulos-Geroulanos; Amyands hernia in premature neonates: report of two cases; Hernia, 11 (2007), pp. 547–549
- 11 S. Gupta, R. Sharma, R. Kaushik; Left-sided Amyands hernia; Singapore Med J, 46 (2005), pp. 424–425
- 12 R. Kumar, J.K. Mahajan, K.L.N. Rao; Perforated appendix in a hernial sac mimicking torsion of undescended testis in a neonate; J Pediatr Surg, 43 (2008), pp. e9–e10
- 13 E. Baldassarre, A. Centonze, A. Mazzei, R. Rubino; Amyands hernia in premature twins; Hernia, 13 (2009), pp. 229–230
- 14 J.F. Tycast, A.L. Kumpf, T.L. Schwartz, C.E. Coln; Amyands hernia: a case report describing laparoscopic repair in a pediatric patient; J Pediatr Surg, 43 (2008), pp. 2112–2114
- 15 P. Jain, A. Mishra; Amyands hernia presenting as chronic scrotal sinus; J Indian Assoc Pediatr Surg, 17 (2012), pp. 128–129
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?