Summary
We report a 26-year-old man with 6 years, history of duodenal gastrointestinal stromal tumor (GIST) with liver, peritoneum and lung metastases. He presented with left eye ptosis, diplopia, left facial numbness and a left temporal fossa mass that was confirmed to be GIST with left skull and left orbit metastases. Craniectomy with cranioplasty, tumor excision and decompression were performed. There was an improvement of his visual symptoms and facial numbness. To our knowledge, this is one of the few reports of surgical management of GIST, metastasized to skull and orbit, with good symptomatic relief.
Keywords
GIST;orbit;skull
1. Introduction
Gastrointestinal stromal tumor (GIST) is a rare mesenchymal tumor of the gastrointestinal tract. Like other gastrointestinal tract tumors, abdominal viscera are common sites of metastasis. We present our patient with rare GIST metastasis to the skull and orbit managed by surgery.
2. Case presentation
Our patient was a 26-year-old man who presented in 2004 for passing tarry stool and who was anemic. Esophagogastroduodenoscopy found two polypoid lesions in the duodenum. Biopsy showed that it consisted of small round cells with eosinophilic cytoplasm, no atypia or mitosis. Immunohistochemistry were positive for CD117, CD34 and smooth muscle actin. It was compatible with GIST. Positron emission tomography (PET) and computed tomography (CT) scans showed a duodenal tumor of size 5.6 × 3.4 × 4 cm3 with liver metastases. Imatinib was started and his clinical condition remained static but he required frequent blood transfusion.
In 2006, he developed gastric outlet obstruction caused by the tumor. Gastrojejunostomy was performed to bypass the obstruction. Imatinib was replaced by sunitinib and two percutaneous radiofrequency ablations for the liver metastases were performed. However, the disease continued to progress with lung metastases. Sunitinib was changed to nilotinib.
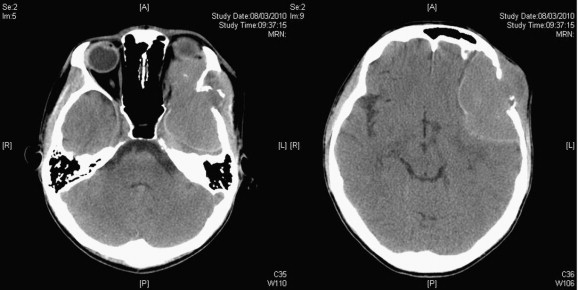
He then complained of left facial numbness and diplopia in February 2010. There was facial asymmetry and his left eye protruded. There was a bulge over the left temporal fossa that was firm and nontender. The overlying skin looked normal. He had diplopia in all gaze but no ophthalmoplegia. There was numbness over the maxillary branch of the left trigeminal nerve. The visual acuities of the right and left eyes were 20/20 and 20/25, respectively, but he complained that the image from the left eye was significantly dimmer. Visual fields of both eyes were full. Magnetic resonance imaging (MRI) showed a 5 cm contrast enhanced lesion over the left temporal region with extension into the left orbit displacing the globe. CT scan showed that the left orbital roof and part of the left temporal bone were eroded by the tumor (Fig. 1). There was also midline shift.
|
|
|
Figure 1. (Left) Preoperative plain computed tomography of the brain showed tumor extending into the orbit with the eyeball displaced and (Right) involved the left temporal region. |
Craniotomy was performed in March 2010. The skin was spared but the temporalis muscle was invaded by the tumor and was partially removed. The tumor had eroded the pterion (Fig. 2). After craniectomy, the tumor was found to have eroded the lateral and superior orbital walls and had compressed onto the globe. Medially, it extended along the greater wing of the sphenoid and had invaded the anterior clinoid process causing optic nerve compression. Inferiorly, it extended to the cavernous sinus and middle cranial fossa. The periorbita and dura were intact. The anterior clinoid process was removed and the optic canal was opened for optic nerve decompression. Because of the extensive skull base involvement, only a partial removal was achieved. The skull defect was repaired with methacrylate (Fig. 3).
