Summary
Video-assisted thorascopic surgery (VATS) is a common technique for thoracic operations. Surgery with access via a single port has gradually become popular. We herein report the unusual case of a 53-year-old Japanese male patient whose chest X-rays revealed an abnormal shadow, which continued to increase in size. The tumor was excised by single-port access surgery. The resected tumor was a pedunculated pleural mass, yellowish in color, and pathological diagnosis confirmed a lipoma. We describe the first known successful treatment by single-port VATS.
Keywords
chest wall;lipoma;single port;VATS
1. Introduction
Lipomas are a common type of benign tumor, but are rarely observed in the intrathoracic cavity.1 We describe the first case of single-port video-assisted thorascopic surgery (VATS) to excise a thoracic pleural lipoma with a minimally invasive procedure, and we discuss the advantages and disadvantages of several practical treatments.
2. Case report
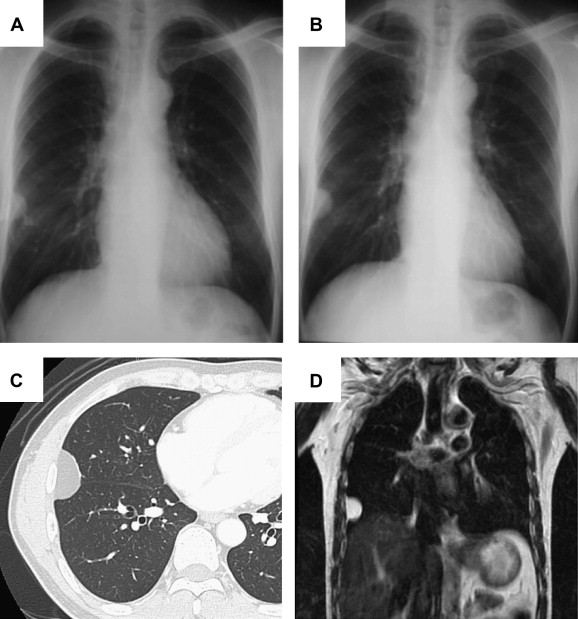
A 53-year-old Japanese male patient was admitted to our hospital after a chest X-ray for a health exam showed an abnormal shadow, which was increasing in size (Figs. 1A and 1B). The patient’s past history, physical examination, and laboratory data were unremarkable. Chest computed tomography (CT) revealed a homogeneous low-density mass measuring 33 mm in diameter arising from the parietal pleura of the thoracic wall. The CT number of the mass was -138 Hounsfield units (HU), indicative of tissue which is composed of fat (Fig. 1C). Magnetic resonance imaging (MRI) demonstrated a high signal intensity mass on both the T1- and T2-weighted images with an extrapleural sign, suggesting the mass originated from the pleura (Fig. 1D). Therefore, the preoperative diagnosis was hypothesized to be thoracic pleural lipoma.
|
|
|
Figure 1. The chest X-ray shows a tumor shadow in the right middle lung field. (A) A 27 × 17 mm tumor in the patient’s chest X-ray in February of 2009. (B) The tumor was 33 × 20 mm in January of 2010; the tumor doubling time was calculated to be 689 days. (C) Chest CT reveals a homogeneous low density mass in the right chest wall. (D) The tumor demonstrates a high signal intensity on the T1- and T2-weighted images following MRI. |
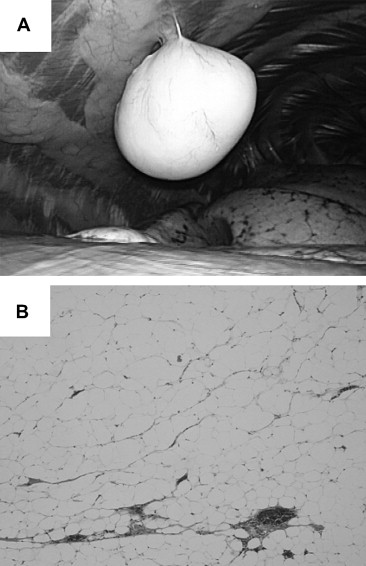
In order to obtain a pathological diagnosis, an operation had to be performed to exclude the possibility of liposarcoma or the infiltrating development of the tumor.1 The patient was explored through the sixth intercostal space using a 12-mm single port: we believed that single-port surgery was feasible for this lesion due to the imaging findings. The thoracoscopic view demonstrated no abnormalities, such as adhesions or a pleural effusion, in the right lateral side of his thoracic cavity. A yellowish tumor sphere was visualized. The pedunculated tumor protruded into the thoracic cavity from the parietal pleura, attached to the pleural surface by its stalk, and moved freely. The tumor was easily extirpated by single-port VATS (Fig. 2A), using an Opti-4 device (Covidien, Tokyo, Japan), which has integrated functions for suction, irrigation, cutting, and coagulation. The tumor was placed in an impermeable bag and removed through the access incision. The histological diagnosis was thoracic pleural lipoma consisting of mature adipose cells (Fig. 2B). There were no malignant findings and positive expression of Ki-67 was seen only sparsely. The patient was discharged after an uneventful recovery on the third day after surgery without excessive analgesic drug treatment. The patient is presently doing well without any tumor recurrence at 1 year after surgery.
