Summary
Introduction
Single-incision laparoscopic cholecystectomy (SILC) is an evolving concept in minimally invasive surgery. It utilizes the concept of inline viewing and a single incision that accommodates all of the working instruments. Here, we describe a single surgeons initial experiences of using this technique in a tertiary hospital.
Methods
Between January and September 2010, 21 patients underwent SILC for symptomatic cholelithiasis. The umbilicus was the point of access into abdomen for all patients using a 2.0–2.5-cm incision. The surgeries were performed using the Covidien SILS port with a 30° angled scope and two 5-mm conventional laparoscopic instruments.
Results
Nineteen patients successfully underwent surgery (8 males and 11 females; mean age: 43 years). The mean body mass index was 25.9 kg/m2 (range: 19.0–38.2 kg/m2). The mean operative time was 89 minutes (range: 55–135 minutes). Minimal blood loss was noted in each patient. The mean length of the postoperative stay was 1.1 days (range: 1–3 days). No complications or mortalities were associated with the technique. The visual analogue score for pain at the 1-day and 6-week follow-up examinations was 2 (range: 1–7) and 0.6 (range: 0–3), respectively. At 6 weeks, the mean satisfaction score for the resultant scar was 8.8 (range: 4–10) and the mean overall satisfaction score was 9.2 (range: 7–10). The mean time until returning to work or normal activities was 8.8 days (range: 1–21 days).
Conclusion
SILC is feasible and demonstrates a good clinical outcome.
Keywords
cholecystectomy;single-incision laparoscopic surgery;single-incision laparoscopic cholecystectomy;SILS;transumbilical access
1. Introduction
Erich Muhe performed the worlds first laparoscopic cholecystectomy in 1985 using a modified laparoscope called the galloscope.1 The advent of the digital camera allowed Phillipe Mouret to perform the first video-assisted laparoscopic cholecystectomy in 1987.2 However, when laparoscopic cholecystectomy made its American debut in 1989, it was greeted with skepticism by many surgeons (and with total disdain by some) because it challenged one of our safest and most effective operative procedures, as described by Dr. John Cameron in the Annals of Surgery in 1991. 3 Cameron further pointed out that it was an “almost totally consumer driven” innovation that allowed conventional laparoscopic cholecystectomy to supplant open cholecystectomy as the gold standard for the treatment of symptomatic cholelithiasis in the 20th century.3 The turn of the century witnessed another paradigm shift in the practice of minimally invasive surgery. One of the emerging concepts is single-port or single-incision laparoscopic surgery (SILS). Again, surgeons are reevaluating the gold standard in the face of technological innovation. The fundamental idea is to have all working ports enter the abdomen through a single incision, utilizing the concept of inline viewing which evolved following the development of natural orifice transluminal endoscopic surgery (NOTES). However, SILS contradicts the principle of conventional laparoscopy which advocates triangulation around a central optical instrument. To the best of our knowledge, here we report the first initial clinical experiences of performing laparoscopic cholecystectomy using single-port transumbilical access in Malaysia. The purpose of this series is to describe the safety and feasibility of performing singe-incision laparoscopic cholecystectomy in a tertiary hospital.
Sarawak General Hospital is the main tertiary referral center for the entire state of Sarawak and its population of 2.3 million people. More than 200 conventional laparoscopic cholecystectomies are performed annually with acceptable complication rates. The main author (SLS) is an experienced laparoscopic surgeon and trained in the advanced use of laparoscopic surgery. He routinely performs conventional laparoscopic cholecystectomy and has performed more than 300 advanced laparoscopic gastrointestinal and colorectal procedures.
2. Patients and methods
Between January 2010 and September 2010, 21 patients underwent SILC. The umbilicus was the point of access into abdomen in all patients. All of the operations were performed consecutively by a single surgeon who had completed a fellowship in minimally invasive surgery. Patients were informed about this novel technique and written consent was obtained prior to participation. The inclusion criteria included symptomatic cholelithiasis in male or female patients older than 18 years and an American Society of Anesthesiology (ASA) score of 1 or 2. Patients with a previous history of gallstone complications (e.g., acute cholecystitis, cholangitis, pancreatitis, or choledocholithiasis), previous upper abdominal surgery, known cirrhosis of the liver, and an ASA score of 3 or higher were excluded. All patients underwent preoperative ultrasonography and baseline liver functions were determined. Data were prospectively collected using a comprehensive questionnaire that included age, sex, weight (kg), height (cm), operative technique, operative time (minutes), complications, postoperative pain score as estimated using the visual analogue scale (VAS), postoperative hospital stay (days), and mortality.
