Question
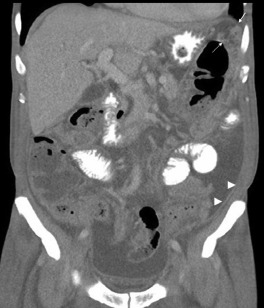
A 64-year-old man presented with abdominal fullness and intermittent night fever for 1 month. His medical history included hemodialysis for 1 year and hypertension. He did not drink alcohol and had no history of chronic hepatitis B or hepatitis C virus infection. There was no body weight loss, cough, or bowel habit change. His physical examination revealed abdominal distension and shifting dullness on percussion. Laboratory workup revealed anemia (hemoglobin, 8.4 g/dL) and hypoalbuminemia (albumin, 2.8 g/dL). The chest radiograph was normal. An abdominal computed tomography with contrast showed ascites, smooth uniform thickening of the peritoneum (arrowhead), omental cakes (arrow; Fig. 1 ), and soft tissue strands with crowded vascular bundles in the small bowel mesentery (Fig. 2 ). The ascitic fluid was cloudy yellow; the analysis revealed a white blood cell count of 950 cells/mm3 with 67% lymphocytes and a total protein level of 4.73 g/dL. Ascitic fluid culture, cytology, cell block, and acid-fast stain yielded negative results.
|
|
|
Figure 1. Contrast-enhanced computed tomography (CT) scan. Note the smooth thickening of the peritoneum (arrowhead), omental cakes (arrow). |
|
|
|
Figure 2. Contrast-enhanced computed tomography (CT) scan. Note the crowded vascular bundles in the small bowel mesentery. |
What is your diagnostic procedure?
- Diagnostic laparoscopy
- Esophagogastroduodenoscopy
- Colonoscopy
- Enteroscopy
What is your impression of this case?
- Peritoneal carcinomatosis
- Peritoneal methothelioma
- Peritoneal tuberculosis
- Peritoneal pseudomyxoma
Answer
Esophagogastroduodenoscopy to exclude malignancy revealed a shallow ulcer at the antrum, and colonoscopy revealed a serrated adenoma in the transverse colon. Diagnostic laparoscopy revealed that the omentum was adherent to the abdominal wall (Fig. 3 ) and the presence of diffuse white nodules in the peritoneum (Fig. 4 ). A peritoneal biopsy showed chronic granulomatous inflammation. The polymerase chain reaction for tuberculosis was positive. The diagnosis of tuberculous peritonitis was reached, and antituberculosis treatment was started. The ascitic fluid culture yielded the same result 2 months later.
|
|
|
Figure 3. Laparoscopy. The omentum is adherent to the abdominal wall. |
|
|
|
Figure 4. Laparoscopy. Diffuse white nodules (arrow) are found in the peritoneum. |
Take home message
The common features of tuberculous peritonitis are ascites, abdominal pain, and fever. The most useful computed tomography findings for distinguishing peritoneal tuberculosis from carcinomatosis in the appearance of the parietal peritoneum. In tuberculosis, the peritoneal thickening is smooth as compared to the nodular peritoneum seen in carcinomatosis. Laparoscopic biopsy is a more rapid method of diagnosing tuberculous peritonitis.
Conflict of interest
All authors declare no conflicts of interest.
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?