Highlights
- Melatonin partially eliminates the AIA/DDC-induced decrease in the activity of the gluconeogenic enzymes PEPCK and G6Pase.
- Melatonin favors a glucose-mediated down-regulating effect on AIA/DDC-induced ALA-S.
- Melatonin reduces AIA/DDC-increases in lipid peroxidation.
- Melatonin partially reverts the AIA/DDC-induced increase in ALA and PBG levels.
- The results obtained suggest the hypothetical use of Mel as co-treatment for acute porphyria.
Abstract
This work investigated the modulation by melatonin (Mel) of the effects of the porphyrinogenic drugs 2-allyl-2-isopropylacetamide (AIA) and 3,5-diethoxycarbonyl-1,4-dihydro-2,4,6-collidine (DDC) on oxidative environment, glucose biosynthesis and heme pathway parameters. Administration of Mel before rat intoxication with AIA/DDC showed a clear beneficial effect in all cases. Mel induced decreases of 42% and 35% in the excretion of the hemeprecursors 5-aminolevulinic acid (ALA) and porphobilinogen (PBG), respectively, and a 33% decrease in the induction of the heme regulatory enzyme 5-aminolevulinic acid-synthase (ALA-S). The activity of the glucose metabolism enzyme phosphoenolpyruvate carboxykinase (PEPCK), which had been diminished by the porphyrinogenic treatment, was restored by 45% when animals were pre-treated with Mel. Mel abolished the modest decrease in glucose 6-phospatase (G6Pase) activity caused by AIA/DDC treatment. The oxidative status of lipids was attenuated by Mel treatment in homogenates by 47%, whereas no statistically significant AIA/DDC-induced increase in thiobarbituric acid reactive substances (TBARS) was observed in microsomes after Mel pre-treatment. We hypothesize that Mel may be scavenging reactive species of oxygen (ROS) that could be damaging lipids, PEPCK, G6Pase and ferrochelatase (FQ). Additionally, Mel administration resulted in the repression of the key enzyme ALA-S, and this could be due to an increase in glucose levels, which is known to inhibit ALA-S induction. The consequent decrease in levels of the heme precursors ALA and PBG had a beneficial effect on the drug-induced porphyria. The results obtained open the possibility of further research on the use of melatonin as a co-treatment option in acute porphyria.
Chemical compounds studied in this article
Melatonin (PubChem CID: 896) ; Allylisopropylacetamide (PubChem CID: 9297) ; 3,5-Diethoxycarbonyl-1,4-dihydro-2,4,6-collidine (PubChem CID: 12446) ; Heme (PubChem CID: 26945) ; 5-Aminolevulinic acid (PubChem CID: 137) ; Porphobilinogen (PubChem CID: 1021)
Keywords
Melatonin ; Glucose synthesis ; Heme pathway ; Acute porphyria ; Oxidative stress
1. Introduction
Melatonin (Mel), which derives from the serotoninergic pathway of tryptophan, is a neurohormone with antioxidant properties [28] . It is mainly produced in the pineal gland but also in other organs. Mel has a number of physiological effects including the regulation of circadian rhythms, oncostasis, stimulation of the immune system and the regeneration of sexual activity, as well as being anti-inflammatory [8] . Mel has been identified as a powerful direct free radical scavenger and an antioxidant of broad spectrum even more potent than glutation (GSH). It can cross the hemato-encephalic and placental barriers [32] and [29] . Numerous investigations have shown its ability to reduce the molecular damage caused by reactive species of oxygen (ROS) and reactive nitrogen species (RNS) [8] ).
Porphyrias are hereditary disorders caused by a de-regulation of the heme pathway due to deficiencies in the activity of some of its enzymes, which lead to the accumulation of heme precursors and diminished heme formation. This deficiency triggers the induction of the regulatory enzyme 5-aminolevulinic acid-synthase (ALA-S) [3] . Life-threatening acute porphyrias are biochemically characterized by the accumulation of heme precursors such as 5-aminolevulinic acid (ALA), which promotes oxidative stress by generating ROS [3] and [6] .
The porphyrinogenic drug 2-allyl-2-isopropylacetamide (AIA) enhances the destruction of liver heme, particularly cytochrome P-450, whereas the porphyrinogenic drug 3,5-diethoxycarbonyl-1,4-dihydro-2,4,6-collidine (DDC) strongly depletes heme by combination of heme destruction and inhibition of heme synthesis [18] . AIA/DDC treatment results in acute heme deficiency, an impairment of ferrochelatase (FQ) activity, a marked de-repression of ALA-S and, as a consequence, an exacerbated production of ALA and other heme precursors in the liver [14] . This combined treatment has been reported to induce a rat experimental porphyria resembling quite accurately acute variegate porphyria [14] . Accumulated ALA has been associated with iron-mediated oxidative damage to biomolecules and cell structures through ROS generation [6] . ROS are able to oxidize nucleic acids, proteins, lipids, and carbohydrates, affecting key cellular functions [6] . It has been demonstrated that AIA/DDC treatment promotes the establishment of an oxidative environment with increases in ROS [14] .
Glucose administration is known to have beneficial effects on acute porphyria patients, significatively improving biochemical parameters and clinical conditions [3] . The prevention of acute experimental porphyria through a carbohydrate-rich diet in animal models illustrates the effect of glucose, which prevents the induction of the heme pathway regulatory enzyme ALA-S [33] . Furthermore, it has been reported that treatment with AIA/DDC hinders gluconeogenesis and glycogenolysis leading to a reduction in glucose availability in hepatocytes. In particular, hepatic phosphoenolpyruvate carboxykinase (PEPCK) and glycogen phosphorylase (GP) activities have been found impaired in AIA/DDC-induced rat porphyria [14] and [20] .