Within 6 weeks after surgery, patients were asked to assess their satisfaction with the operational outcome and resulting scar on a scale of 10 (10 being the most satisfied) and the time required to return to work or normal activities. Operative time, length of stay, and complications were used as measurements of clinical outcome.
2.1. Operative techniques for SILC
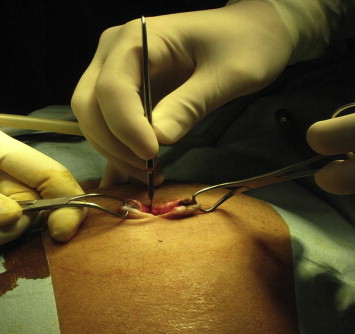
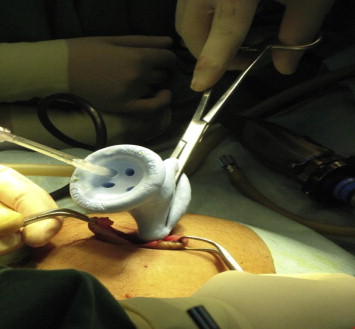
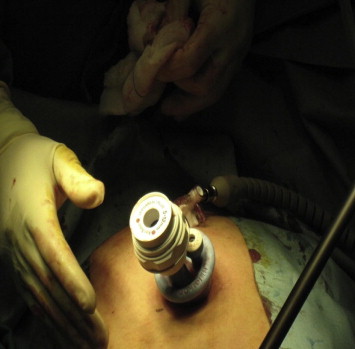
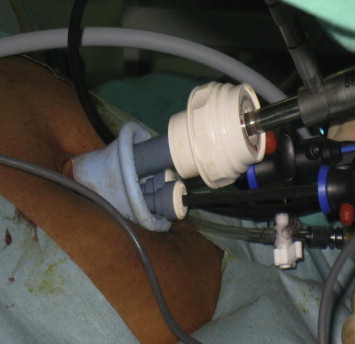
Patients were placed in a supine position with the surgeon standing between the legs and the assistant to the right of the patient. A television monitor and the insufflator system Karl Storz HD were placed to the left of the patient. A 2.0–2.5 cm vertical subumbilical skin incision was made and directed down into the peritoneum (Fig. 1). A special single incision port (Covidien SILS™ port, USA) was placed into position through the incision using a Kelly clamp (Covidien, USA) (Fig. 2). The port is made from an elastic polymer, is slightly hourglass-shaped, and contains four openings: one for insufflation via a right-angled tube and three that can accommodate trocars sized between 5–12 mm (Figs. 3 and 4).4 After pneumoperitoneum was established, a 10-mm trocar and two 5-mm trocars were then inserted through the SILS port. We used a 10-mm 30° laparoscope and two standard laparoscopic instruments (usually a hook and a grasper) to perform the surgery. A straight grasper was used at the infundibulum for lateral retraction. Clipping and division of the cystic duct and artery were then performed in the same manner as conventional 3- to 4-port laparoscopic cholecystectomy. In one patient, a suture on a Keith needle was subcostally placed into the operative field and then through the fundus of the gallbladder for cephalad retraction. Following successful dissection of the gallbladder from the liver bed, 10-mm 30° camera was exchanged for a 5-mm 0° camera. A specimen grasper was placed into the 10-mm trocar to facilitate retrieval of the gallbladder. The abdomen was deflated by the removal of the 5-mm and 10-mm trocars from the SILS port. The gallbladder was removed through the umbilical wound following disengagement of the SILS port (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 ; Figure 6).
|
|
|
Figure 1. Transumbilical incision. |
|
|
|
Figure 2. Insertion of the SILS port using a Kelly clamp. |
|
|
|
Figure 3. Insufflation. |
|
|
|
Figure 4. The flexible triport that permits the introduction of two 5-mm and one 12-mm trocars. |
|
|
|
Figure 5. Umbilical wound immediately after surgery. |
|
|
|
Figure 6. No visible scar at 6-weeks postsurgery. |
After the operations were completed, the SILS™ port was removed and the umbilical fascia was closed using Vicryl O J needle (Johnson & Johnson, USA). The umbilical skin was approximated using 4-0 monocryl (Johnson & Johnson, USA) subdermal stitches (Fig. 5).
