Summary
A Dieulafoy lesion is an uncommon and sometimes life-threatening cause of gastrointestinal hemorrhage. Typically, it presents as a tiny mucosal defect with an exposed protruding artery with normal surrounding mucosa. An 84-year-old woman developed sudden massive hematochezia and had an unstable hemodynamic status. The source of bleeding was found to be an exposed vessel in the rectum without surrounding ulceration. The patient was treated successfully with an epinephrine injection given endoscopically, followed by hemostatic clipping.
Keywords
Colonoscopy ; Dieulafoy lesion ; Hematochezia ; Hemostasis ; Rectum
Introduction
The etiology of acute massive gastrointestinal hemorrhage can be identified in 80–95% of patients after performing a flexible fiber-optic endoscopic examination [1] . Dieulafoy lesions are rare but potentially life threatening, and account for 1–2% of cases of acute gastrointestinal bleeding. The lesion was initially described by Gallard in 1884, and was then further defined and characterized by a French surgeon named Paul Georges Dieulafoy in 1898 [2] . Dieulafoy lesions usually occur in the proximal stomach, especially in the lesser curvature within 6 cm of the gastroesophageal junction [3] . Bleeding from a Dieulafoy lesion is not specific to a particular age group, but is more commonly reported in elderly men.
Currently, endoscopy is the first choice of treatment for these lesions [4] ; [5] ; [6] ; [7] ; [8] . Only a few cases of Dieulafoy lesions in the rectum have been reported in the literature. Here we report the case of an elderly woman with acute profuse lower gastrointestinal hemorrhage from a rectal Dieulafoy lesion. The patient was successfully treated endoscopically.
Case report
An 84-year-old woman had congestive heart failure associated with hypertension, atrial fibrillation, and valvular heart disease. She was admitted after experiencing profuse hematochezia for 3 days. On admission, her blood pressure was 88/60 mmHg, and her pulse rate was 100 beats/min. Biologic testing revealed marked anemia (hemoglobin, 7.4 g/dL), mild hypokalemia (potassium, 3 mEq/L), mild hyponatremia (sodium, 133 mEq/L), renal function abnormalities (creatinine, 1.3 mg/dL; blood urea, 42 mg/dL), and hypoalbuminemia (albumin, 2.3 g/dL). After resuscitation and a blood transfusion, urgent colonoscopy without full-bowel preparation was performed. The colonoscope was advanced through the rectum only to the level of the sigmoid colon because of the poor bowel visualization caused by a large amount of fresh blood and blood clots. Based on the first colonoscopic examination findings, the bleeding was suspected to originate from the small bowel or colon.
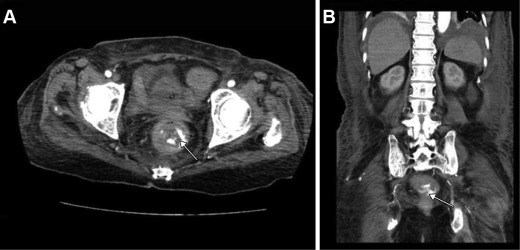
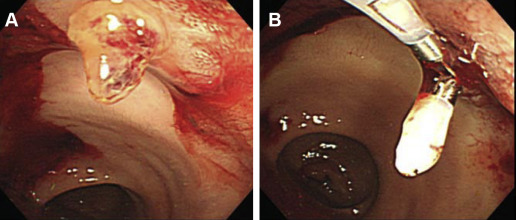
Three days later, computed tomography angiography (CTA) was performed after the patient had another episode of massive gastrointestinal bleeding. Contrast extravasation from the rectal wall was identified on CTA scans (Fig. 1 ). In addition, a small amount of ascites was demonstrated within the subphrenic space, which suggested possible congestive heart failure and hypoalbuminemia. After discussing the possible treatment options with a radiologist, we chose to repeat endoscopic examination first. A bilateral iliac angiography with subsequent embolization for rectal bleeding would be performed if the therapeutic endoscopic examination failed. Repeat colonoscopy again revealed a protruding vessel oozing blood 5 cm from the proximal end to the anal verge. The surrounding mucosa of the vessel appeared normal, without ulceration or erosion, which was consistent with a Dieulafoy lesion (Fig. 2 A). Hemostasis was achieved by administering an endoscopic epinephrine injection, followed by application of two hemoclips (Fig. 2 B). The patient was discharged in a stable condition 1 week later.
|
|
|
Figure 1. Results from computed tomography angiography (CTA) of an 84-year-old woman with massive bleeding. (A) Axial and (B) coronal CTA images reveal contrast extravasation from the rectal wall (arrow). |
|
|
|
Figure 2. Colonoscopic findings in our elderly patient. (A) Urgent colonoscopy revealed a protruding vessel in the lower rectum with normal surrounding mucosa, consistent with a Dieulafoy lesion. (B) The lesion was treated endoscopically with epinephrine injection and placement of two hemoclips. |
Discussion
Although rectal Dieulafoy lesions are extremely rare, they should be considered in the differential diagnosis of massive lower gastrointestinal bleeding, and, as shown in this case, these lesions are particularly suitable for endoscopic therapy.
Lower gastrointestinal bleeding originates from the small bowel or colon. It usually presents with hematochezia and occasionally with melena. Colonoscopy is considered the procedure of choice for the initial evaluation and treatment of acute lower gastrointestinal bleeding. However, if the condition of a patient with massive bleeding cannot be stabilized and colonoscopy is impossible, or when the source of bleeding cannot be identified by endoscopic examination, mesenteric angiography with or without preceding radionuclide scanning or CTA is also an appropriate choice.
