Summary
A mesenteric cyst is defined as a cyst that is located in the mesentery of the gastrointestinal tract and may extend from the base of the mesentery into the retroperitoneum. A case report of a patient with mesenteric cyst is presented. In addition, a systematic review was performed of English language literature on chylous mesenteric cysts in adult humans. Of the 18 articles included in the review, there were 19 cases of chylous mesenteric cysts reported. Male to female ratio was 1.4:1 with a median age of 46 years. A preoperative diagnosis of mesenteric cyst was made in four patients based on computed tomography. All patients underwent surgery and there were no reports of recurrence on follow up. Chylous mesenteric cyst is a rare entity that needs to be recognized whenever a preliminary diagnosis of intra-abdominal cystic mass is made.
Keywords
adult;chylous;cyst;laparoscopy;mesenteric
1. Introduction
Mesenteric cysts are identified in about 1 of 100,000 adult hospital admissions.1; 2; 3 ; 4 Mesenteric cysts can occur anywhere in the mesentery of the gastrointestinal tract from the duodenum to the rectum. They may extend from the base of the mesentery into the retroperitoneum.5 ; 6 In a series of 162 patients, 60% of mesenteric cysts occurred in the small-bowel mesentery, 24% in the large-bowel mesentery, and 14.5% in the retroperitoneum.2
Chylous mesenteric cysts have an estimated incidence of 7.3% of all abdominal cysts.7 Only 50 cases had been reported up to 1987.8 It was first described by von Rokitansky in 1842.9
Patients generally present with abdominal distention associated with vague abdominal pain with or without a palpable mass.10 ; 11 The mass may be huge, simulating ascites.12 These cysts can be detected during laparotomy or laparoscopy.13 Although often asymptomatic, 10% of patients with such cysts present as an acute abdomen.13 The mainstay of therapy is the complete surgical removal of the cyst.
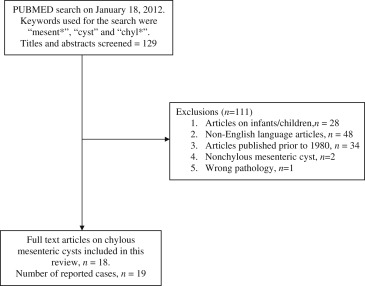
Following management of a patient with a mesenteric cyst (see ‘Case report’ section), a literature search of the Medline database via the PubMed interface was performed on January 18, 2012 using the terms ‘mesent∗’, ‘chyl∗’ and ‘cyst’ as keywords. The titles and abstracts of the retrieved searches were screened to include all original articles that described chylous mesenteric cysts in humans. Articles that did not have an English translation, articles on infants and/or children, and articles published prior to 1980 were excluded. Articles that did not report on the chylous content of the mesenteric cyst were also excluded. All full text articles of the eligible manuscripts were reviewed.
The data were extracted in a standardized manner and exported to an Excel spreadsheet. This included details of the study population, presentation, imaging, management, findings at surgery, and outcomes. Fig. 1 illustrates the process of inclusion and exclusion of articles identified by the search.
|
|
|
Figure 1. The process of inclusion and exclusion of articles identified by the search. |
2. Case report
A nulliparous 34-year-old lady initially presented to the gynecologists with abdominal distension, discomfort, and a feeling of “lump in the abdomen” of 2 months' duration. She did not report any episodes of acute pain, altered bowel habits, or menstrual irregularities. She had no comorbid illnesses. A mass in the suprapubic region could be palpated. Transabdominal and transvaginal ultrasound scans showed a 10 cm × 10 cm lesion suggestive of a left ovarian cyst. The cancer antigen 125 level was normal.