The relationship between carbohydrates and oxidative status with porphyria, plus the known anti-oxidant and radical-scavenging properties of Mel, prompted the present investigation about Mel as a possible modulator of AIA/DC-induced experimental porphyria. Effects were studied at the level of oxidative environment, glucose biosynthesis and heme pathway by measuring key enzymes of the heme and glucose pathways as well as porphyria and lipid peroxidation markers.
2. Materials and methods
2.1. Materials
AIA was a gift from Roche Co. (Germany). DDC was purchased from Aldrich Chemical Company Inc. (Milwaukee, WI). Melatonin, bovine serum albumin, deoxyguanosine 5′-diphosphate, glucose-1-phosphate, malate dehydrogenase, NADH, Dowex 1, Dowex 50 W and thiobarbituric acid were obtained from Sigma Chemical Co. (St. Louis, MO). All other chemicals were of analytical grade.
2.2. Animal treatments
Female Wistar rats (180–200 g) were purchased from the National Committee of Atomic Energy (CONEA, Argentina). They were maintained on food and water ad libitum and housed under conditions of controlled temperature (25 °C) and light (12 h light–dark cycle, light from 6am to 6pm).
Animals were treated according to International Guidelines (Guide for Care and Use of Laboratory Animals, National Research Council, USA, 1996, the Council of the European Communities Directive, 86/609/ECC) and to guidelines from the Animal Care and Use Committee of the Argentine Association of Specialists in Laboratory Animals (AADEALC). AIA was dissolved in saline solution (0.9% NaCl, w/v) and DDC was dissolved in corn oil [5] just before administration. Melatonin was dissolved in pure ethanol. The solution was protected from light and kept at 4 °C until injection. Ethanolic stocks were diluted with 0.9% NaCl (w/v) to achieve a ratio 0.9% NaCl/ethanol of 20/1 (v/v, melatonin vehicle). Mel was dissolved in saline just before being ip administered.
A total of 3 experiments were performed, each involving 8 randomly selected animals divided in 4 groups of 2 animals. The four groups were as follows: “−Mel,−AIA/DDC”, not pretreated with Mel nor treated with AIA/DDC; “−Mel,+AIA/DDC”, not pretreated with Mel and treated with AIA/DDC; “+Mel,−AIA/DDC”, pretreated with Mel but not treated with AIA/DDC; and “+Mel,+AIA/DDC”, pretreated with Mel and then treated with AIA/DDC. Mel (10 mg/kg) body weight (bw) or Mel vehicle were intraperitoneally (ip) injected 3 times a day at 8am, 12pm and 4pm during 2 days. At the end of this treatment, intoxication with AIA (300 mg/kg), bw, subcutaneously (sc) and DDC (50 mg/kg bw, ip) was performed. In the case of controls, Mel, AIA and DDC vehicles were administered. Mel dosage was based on studies about its drug toxicity-reduction and drug protective ability [27] , [11] and [13] . Rats were fasted 8 h before and 16 h after intoxication. Access to drinking water was free. Parameters were measured in duplicate at 16 h post-intoxication, in all cases. Urine was collected during the whole period of 16 h after intoxication by using individual metabolic cages for each animal.
2.3. Liver extracts
Rats were euthanized by carbon dioxide inhalation followed by decapitation, 16 h after AIA/DDC administration. Animals had been fasted for a total of 24 h before death, as this has been previously shown to result in reliable measurements of PEPCK and glucose 6-phospatase (G6Pase) activities [22] . Livers previously perfused with ice-cold saline solution, were removed and portions from them were homogenized in a Potter-Elvehjem homogenizer using different solutions according to the assays to be performed, in all cases at 0–4 °C. Liver portions of approximately 1 g were excised and immediately homogenized in 3 ml of a solution containing 0.9% NaCl, 0.1 mM Tris–HCl pH 7.4 and 0.5 mM EDTA. These extracts were employed to determine ALA-S activity [19] . For PEPCK activity, liver was homogenized (1:3 w/v) in 0.25 M sucrose. Homogenates were centrifuged for 1 h at 100000xg and the resulting supernatants were used for PEPCK activity measurements while the pellets, properly resuspended, were used for microsomal G6Pase enzymatic determination. All procedures were carried out at 4 °C. For hepatic FQ determination, homogenates were prepared with 0.154 M KCl (1:5 w/v). Homogenates were centrifuged for 25 mim at 11000xg and the resulting pellets were frozen until hepatic FQ activities were determined. Lipid peroxidation was determined in homogenates (those used also for PEPCK activity tissue preparations) and microsomal fractions (those used also for G6Pase enzymatic determination)
2.4. Metabolite levels and enzyme assays
2.4.1. 5-Aminolevulinic acid and porphobilinogen in urine
0.3–1.0 ml samples from urine collected during 16 h after intoxication adjusted to pH 4.5–6.0, was placed on the top of two column, anion–cation exchange assembly as described by Piper et al. [25] . Then the column assembly was washed three time with 8 ml of distilled water and then the columns were separated. PBG, bound to the anion exchange Dowex 1 column, was eluted by 2 ml of 1 M acetic acid followed by 3 ml of 0.2 M acetic acid, whereas ALA bound to the cation exchange Dowex 50W column was eluted with 7 ml of 1 M sodium acetate. ALA pyrrole and PBG were determined colorimetrically as described by Mauzerall and Granick [21] .