A Dieulafoy lesion is a rare but well-recognized cause of gastrointestinal bleeding. It consists of a large-caliber submucosal artery protruding through a tiny mucosal defect into the bowel lumen, which induces intermittent massive gastrointestinal bleeding. Although it most often occurs in the proximal stomach [3] , it has also been reported in the esophagus, small intestine, colon, and rectum.
The diagnosis depends on the following endoscopic criteria [9] : (1) active arterial spurting or micropulsatile streaming from a minute (<3 mm) mucosal defect or through the normal surrounding mucosa; (2) visualization of a protruding vessel with or without active bleeding from a minute mucosal defect or through the normal-appearing mucosa; and (3) the appearance of a fresh, densely adherent clot with a narrow point of attachment to a minute mucosal defect or the normal-appearing mucosa. The absence of macroscopic surrounding inflammatory tissue is important for the endoscopic diagnosis. Our patient had a vessel protruding through the normal-appearing rectal mucosa.
Making an endoscopic diagnosis of rectal Dieulafoy lesions is more challenging because of the small size of the lesion and the presence of many blood clots and stool in the rectum. Therefore, repeated endoscopic evaluations with careful inspection of rectal mucosa are sometimes necessary to make the correct diagnosis [6] ; [7] . In our elderly patient, we could not detect the origin of bleeding during the first colonoscopy because of the presence of fresh blood and blood clots in the colon and rectum. During another episode of massive bleeding, CTA scans showed the approximate location of the bleeding site, and with repeated endoscopic examination we were able to detect a rectal Dieulafoy lesion.
Bleeding from a Dieulafoy lesion often does not respond to conservative treatment alone. A number of endoscopic hemostasis techniques have been reported to be effective for treating Dieulafoy lesions. Endoscopic epinephrine injection followed by heater probe thermal coagulation, bipolar probe coagulation, or hemoclipping are effective ways to control active bleeding. Endoscopic band ligation of the exposed vessel has also been used to treat Dieulafoy lesions successfully [4] ; [5] ; [6] ; [7] ; [8] . Surgical resection or arterial embolization is performed for patients with intractable bleeding or in those in whom endoscopic therapy has failed [3] ; [9] ; [10] . In our case, the rectal Dieulafoy lesion was treated successfully by epinephrine injection followed by hemostatic clipping.
In summary, although rectal Dieulafoy lesion is an uncommon cause of lower gastrointestinal bleeding, the possibility must be kept in mind when profuse rectal bleeding is encountered. Our case confirms the safety and effectiveness of endoscopic therapy for rectal Dieulafoy lesions.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] K.S. Lee, Y.J. Moon, S.I. Lee, I.S. Park, S.K. Sohn, J.S. Yu, et al.; A case of bleeding from the Dieulafoy lesion of the jejunum; Yonsei Med J, 38 (1997), pp. 240–244
- [2] E. Franko, R. Chardavoyne, L. Wise; Massive rectal bleeding from a Dieulafoy’s type ulcer of the rectum: a review of this unusual disease; Am J Gastroenterol, 86 (1991), pp. 1545–1547
- [3] S.J. Veldhuyzen van Zanten, J.F. Bartelsman, M.E. Schipper, G.N. Tytgat; Recurrent massive haematemesis from Dieulafoy vascular malformations—a review of 101 cases; Gut, 27 (1986), pp. 213–222
- [4] H.H. Kim, J.H. Kim, S.E. Kim, S.J. Park, M.I. Park, W. Moon; Rectal dieulafoy lesion managed by hemostatic clips; J Clin Med Res, 4 (2012), pp. 439–441
- [5] W. Apiratpracha, J.K. Ho, J.J. Powell, E.M. Yoshida; Acute lower gastrointestinal bleeding from a dieulafoy lesion proximal to the anorectal junction post-orthotopic liver transplant; World J Gastroenterol, 12 (2006), pp. 7547–7548
- [6] A. Hokama, Y. Takeshima, A. Toyoda, Y. Yonamine, R. Tomiyama, F. Kinjo, et al.; Images of interest. Gastrointestinal: rectal Dieulafoy lesion; J Gastroenterol Hepatol, 20 (2005), p. 1303
- [7] S. Nomura, M. Kawahara, K. Yamasaki, Y. Nakanishi, M. Kaminishi; Massive rectal bleeding from a Dieulafoy lesion in the rectum: successful endoscopic clipping; Endoscopy, 34 (2002), p. 237
- [8] G. Casella, G. Bonforte, R. Corso, C.A. Buda, G. Corti, A.R. Cambareri, et al.; Rectal bleeding by Dieulafoy-like lesion: successful endoscopic treatment; G Chir, 26 (2005), pp. 415–418
- [9] M.E. Stark, C.J. Gostout, R.K. Balm; Clinical features and endoscopic management of Dieulafoy’s disease; Gastrointest Endosc, 38 (1992), pp. 545–550
- [10] M. Kim, H.J. Song, S. Kim, Y.K. Cho, H.U. Kim, B.C. Song, et al.; Massive life-threatening lower gastrointestinal hemorrhage caused by an internal hemorrhoid in a patient receiving antiplatelet therapy: a case report; Korean J Gastroenterol, 60 (2012), pp. 253–257
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?