|
|
|
Figure 2. (A) The pedunculated tumor was found to protrude into the thoracic cavity from the parietal pleura during the thoracoscopy. (B) The tumor consists of mature adipose cells following hematoxylin and eosin staining. The original image magnification is 40×. |
3. Discussion
The clinical finding of a lipoma, which is mostly observed within the subcutaneous areas of the body, is very common. Thoracic pleural lipomas are, however, relatively rare.1 These well-circumscribed mesenchymal tumors, which originate from adipose tissue, are very slow-growing and therefore tend to develop over many years.1 The tumor in the present case also showed this phenomenon. Tumor growth may be due to cell proliferation, which would show staining for Ki-67. Where this is the case, it is difficult to distinguish between a lipoma and a liposarcoma.1 The management strategy for pleural lipoma is not well established. Radiological follow-up with scans such as CT are useful for diagnosing these patients. However, these examinations are not always adequate for confirming the final diagnosis. Percutaneous needle biopsy is less harmful, although the pathological examination of the specimen is limited.2 Consequently, tumor resection is essential for obtaining a pathological diagnosis.1 An open thoracotomy is easy to perform but is invasive.3 Recently, VATS has become a more common technique for thoracic tumor operations.4 In particular, single-port VATS has been useful for specific diseases, such as polyhydrosis, aided by the incredible advances in operative devices.5 To the best of our knowledge there are no previous reports on the use of single-port VATS for thoracic pleural lipoma in the literature. For the first time, we utilized single-port VATS for both accurate diagnosis and complete extirpation. This procedure is ideal for the following reasons: (1) a pathological examination shows the entire picture of a tumor; (2) this technique is a safe and minimally invasive procedure because most of the pleural lipoma is not directly attached to the lung parenchyma; (3) decreasing postoperative pain and better cosmetic results following surgery can be obtained; (4) it is easy to convert from an open thoracotomy safely, while maintaining an excellent intraoperative view; (5) it is a technique that continues to improve, and it therefore holds promise for achieving subsequent operative advances. This strategy might be applicable for any pleural locations, including the mediastinum, without any limitation for any size. In the current study, the patient did not require excessive analgesics to improve postoperative pain, and was discharged only a short period after surgery. In conclusion, we recommend single-port VATS for the resection of thoracic pleural lipomas with minimal invasiveness.
References
- 1 H. Sakurai, M. Kaji, K. Yamazaki, K. Suemasu; Intrathoracic lipomas: their clinicopathological behaviors are not as straightforward as expected; Ann Thorac Surg, 86 (2008), pp. 261–265
- 2 R.H. Yuan, C.C. Chen, C.L. Chen; Benign chest wall lipoblastoma: report of a case; J Formos Med Assoc, 90 (1991), pp. 419–421
- 3 B.G. O’Riordan, F.J. Daniel, D.R. Fletcher; Open lung biopsy without thoracotomy: technique and possible indications; Aust NZ Surg, 62 (1992), pp. 79–80
- 4 M. Shapiro, T.S. Weiser, J.P. Wisnivesky, C. Chin, M. Arustamyan, S.J. Swanson; Thoracoscopic segmentectomy compares favorably with thoracoscopic lobectomy for patients with small stage I lung cancer; J Thorac Cardiovasc Surg, 137 (2009), pp. 1388–1393
- 5 O. Gigirey Castro, L. Berlanga González, E. Sánchez Gómez; Single port thorascopic surgery using the SILS tool as a novel method in the surgical treatment of pneumothorax; Arch Bronconeumol, 46 (2010), pp. 439–441
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?