3. Results
The characteristics of the patients and the operative and outcome data are detailed in Table 1. Twenty-one patients were selected to undergo SILC between January 2010 and September 2010. Of 21 patients, 19 (90.5%) successfully underwent SILC. For one patient, the technique was quickly abandoned because the conventional grasper could not reach the gallbladder from the umbilical position due to the patients long upper abdomen. The distance between the xiphisternum and the umbilicus was measured to be 24 cm. The patient was “converted” to conventional three-trocar laparoscopic cholecystectomy. The second patient required an additional 5-mm port due to the large caudate lobe overlying Calots triangle; therefore, the critical view of Calots triangle was compromised. These patients were excluded from further analysis. Of 19 patients, 11 (57.9%) were female, the mean age was 43 years (range: 29–69 years) and the mean body mass index (BMI) was 25.9 kg/m2 (range: 19.0–38.2 kg/m2). The mean operative time was 89 minutes (range: 55–135 minutes). Blood loss was minimal in all cases. No bile spillage was encountered during the procedure and no drains were placed in any case. The length of the postoperative stay was 1.1 days (range: 1–3 days). Regarding postoperative pain, the mean VAS scores at the 1-day and 6-week follow-up examinations were 2 (range: 1–7) and 0.6 (range: 0–3), respectively. None of the patients reported pain that interfered with normal or work activities. No postoperative complications were observed, except one patient developed shortness of breath on postoperative day 1. She was suspected of having a pulmonary embolism because of a positive D-dimer test. However, computed tomography of the thorax was normal. She was conservatively managed on oxygen and uneventfully discharged on postoperative day 3.
| Number of successful SIL cholecystectomies | 19 |
| Gender (M/F) (n) | 8/11 |
| Mean age ± SD (y) | 43 ± 2.6 |
| Mean BMI ± SD (kg/m2) | 25.9 ± 4.6 |
| Mean operative time ± SD (min) | 89 ± 23.5 |
| Blood loss | Minimal in 100% |
| Mean length of postoperative stay ± SD (d) | 1.1 ± 0.46 |
| Postoperative pain VAS score on 1 day ± SD (/10) | 2 ± 2.05 |
| Complications (n) | Shortness of breath (1) |
| Pathology (%) | Chronic cholecystitis (84.2%) |
| Cosmesis score ± SD (/10) | 8.8 ± 1.7 |
| Overall satisfaction score ± SD (/10) | 9.2 ± 1.0 |
| Return to work or normal activities ± SD (d) | 8.8 ± 6.7 |
BMI, body mass index; SD, standard deviation; VAS, visual analogue scale. Note: Two patients were excluded from this analysis.
At the 6-week follow-up examination, almost all of the patients were satisfied with the resultant scar (Fig. 6), reporting a mean satisfaction score of 8.8 (range: 4–10). The mean overall satisfaction score was 9.2 (range: 7–10). The mean time required before returning to work or normal activities was 8.8 days (range: 1–21 days).
Pathological data are available for all 19 patients. Sixteen (84.2%) patients had been diagnosed with chronic cholecystitis and three (15.8%) with acute cholecystitis. Although it was our intention to select patients with symptomatic cholelithiasis without signs of inflammation, we could not avoid enrolling patients with previous recurrent bouts of attack or even acute attack. This shows that most of our patients presented with late onset.
4. Discussion
Single-incision or single-port laparoscopic surgery is a new concept in minimally invasive surgery that has captured the attention of surgeons, patients, and the medical industry. Navarra et al first described a series of 30 SILC in 1997 that utilized two 10-mm ports and three transabdominal stay sutures to aid in gallbladder retraction. The two umbilical fascial incisions were connected at the end of the case to facilitate the removal of the gallbladder.5 Further reports on the use of transumbilical SILC were reported in 1999,6 ; 7 which was followed by a decade of little reporting on this technique in the literature. From 2008 onwards, there has been a renewed interest in SILC and several authors have reported encouraging results in terms of feasibility and safety.8; 9; 10; 11; 12; 13; 14; 15; 16; 17; 18; 19 ; 20
As surgeons start to adopt this technique, there is a need to observe both its risk and benefits. The major concern regarding this technique is the risk of common bile duct injury. Early experiences with laparoscopic cholecystectomy were associated with higher rates of common bile duct injuries.21 Laparoscopic cholecystectomy in the emergency setting for acute cholecystitis is associated with three times higher incidence of bile duct injury compared with elective cholecystectomy.22 With these considerations in mind, we avoided performing SILS cholecystectomy in any patients who presented with acute cholecystitis in the acute setting.