2.4.2. 5-Aminolevulinic acid synthase activity
ALA-S activity was assayed in whole liver homogenates by the method of Marver et al. [19] . Incubation mixtures containing 0.1 M glycine, 0.01 M EDTA, 0.08 M Tris–HCl buffer pH 7.2 and 0.5 ml of homogenate in a final volume of 2 ml were incubated at 37 °C for 60 min. The reaction products were determined spectrophotometrically at 553 nm [21] .
2.4.3. Ferrochelatase activity
FQ activities were measured in liver mitochondrial fractions. Pellets containing mitochondria were used after being frozen at −20 °C for 24–48 h. Enzymatic activities were determined in resuspended pellets, using protoporphyrin IX as substrate, as described by Porra and Jones [26] .
2.4.4. Phosphoenolpyruvate carboxykinase activity
PEPCK was measured according to Petrescu et al. [24] using deoxyguanosine 5′-diphosphate as the substrate, and 100,000 × g homogenate supernatant of as the enzyme source (Section 2.3 ). The oxaloacetate formed during the reaction was determined spectrophotometrically at 340 nm by reduction with malate dehydrogenase in the presence of NADH.
2.4.5. Glucose 6-phosphatase activity
G6-Pase was measured as described by Baginski et al. [2] . The release of inorganic phosphate from glucose-6-phosphate was measured through the formation of the phosphomolybdate complex and its reduction by ascorbic acid, which is quantified spectrophotometrically at 700 nm [1] . Pellets obtained from liver homogenates, containing approximately 40 μg protein, were used as the source of enzyme activity, as described in Section 2.3 .
2.4.6. Lipid peroxidation
Lipid peroxidation was determined by measuring the rate of generation of thiobarbituric acid reactive substances (TBARS) using whole homogenates and microsomes from liver. The red malonyldialdehyde–thiobarbituric acid complex produced was extracted with butanol to avoid interference by endogenous porphyrins. TBARS content was measured by its absorbance at 532 nm, using the molar absorption coefficient 156,000 M−1 cm−1[23] .
2.4.7. Protein determination
Protein concentrations were measured according to Lowry et al. [16] using bovine serum albumin as standard.
2.5. Statistical analysis
Figure data are expressed as means (±SEM) of six animals, i.e. combining together the animals of the same group from all three experiments. Data were subjected to analysis of variance (ANOVA) with two factors: Mel pre-treatment and AIA/DDC treatment. Multiple comparisons among groups were performed using Tukey–Kramer’s test. Differences were considered significant when p < 0.05. Before statistical analysis, data were tested for normality and uniformity of variance using Lilliefors and Bartlett’s tests, respectively.
3. Results
3.1. Heme pathway parameters
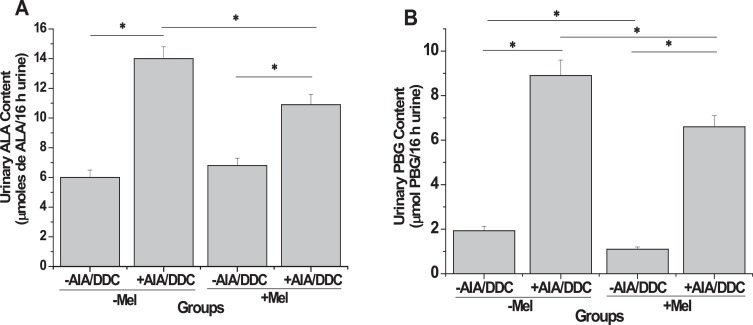
The levels of total urinary excretion of ALA and PBG indicate the severity of porphyric conditions. The porphyrinogenic AIA/DDC treatment induced statistically significant increases of 137% for ALA and 356% for PBG, in the absence of melatonin pre-treatment (“−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 1 A and B). Mel pre-treatment resulted in a 25% decrease (p < 0.05) in the total amount of ALA formed under drug treatment (“−Mel,+AIA/DDC” vs “+Mel,+AIA/DDC”, Fig. 1 A). A comparison of the drug-induced ALA increases in the absence of Mel (“−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 1 A) with those in the presence of Mel (“+Mel,+AIA/DDC” vs “+Mel,−AIA/DDC”, Fig. 1 A), a Mel-induced decrease of 42% (p < 0.05) in ALA accumulation is apparent. The total amount of PBG formed after drug treatment was smaller by 28% (p < 0.05) as a result of Mel pre-treatment (“+Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 1 B). A comparison of the drug-induced PBG increases in the absence of Mel (“−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 1 B) with those in the presence of Mel (“+Mel,+AIA/DDC” vs “+Mel,−AIA/DDC”, Fig. 1 B) shows that a Mel-induced decrease of 35% (p < 0.05) in PBG accumulation is apparent. Even in the absence of porphyrinogenic drugs, Mel treatment resulted in a decrease of 36% (p < 0.05) in PBG levels, shown by comparing the groups “−Mel,−AIA/DDC” and “+Mel,−AIA/DDC” (Fig. 1 B).