|
|
|
Figure 2. Intraoperative photo after the temporalis muscle was lifted up. A reddish soft tumor had eroded through the skull bone and infiltrated the temporalis muscle. |
|
|
|
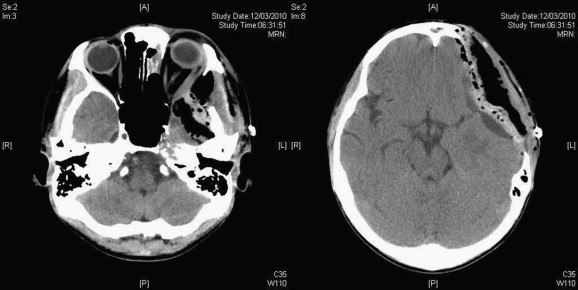
Figure 3. (Left) Postoperative plain computed tomography of the brain showing good decompression of the orbit and (Right) the brain with cranioplasty performed. |
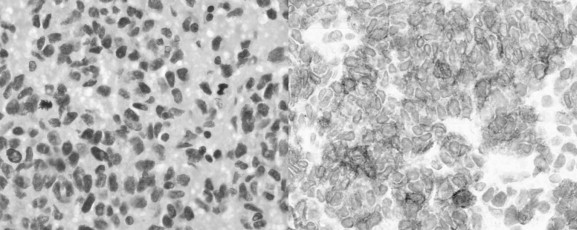
After the operation, proptosis of the left eye was resolved. There was a markedly subjective improvement of diplopia. Vision of the left eye was improved with brighter image. The numbness over the left face had also decreased. The patient was discharged 5 days after the operation. Histology exams showed that the nuclei of the tumor cells were large, hyperchromatic and pleomorphic with coarse chromatin. Mitoses were 23 per 10 high-power fields. Immunohistochemistry was positive for CD117 and CD34 that was compatible with GIST (Fig. 4). He received external beam irradiation and continued nilotinib afterwards.
|
|
|
Figure 4. (Left) Hematoxylin and eosin staining of the tumor and (Right) positive immunohistochemistry staining for CD117 (original magnifications ×40). |
3. Discussion
The head is a rare site for GIST metastases. There have been a few reports on cerebral metastases,1; 2 ; 3 one with clival metastases treated by tyrosine kinase inhibitors (TKI),4 one had skull vault metastasis with excisional biopsy5 and one had metastasis to the orbit and optic canal causing optic nerve compression.6 In the last report, diagnosis was based on clinical grounds with no biopsy taken. External beam irradiation was used, but only achieved pain relief without vision improvement. In comparison, our patient suffered from more extensive involvement causing proptosis. Our surgical decompression provided quick vision improvement, relief from the cerebral compression and good cosmesis. Intact periorbita and dura enabled a relatively safe procedure. As only a partial excision was achieved, external beam irradiation was needed for better disease control. Treatment failure with different TKIs poses difficulties with future planning. It is believed that the disease will recur soon and the value of further surgical resection is doubtful without adjuvant therapy.
Small intestinal GISTs have been shown to be more aggressive than its gastric counterpart.7 Both the size of the primary GIST and mitotic activity are related to biological activities. In our patient, there was no mitotic figure in the duodenum biopsy but there were high mitotic activities in the orbit metastasis. It is uncertain if: 1) the mitotic figure had been properly evaluated from the small duodenal biopsy; 2) this is the usual progress with an increase in mitotic figure; 3) the use of TKIs resulted in clonal selection; or 4) the metastasis represents a clone with high mitotic figure and aggressive behavior while the duodenum tumor remained unchanged. In the last case, further surgery may be warranted as symptomatic control, provided that other systemic tumors remain static.
In summary, this is one of the few reported cases of GIST that metastasized to the skull and orbit, which was managed surgically with good symptomatic relief.
References
- 1 B. Hughes, D. Yip, D. Goldstein, P. Waring, V. Beshay, G. Chong; Cerebral relapse of metastatic gastrointestinal stromal tumor during treatment with imatinib mesylate: case report; BMC Cancer, 4 (2004), p. 74
- 2 S. Kaku, T. Tanaka, T. Ohtuka, et al.; Perisacral gastrointestinal stromal tumor with intracranial metastasis. Case report; Neurol Med Chir (Tokyo), 46 (2006), pp. 254–257
- 3 T. Puri, G. Gunabushanam, M. Malik, et al.; Mesenteric gastrointestinal stromal tumour presenting as intracranial space occupying lesion; World J Surg Oncol, 4 (2006), p. 78
- 4 J. Barrière, J. Thariat, F. Vandenbos, P.Y. Bondiau, I. Peyrottes, F. Peyrade; Diplopia as the first symptom of an aggressive metastatic rectal stromal tumor; Onkologie, 32 (2009), pp. 345–347
- 5 I. Gil-Arnaiz, J. Martínez-Trufero, R.A. Pazo-Cid, F. Felipo, M.J. Lecumberri, V. Calderero; Skull metastasis from rectal gastrointestinal stromal tumours; Clin Transl Oncol, 11 (2009), pp. 625–627
- 6 K. Akiyama, J. Numaga, F. Kagaya, et al.; Case of optic nerve involvement in metastasis of a gastrointestinal stromal tumor; Jpn J Ophthalmol, 48 (2004), pp. 166–168
- 7 M. Miettinen, H. Makhlouf, L.H. Sobin, J. Lasota; Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up; Am J Surg Pathol, 30 (2006), pp. 477–489
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?