Like all new procedures, SILC has its own unique learning curve. The surgeon needs to learn how to navigate the instruments using a limited range of movement and develop an understanding with camera wielding assistant. The surgeon needs to learn to adapt to the instruments clashing at the point of entry into the abdominal cavity and to make necessary adjustments to inadvertent movements of the adjacent instrument during the maneuvering of the camera. It has been reported that the learning curve for a fellowship-trained laparoscopic surgeon to become proficient at SILC is approximately 10 cases.23 However, our experience suggests that while surgeons may become proficient after 10 cases, the operating time is not significantly altered due to anatomical difficulties in certain patients. Maybe a larger series will be able to delineate the learning curve in terms of operative time.
Obese patients with BMI > 30 could pose potential risks to SILC due to the presence of fatty liver. To overcome this problem, we advised our patients to go on a high-protein, low-carbohydrate, and low-fat diet a week before the surgery. Our preliminary results indicate the feasibility of performing the procedure with the only disadvantage being a longer operative time.
Some authors advocate the use of articulating instruments for achieving local triangulation.9; 16; 17; 19; 20 ; 23 Our initial experiences indicate that conventional laparoscopic instruments are feasible for use in SILC. The technical challenges that we encountered during the surgery included the clashing between the instruments and the optic cable of the laparoscope, inadequate retraction of the gallbladder and exposure of the Calots triangle, inadequate length of the instrumentation, and smoke entrapment in the abdominal cavity. We believe that in order to enhance the ergonomics and the comfort of using conventional laparoscopic instruments, it is important to use an extra-long scope with a cable that is connected to the posterior rather than the lateral aspect in order to allow the full rotation of the 30° laparoscope without interference to the operative instruments. Furthermore, the use of instruments with a low profile, streamlined handpieces that reduce external crowding, and a separate venting channel to release intra-abdominal smoke could make the surgery less stressful for the surgeon.
Gallbladder anchorage using the sutures are said to improve the operative field.9 This allows the surgeon to “puppeteer” the gallbladder, thus replicating the movements that would normally be performed by the surgeons left hand in a conventional laparoscopic cholecystectomy.9 In one patient, we used a transabdominal stay suture to suspend the gallbladder fundus because the gallbladder was of considerable size and folded in on itself at the junction of the fundus with body, rendering the retraction of the gallbladder and exposure of Calots triangle difficult. However, it left no scar in the abdominal wall. Ersin et al suggested that in order to achieve favorable results, the suspending suture should be located in the thoracoabdominal region. 20
Regarding safety, we feel that SILC is feasible, but not necessarily as safe as conventional 3- to 4-port laparoscopic cholecystectomy. Meticulous attention to detail and early conversion for difficult situations must be maintained at all times. It cannot be stated clearly enough that if an adequate critical view is a limiting factor, the use of an extraumbilical port or conversion to a 3- or 4-port surgery should be performed. This should not be considered as a failure or complication.
SILC represents an advancement in the field of minimally invasive surgery. However, it remains to be determined whether this approach would benefit patients, other than for cosmetic purposes, in comparison with conventional laparoscopic cholecystectomy. Additional prospective randomized controlled trials are needed to examine its feasibility and safety.
5. Conclusions
SILS represents a new concept in minimally invasive surgery. It is possible that the public will demand this surgical approach much in the same way that it forced the explosion in the use laparoscopic surgery two decades ago. Conceptual development through human experiences and the introduction of new dedicated instruments may be the key to unlocking its potential. As for the present, we believe SILC should be performed by surgeons with significant experience in advanced laparoscopy.
Acknowledgments
We would like to thank the Director General of Health, Malaysia for allowing us to publish this paper.