|
|
|
Fig. 1. Levels of the heme pathway metabolites ALA (A) and PBG (B) in urine: effect of melatonin pre-treatment on AIA/DDC-induced porphyrinogenesis. ALA and PBG levels were determined in liver extracts from animals belonging to four different groups: −Mel−AIA/DDC, not pretreated with Mel nor treated with AIA/DDC; −Mel+AIA/DDC, not pretreated with Mel and treated with AIA/DDC; +Mel −AIA/DDC, pretreated with Mel but not treated with AIA/DDC; and +Mel + AIA/DDC, pretreated with Mel and then treated with AIA/DDC. Results are expressed as means ± SEM (n = 6 for each group). Urinary ALA content value of “−Mel−AIA/DDC” group: 6 μg ALA/16 h; urinary PBG content value of “−Mel−AIA/DDC”group: 1.93 mg/16 h. Statistically significant differences between groups (p<0.05) are indicated by asterisks above horizontal lines showing the group comparisons, as follows: “−Mel,+AIA/DDC” compared with “−Mel,−AIA/DDC”, for both ALA and PBG; “+Mel,+AIA/DDC” compared with “+Mel,−AIA/DDC”, for both ALA and PBG; “+Mel,+AIA/DDC” compared with “−Mel,+AIA/DDC”, for both ALA and PBG; “+Mel,−AIA/DDC” compared with “−Mel,−AIA/DDC”, for PBG
|
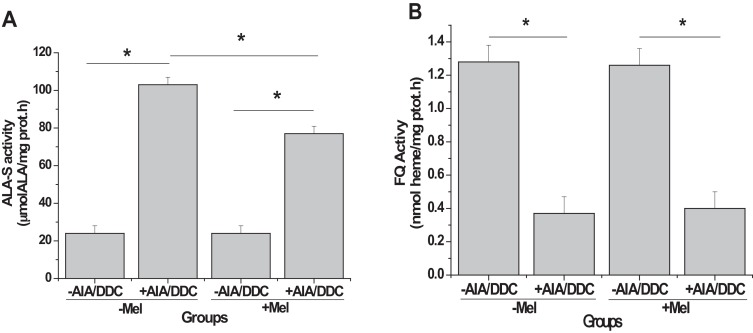
The activity of the heme pathway enzyme ALA-S was enhanced by 326% (p<0.05) as a result of the porphyrinogenic treatment (“−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 2 A). When animals were pre-treated with Mel before administration of AIA/DDC, ALA-S activity increased much less, by 220% (p < 0.05) (“+Mel,+AIA/DDC” vs “+Mel,−AIA/DDC”, Fig. 2 A). In brief, Mel attenuated by 33% the drug-induced enhancement of ALA-S activity. Mel alone had no effect on the expression of ALA-S activity (“+Mel,−AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 2 A).
|
|
|
Fig. 2. Heme pathway enzyme activities: effect of melatonin pre-treatment on AIA/DDC-induced porphyrinogenesis. Activities of ALA-S (A) and FQ (B) were determined in liver extracts from animals belonging to the four different groups described in Section 2.2 and Fig. 1 . Results are expressed as means ± SEM (n = 6 for each group). Hepatic ALA-S activity value of “−Mel−AIA/DDC” group: 24 μmol ALA/mg prot; hepatic FQ activity value of “−Mel−AIA/DDC” group: 1.28 nmol piridin.hemocromogen/mg prot.h. Statistically significant differences between groups (p < 0.05) are indicated by asterisks above horizontal lines showing the group comparisons, as follows: “−Mel,+AIA/DDC” compared with “−Mel,−AIA/DDC”, for ALA-S and FQ; “+Mel,+AIA/DDC” compared with “−Mel,+AIA/DDC”, for ALA-S; “+Mel,+AIA/DDC” compared with “+Mel,−AIA/DDC”, for ALA-S and FQ.
|
Because FQ is the last enzyme of the heme pathway, decreases in its activity will favor porphyria, inversely to ALA-S. As expected, FQ activity was decreased by 71% (p < 0.05) as a result of AIA/DDC treatment (“−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 2 B). This reduction was essentially the same when animals were pre-treated with Mel, as shown by comparing the decrease of “+Mel,+AIA/DDC” vs “+Mel,−AIA/DDC” with that of “−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC” (Fig. 2 B). Mel alone did not affect FQ activity (“+Mel,−AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 2 B).
3.2. Gluconeogenesis parameters
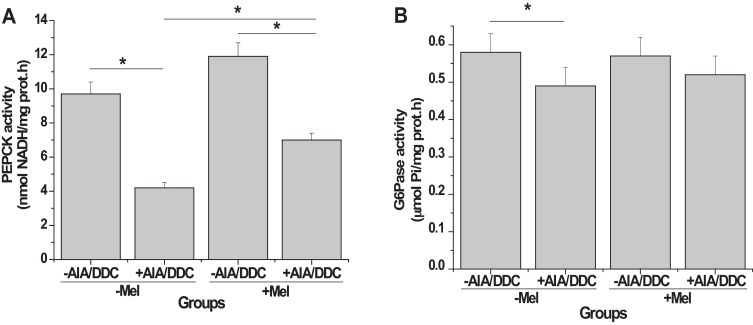
Since glucose is known to be beneficial to acute porphyrias, we determined the hepatic activity of the gluconeogenic enzymes PEPCK and G6Pase in the four groups studied (Fig. 3 ). Porphyrinogenic treatment resulted in a 55% decrease (p < 0.05) in PEPCK activity, as can be seen comparing “−Mel,+AIA/DDC” with “−Mel,−AIA/DDC” (Fig. 3 A). Administration of Mel before AIA/DDC reverted by 45% (p < 0.05) this porphyrinogenic drug-induced decrease in PEPCK, as shown by comparing the difference between “+Mel,+AIA/DDC” and “−Mel,+AIA/DDC” with the decrease “−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC” (Fig. 3 A). G6Pase activity was 15% lower (p < 0.05) in porphyric animals (“−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 3 B), and Mel pre-treatment abolished the difference between AIA/DDC-treated and untreated rats (“+Mel,+AIA/DDC” vs “+Mel,−AIA/DDC”, Fig. 3 B). The administration of Mel alone did not alter the activity of either PEPCK or G6Pase in a statistically significant way (“+Mel,−AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 3 A and B).
|
|
|
Fig. 3. Gluconeogenic enzyme activities: Effect of melatonin pre-treatment on AIA/DDC induced porphyrinogenesis. Activities of PEPCK (A) and G6Pase (B) were determined in liver extracts from animals belonging to the four different groups described in Section 2.2 and Fig. 1 . Results are expressed as means ± SEM (n = 6 for each group). Hepatic PEPCK activity value of “-Mel-AIA/DDC” group: 9.7 nmoles NADH consumed/mg prot.min; hepatic G6Pase activity value of “−Mel−AIA/DDC” group: 0.574 μmoles Pi/mg prot.min. Statistically significant differences between groups (p < 0.05) are indicated by asterisks above horizontal lines showing the group comparisons, as follows: “−Mel,+AIA/DDC” compared with “−Mel,−AIA/DDC”, for PEPCK and G6Pase; “+Mel,+AIA/DDC” compared with “−Mel,+AIA/DDC”, for PEPCK; “+Mel,+AIA/DDC” compared with “+Mel,−AIA/DDC”, for PEPCK.
|
3.3. Oxidative stress
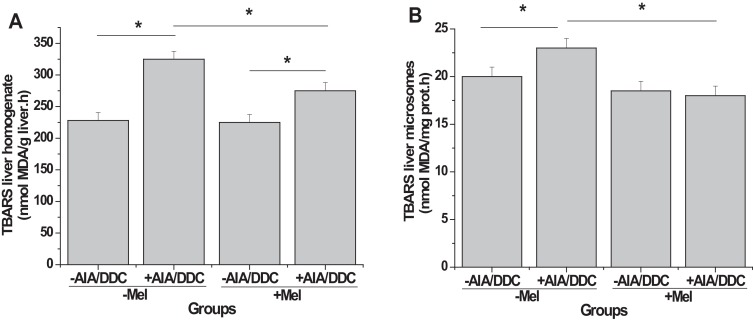
The development of AIA/DDC-induced oxidative stress was followed by determining TBARS levels in homogenates (Fig. 4 A) and microsomes (Fig. 4 B) from livers, in the four different animal groups. Porphyric rats showed increases in TBARS both in homogenates (45%, p < 0.05) and microsomes (21% p < 0.05), as shown by the comparison “−Mel,+AIA/DDC” with “−Mel,−AIA/DDC” (Fig. 4 A). Pre-treatment with Mel resulted in a considerably smaller increase in TBARS (24% p < 0.05) in liver homogenates, apparent when comparing “−Mel,+AIA/DDC” with “+Mel,+AIA/DDC” (Fig. 4 A). The increase in TBARS generation due to AIA/DDC in the absence of Mel (“−Mel,+AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 4 A) was reduced by 47% in its presence (“+Mel,+AIA/DDC” vs “+Mel,−AIA/DDC”, Fig. 4 A). In microsomes, pre-treatment with Mel abolished the 21% increase (p < 0.05) in TBARS induced by AIA/DDC without Mel (compare “−Mel,+AIA/DDC” vs “−Mel,+AIA/DDC” with “+Mel,−AIA/DDC” vs “+Mel,+AIA/DDC”, Fig. 4 B). Mel alone did not affect lipid peroxidation in either homogenates or microsomes (“+Mel,−AIA/DDC” vs “−Mel,−AIA/DDC”, Fig. 4 A and B).
|
|
|
Fig. 4. Oxidative stress: effect of melatonin pre-treatment on AIA/DDC-induced porphyrinogenesis. As markers of lipid peroxidation, levels of thiobarbituric acid reactive substances (TBARS) were determined in liver homogenates (A) and microsomal fractions (B) of animals belonging to the four different groups described in Section 2.2 and Fig. 1 . Results are expressed as means ± SEM (n = 6 for each group). Hepatic TBARS homogenate value of “−Mel−AIA/DDC” group: 228 nmoles MDA/g liver.h; hepatic TBARS microsomes value of “−Mel−AIA/DDC” group: 20 nmoles MDA/mg prot.h. Statistically significant differences between groups (p < 0.05) are indicated by asterisks above horizontal lines showing the group comparisons, as follows: “−Mel,+AIA/DDC” compared with “−Mel,−AIA/DDC”, for both whole homogenates and microsomes; “+Mel,+AIA/DDC” compared with “−Mel,+AIA/DDC”, for both whole homogenates and microsomes; “+Mel,+AIA/DDC” compared with “+Mel,−AIA/DDC”, for whole homogenates.
|
4. Discussion
We report here that the administration of Mel prior to the intoxication of rats with AIA/DDC results in a clear beneficial effect on the hepatic alterations elicited by these porphyrinogenic drugs regarding heme pathway, glucose metabolism and lipid peroxidation.