References
- 1 E. Muhe; Die erste: cholecystecktomie durch das laparoskop (The first laparoscopic cholecystectomy); Langenbecks Arch Surg, 369 (1986), p. 804
- 2 A.M. Kaiser, M.L. Corman; History of laparoscopy; Surg Oncol Clin N Am, 10 (2001), pp. 483–492
- 3 J.L. Cameron, T.R. Gadacz; Laparoscopic cholecystectomy; Ann Surg, 213 (1) (1991), pp. 1–2
- 4 J.R. Romanelli, D.B. Earle; Single-port laparoscopic surgery: an overview; Surg Endosc, 23 (2009), pp. 1419–1427
- 5 G. Navarra, E. Pozza, S. Occhionorelli, et al.; One-wound laparoscopic cholecystectomy; Br J Surg, 84 (1997), p. 695
- 6 F. Bresadola, A. Pasqualucci, A. Donini, et al.; Elective transumbilical compared with standard laparoscopic cholecystectomy; Eur J Surg, 165 (1999), pp. 29–34
- 7 J. Piskun, S. Rajpal; Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus; J Laparoendosc Adv Surg Tech, 9 (1999), pp. 361–364
- 8 P. Bucher, F. Pugin, N. Buchs, et al.; Single port access laparoscopic cholecystectomy (with video); World J Surg, 33 (2009), pp. 1015–1019
- 9 A. Chow, S. Purkayastha, P. Paraskeva; Appendicectomy and cholecystectomy using single-incision laparoscopic surgery (SILS): the first UK experience; Surg Innov, 16 (2009), pp. 211–217
- 10 K. Dunning, H. Kohli; Transumbilical laparoscopic cholecystectomy: a novel technique; Arch Surg, 144 (10) (2009), pp. 957–960
- 11 T.H. Hong, Y.K. You, K.H. Lee; Transumbilical single-port laparoscopic cholecystectomy-scarless cholecystectomy; Surg Endosc, 23 (2009), pp. 1393–1397
- 12 A. Kirschniak, S. Bollmann, R. Pointner, et al.; Transumbilical single-incision laparoscopic cholecystectomy: preliminary experiences; Surg Laparosc Endosc Percutan Tech, 19 (6) (2009), pp. 436–438
- 13 T.E. Langwieler, T. Nimmesgern, M. Back; Single-port access in laparoscopic cholecystectomy; Surg Endosc, 23 (2009), pp. 1138–1141
- 14 H. Rivas, E. Varela, D. Scott; Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients; Surg Endosc, 24 (2010), pp. 1403–1412
- 15 K.E. Roberts, D. Solomon, A.J. Duffy, et al.; Single-incision laparoscopic cholecystectomy: a surgeons initial experience with 56 consecutive cases and a review of the literature; J Gastrointest Surg, 14 (2010), pp. 506–510
- 16 J.R. Romanelli, T.B. Roshek III, D.C. Lynn, et al.; Single-port laparoscopic cholecystectomy: initial experience; Surg Endosc, 24 (2010), pp. 1374–1379
- 17 R. Tacchino, F. Greco, D. Matera; Single-incision laparoscopic cholecystectomy: surgery without a visible scar; Surg Endosc, 23 (2009), pp. 896–899
- 18 P.G. Curcillo II, A.S. Wu, E.R. Podolsky, et al.; Single-port-access (SPA(TM)) cholecystectomy: a multi-institutional report of the first 297 cases; Surg Endosc, 24 (2010), pp. 1854–1860
- 19 J. Erbella Jr., G.M. Bunch; Single-incision laparoscopic cholecystectomy: the first 100 outpatients; Surg Endosc, 24 (2010), pp. 1958–1961
- 20 S. Ersin, O. Firat, M. Sozbilen; Single-incision laparoscopic cholecystectomy: is it more than a challenge?; Surg Endosc, 24 (2010), pp. 68–71
- 21 J.A. Shea, M.J. Healey, J.A. Berlin, et al.; Mortality and complications associated with laparoscopic cholecystectomy: a meta-analysis; Ann Surg, 224 (1996), pp. 609–620
- 22 S.M. Strasberg; Avoidance of biliary injury during laparoscopic cholecystectomy; J Hepatobiliary Pancreat Surg, 9 (2002), pp. 543–547
- 23 K.E. Roberts, D. Solomon, A.J. Duffy, et al.; Single-incision laparoscopic cholecystectomy: a surgeons initial experience with 56 consecutive cases and review of the literature; J Gastrointest Surg, 14 (3) (2010), pp. 506–510
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?