The AIA/DDC-induced increase in peroxidation we are reporting, indicated by an increase in TBARS in both liver homogenates and microsomes, is in agreement with increases previously found in our laboratory concerning protein carbonyl content, urinary chemiluminiscence, antioxidant SOD responses [14] and 8-hydroxy-2′-deoxyguanosine levels in urine [6] . These results, all obtained using the same porphyrinogenic drugs and rat strain, confirm the existence of oxidative stress in this experimental model of acute porphyria. The mechanism involves an important drug-induced increase in ALA-S activity causing the accumulation of ALA, which in turn promotes an oxidative environment by enhancing ROS generation [6] . ROS are able to damage lipids, DNA and proteins. The fact that the extent of the drug-induced oxidative level is reduced as a consequence of pre-treatment of the animals with Mel is likely to be due to the antioxidant and free radical scavenging properties of this hormone. Mel has been reported to interact with highly toxic hydroxyl radicals and neutralize hydrogen peroxide, singlet oxygen, peroxynitrite anion, nitric oxide and hypochlorous acid [29] . In addition, interactions of Mel with ROS via oxidative pyrrole ring cleavage can generate further antioxidant compounds such as cyclic 3-hydroxymelatonin, N1-acetyl-N2-formyl-5-methoxyquinuramine (AFMK) and N1-acetyl-5-methoxyquinuramine (AMK) [29] and [30] . The process by which Mel and its metabolites scavenge ROS and RNS is considered to be a free radical scavenging cascade that magnifies the efficacy of Mel as an antioxidant [8] . The ability of Mel to attenuate lipid damage, here described, is in keeping with reports of Mel decreasing lipid peroxidation and the rigidity of microsomal membranes due to the oxidative stress caused by ALA [12] .
Aldehydes generated during lipid peroxidation can react with amino-acid side chains of proteins [4] , with the residues susceptible to oxidation being Arg, Lys, Thr, Cys and His [15] . Therefore, ROS generated during the porphyrinogenic treatment could damage protein structures and/or even oxidize enzyme active site residues. Thus, the activity of gluconeogenic enzymes such as PEPCK and G6Pase can be reduced by AIA/DDC treatment [14] , so favoring the development of acute porphyria. In fact, G6Pase is a nine-transmembrane domain protein with a catalytic center including Lys76 , Arg83 , His119 , Arg170 , and His176 on the luminal side of the ER membrane. His176 is involved in the formation of a phosphohistidine-enzyme intermediate during catalysis [9] and [10] . Pre-treatment with Mel had attenuating, beneficial effects regarding PEPCK and G6Pase activities.
Summarizing, the AIA/DDC-induced decrease in the activity of the gluconeogenic enzymes PEPCK and G6Pase results in a reduction in glucose synthesis. The latter de-represses the regulatory heme pathway enzyme ALA-S [33] , as shown in the present work and in agreement with our previous findings [14] and [20] . Pre-treatment with Mel partially reverts the AIA/DDC-induced decreases in PEPCK and G6Pase activities, therefore increasing glucose synthesis. As a consequence, ALA-S is repressed. The down-regulation of ALA-S was confirmed in the present work by the observed decrease in levels of the heme precursors ALA and PBG elicited by Mel pre-treatment. Being the last enzyme for heme synthesis, a lower FQ activity favors the accumulation of heme precursors. We observed a lower FQ activity in AIA/DDC-treated rats, probably due to oxidative reactions affecting SH groups [31] and an essential His residue seemingly involved in Fe+2 chelation [7] . The porphyrinogenic drug-induced decrease in FQ activity was not reversed by Mel pre-treatment.
The influence of Mel pre-treatment on the events described above point to a beneficial decrease in the severity of acute porphyria in the model here employed. This is in line with other beneficial effects reported for Mel in a broad number of different situations [17] . The results shown also suggest the possibility of using Mel as co-treatment for acute porphyria.
5. Conclusions
The present work shows that Mel treatment has a beneficial effect in experimental acute porphyria. We hypothesize that Mel could be scavenging ROS/RNS that peroxidize lipids and alter PEPCK and G6Pase activity. Mel would act by restoring glucose levels, therefore repressing ALA-S, with a consequential decrease in the levels of the heme precursors ALA and PBG which decreases the severity of porphyria. The results obtained open new research possibilities regarding the use of melatonin as a co-treatment option in acute porphyria.
Conflicts of interest
None.
Acknowledgements
We thank Dr. Rodolfo Garcia for the kind revision and language correction of the manuscript and Dr Sergio I. Nemirovsky (IQUIBICEN) for guidance on statistical analysis of the results. This work was supported by grants from The National Research Council of Argentina (CONICET) and The University of Buenos Aires . L.C. San Martín de Viale is a member of the Scientific Research Career of the CONICET.
References
- [1] B.N. Ayes; Assay of inorganic phosphate, total phosphate and phosphatases; E.F. Neufeld, V. Ginsburg (Eds.), Carbohydrate Metabolism, Part E: Methods in Enzymology, vol. VIII, Academic Press, New York (1966), pp. 115–118
- [2] E.S. Baginski, P.P. Foa, B. Zak; Glucose-6-phosphatase; H.U. Bermeyer (Ed.), Method of Enzymatic Analysis (2nd ed.), vol. 1, Verlag Chemie/Academic Press, New York (1974), pp. 876–880
- [3] S. Besur, W. Hou, P. Schmeltzer, H.L. Bonkovsky; Clinically important features of porphyrin and heme metabolism and the porphyrias; Metabolites, 4 (2014), pp. 977–1006 doi: 10.3390/metabo4040977; Review. PMID:25372274. [PubMed] PMCID: PMC4279155
- [4] I. Dalle-Donne, R. Rossi, D. Giustarini, A. Milzani, R. Colombo; Protein carbonyl groups as biomarkers of oxidative stress; Clin. Chim. Acta, 329 (2003), pp. 23–38 http://dx.doi.org/10.1016/S0009-8981(03)00003-2 PMID:12589963[PubMed—indexed for MEDLINE]
- [5] F. De Matteis, G. Abbritti, A.H. Gibbs; Decreased liver activity of porphyrin–metal chelatase in hepatic porphyria caused by 3,5-diethoxycarbonyl-1,4-dihydrocollidine. Studies in rats and mice; Biochem. J., 134 (1973), pp. 717–727 PMID:4749272[PubMed - indexed for MEDLINE] PMCID:PMC1177868
- [6] M. Faut, A. Paiz, L.C. San Martín de Viale, M.B. Mazzetti; Alterations of the redox state, pentose pathway and glutathione metabolism in an acute porphyria model. Their impact on heme pathway; Exp. Biol. Med. (Maywood), 238 (2013), pp. 133–143 http://dx.doi.org/10.1177/1535370212473702 Epub 2013 Feb 6. PMID:23390166
- [7] R. Franco, J.G. Ma, Y. Lu, G.C. Ferreira, J.A. Shelnutt; Porphyrin interactions with wild-type and mutant mouse ferrochelatase; Biochemistry, 39 (2000), pp. 2517–2529 http://dx.doi.org/10.1021/bi991346t PMID:10704201[PubMed—indexed for MEDLINE]
- [8] J.J. García, L. López-Pingarrón, P. Almeida-Souza, A. Tres, P. Escudero, F.A. García-Gil, D.X. Tan, R.J. Reiter, J.M. Ramírez, M. Bernal-Pérez; Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: a review; Pineal Res., 56 (2014), pp. 225–237 http://dx.doi.org/10.1111/jpi.12128 PMID:24571249 [PubMed—indexed for MEDLINE]
- [9] A. Ghosh, J.J. Shieh, C.J. Pan, M.S. Sun, J.Y. Chou; The catalytic center of glucose-6-phosphatase. HIS176 is the nucleophile forming the phosphohistidine-enzyme intermediate during catalysis; J. Biol. Chem., 277 (2002), pp. 32837–32842 http://dx.doi.org/10.1074/jbc.M201853200 PMID:12093795 [PubMed—indexed for MEDLINE]
- [10] A. Ghosh, J.J. Shieh, C.J. Pan, J.Y. Chou; Histidine 167 is the phosphate acceptor in glucose-6-phosphatase-beta forming a phosphohistidine enzyme intermediate during catalysis; J. Biol. Chem., 279 (2004), pp. 12479–12483 http://dx.doi.org/10.1074/jbc.M313271200 PMID:14718531 [PubMed - indexed for MEDLINE]
- [11] M. Karbownik, D. Tan, L.C. Manchester, R.J. Reiter; Renal toxicity of the carcinogen delta-aminolevulinic acid: antioxidant effects of melatonin; Cancer Lett., 161 (2000), pp. 1–7 http://dx.doi.org/10.1016/S0304-3835(00)00568-1PMID:11078907 [PubMed - indexed for MEDLINE]
- [12] M. Karbownik, R.J. Reiter, J.J. Garcia, D.X. Tan, W. Qi, L.C. Manchester; Melatonin reduces rat hepatic macromolecular damage due to oxidative stress caused by delta-aminolevulinic acid; Biochim. Biophys. Acta, 1523 (2000), pp. 140–146 http://dx.doi.org/10.1016/S0304-4165(00)00110-0 PMID:11042377 [PubMed—indexed for MEDLINE]
- [13] M. Karbownik, A. Lewinski, R.J. Reiter; Anticarcinogenic actions of melatonin which involve antioxidative processes: comparison with other antioxidants; Int. J. Biochem. Cell Biol., 33 (2001), pp. 735–753 Review. 10.1016/S1357-2725(01)00059-0; PMID: 11404179 [PubMed - indexed for MEDLINE]
- [14] S.M. Lelli, L.C. San Martin de Viale, M.B. Mazzetti; Response of glucose metabolism enzymes in an acute porphyria model. Role of reactive oxygen species; Toxicology, 216 (2005), pp. 49–58 http://dx.doi.org/10.1016/j.tox.2005.07.016 PMID:16125296 [PubMed—indexed for MEDLINE
- [15] R.L. Levine, J.A. Williams, E.R. Stadtman, E. Shacter; Carbonyl assays for determination of oxidatively modified proteins; L. Packer (Ed.), Oxygen Radicals in Biological Systems. Methods in Enzymology, vol. 233, Academic Press, San Diego (1994), pp. 346–357
- [16] O. Lowry, N. Rosebrough, A. Farr, R. Randall; Protein measurement with the folin-phenol reagent; J. Biol. Chem., 193 (1951), pp. 265–275 PMID:14907713[PubMed—indexed for MEDLINE]
- [17] A. Masters, S.R. Pandi-Perumal, A. Seixas, J.L. Girardin, S.I. McFarlane; Melatonin, the hormone of darkness: from sleep promotion to Ebola treatment; Brain Disord. Ther. (2014) 4. pii: 1000151. 10.4172/2168-975X.1000151; PMID:25705578 [PubMed] PMCID: PMC4334454
- [18] G.S. Marks, S.A. McCluskey, J.E. Mackie, D.S. Riddick, C.A. James; Disruption of hepatic heme biosynthesis after interaction of xenobiotics with cytochrome P-450; FASEB J., 2 (1988), pp. 2774–2783 0892-6638/88/0002-2774; PMID:3044903 [PubMed-indexed for MEDLINE]
- [19] H.S. Marver, D.P. Tschudy, M.G. Perlroth, A. Collins; Delta-aminolevulinic acid synthetase. I. Studies in liver homogenates; J. Biol. Chem., 241 (1966), pp. 2803–2889 PMID: 4957991 [PubMed—indexed for MEDLINE]
- [20] L.B. Matkovic, F. D’Andrea, D. Fornes, L.C. San Martín de Viale, M.B. Mazzetti; How porphyrinogenic drugs modeling acute porphyria impair the hormonal status that regulates glucose metabolism. Their relevance in the onset of this disease; Toxicology, 290 (2011), pp. 22–30 doi: 10.1016/j.tox.2011.08.014 ; PMID:21889565PubMed—indexed for MEDLINE]
- [21] D. Mauzerall, S. Granick; The occurrence and determination of delta-amino-levulinic acid and porphobilinogen in urine; J. Biol. Chem., 219 (1956), pp. 435–446 PMID:13295297[PubMed—indexed for MEDLINE]
- [22] M.B. Mazzetti, M.C. Taira, S.M. Lelli, E. Dascal, J.C. Basabe, L.C. San Martín de Viale; Hexachlorobenzene impairs glucose metabolism in a rat model of porphyria cutaneatarda: a mechanistic approach; Arch. Toxicol, 78 (2004), pp. 25–33 http://dx.doi.org/10.1007/s00204-003-0470-y PMID:12898129 [PubMed—indexed for MEDLINE]
- [23] H. Ohkawa, N. Ohishi, K. Yagi; Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction; Anal. Biochem., 95 (1979) 351–358. PMID:36810 [PubMed—indexed for MEDLINE]
- [24] I. Petrescu, O. Bojan, M. Saied, O. Barzu, F. Schmidt, H.F. Kuhnle; Determination of phosphoenolpyruvate carboxykinase activity with deoxyguanosine 5′-diphosphate as nucleotide substrate; Anal. Biochem., 96 (1979), pp. 279–281 PMID:474956[PubMed - indexed for MEDLINE]
- [25] W.N. Piper, L.W. Condie, T.R. Tephly; The role of substrates for glycine acyltransferase in the reversal of chemically induced porphyria in the rat; Arch. Biochem. Biophys., 159 (1973), pp. 671–677 http://dx.doi.org/10.1016/0003-9861(73)90506-7 Science direct
- [26] R.J. Porra, O.T. Jones; Studies on ferrochelatase. I. Assay and properties of ferrochelatase from a pig-liver mitochondrial extract; Biochem. J., 87 (1963), pp. 181–185 PMID: 13972328 [PubMed - indexed for MEDLINE] PMCID: PMC1276858
- [27] R.J. Reiter, D.X. Tan, C. Osuna, E. Gitto; Actions of melatonin in the reduction of oxidative stress. A review; J. Biomed. Sci., 7 (2000), pp. 444–458 PMID:11060493[PubMed—indexed for MEDLINE
- [28] R.J. Reiter, D.X. Tan, M.D. Maldonado; Melatonin as an antioxidant: physiology versus pharmacology; J. Pineal Res., 39 (2005), pp. 215–216 http://dx.doi.org/10.1111/j.1600-079X.2005.00261.x PMID:16098101 [PubMed—indexed for MEDLINE]
- [29] R.J. Reiter, D.X. Tan, A. Galano; Melatonin reduces lipid peroxidation and membrane viscosity; Front. Physiol., 5 (2014), p. 377 http://dx.doi.org/10.3389/fphys.2014.00377 PMID:25339906 [PubMed] PMCID: PMC4186275
- [30] A.R. Ressmeyer, J.C. Mayo, V. Zelosko, R.M. Sáinz, D.X. Tan, B. Poeggeler, et al.; Antioxidant properties of the melatonin metabolite N1-acetyl-5-methoxykynuramine (AMK): scavenging of free radicals and prevention of protein destruction; Redox Rep., 8 (2003), pp. 205–213 http://dx.doi.org/10.1179/135100003225002709; PMID:14599344 [PubMed - indexed for MEDLINE]
- [31] V.M. Sellers, M.K. Johnson, H.A. Dailey; Function of the [2FE-2S] cluster in mammalian ferrochelatase: a possible role as a nitric oxide sensor; Biochemistry, 35 (1996), pp. 2699–2704 http://dx.doi.org/10.1021/bi952631p PMID:8611576 [PubMed—indexed for MEDLINE]
- [32] D.X. Tan, R.J. Reiter, L.C. Manchester, M.T. Yan, M. El-Sawi, R.M. Sainz, et al.; Chemical and physical properties and potential mechanisms: melatonin as a broad hspectrum antioxidant and free radical scavenger; Curr. Top. Med. Chem., 2 (2002), pp. 181–197 http://dx.doi.org/10.2174/1568026023394443 PMID:11899100 [PubMed—indexed for MEDLINE]
- [33] D.P. Tschudy, F.H. Welland, A. Collins, G. Hunter Jr.; The effect of carbohydrate feeding on the induction of delta-aminolevulinic acid synthetase; Metabolism, 13 (1964), pp. 396–406 PMID:14169218 [PubMed—indexed for MEDLINE]
Document information
Published on 02/05/17
Accepted on 02/05/17
Submitted on 02/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?