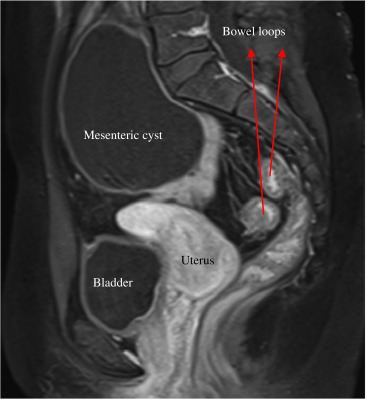
An initial laparoscopy with the intention to perform an ovarian cystectomy was terminated as a large cyst was found to arise from the small bowel mesentery, prolapsing into the pelvis. The pelvic organs were normal. Further imaging (magnetic resonance imaging) demonstrated an 11 cm cystic mass arising from the small bowel mesentery just below the bifurcation of the aorta (Fig. 2). It had the appearances of a benign lesion (thin walled, homogenous cyst with no solid components).
|
|
|
Figure 2. Sagittal view of the abdomen and pelvis on magnetic resonance imaging. The mesenteric cyst is shown lying in front of the sacral promontory and above the uterus. |
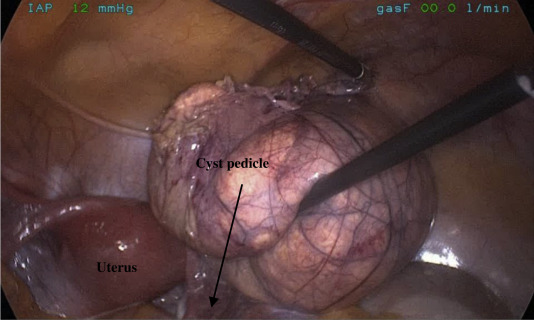
A laparoscopic excision of mesenteric cyst was performed. Intraoperatively, the cyst was noted to arise from the base of the jejunal mesentery (Fig. 3). Decompression of the cyst showed chylous fluid. The procedure was uneventful, the patient recovered, and she was discharged on the second postoperative day.
|
|
|
Figure 3. Intraoperative view showing normal uterus. A pedicled mesenteric cyst that enabled complete excision without bowel resection. |
Histological examination showed features of a unilocular cyst comprised a single layer of flattened mesothelial cells lining a fibrous wall that contained clusters of lymphocytes and cholesterol crystals. There was no evidence of malignancy. Biochemical examination could not be performed as the contents had become viscous on standing. Microbiological assessment showed no growth.
3. Discussion
The diagnosis of mesenteric cysts pose a challenge as these may mimic pathologies such as pancreatic pseudocysts, cystic tumors, pelvic diseases, and aortic aneurysms.14; 15 ; 16Malignant changes occur in less than 3% of cases.17
Chylous cyst is to be differentiated from other fluid-filled abdominal cystic masses such as mesenteric, omental, and dermoid cysts.8; 18 ; 19 This is because lymph fluid is normally found in the mesentery of the small bowel and the thoracic duct.7 True chylous cyst originates from the mesentery of the small bowel whereas false chylous cyst occurs from nonlymphatic sources or regional lymphatics.7 Chylous cysts are often congenital but may be related to previous abdominal surgery, pelvic diseases, and trauma.1; 2; 3; 4; 20 ; 21 The etiology of chylous mesenteric cyst remains unclear.
3.1. Presentation
The findings of the systematic review have been presented here. Nineteen cases presented in 18 reports were included. The median age of presentation of patients with chylous mesenteric cysts was 46 years (range, 20–74 years). The male to female ratio was 1.4:1.0. Table 1 shows the presenting symptoms and signs. Uncommon scenarios included a young patient with coexisting acute Crohns disease and one elderly patient with abdominal aortic aneurysm. Table 2 displays the characteristics of patients with chylous mesenteric cysts featured in the systematic review.8; 14; 15; 16; 22; 23; 24; 25; 26; 27; 28; 29; 30; 31; 32; 33; 34 ; 35
| Presenting symptom | Patients affected (n) |
|---|---|
| Abdominal pain | 13 |
| Abdominal distension | 7 |
| Nausea and vomiting | 6 |
| Progressively increasing abdominal mass | 3 |
| Loss of weight | 2 |
| Postprandial pain | 1 |
| Constipation | 1 |
| Early satiety | 1 |
| Syncope | 1 |
| Ref | Sex | Age (y) | Presentation | Imaging | Preoperative diagnosis | Management | Comments |
|---|---|---|---|---|---|---|---|
| 22 | M | 64 | 3-d history of epigastric pain, nausea and vomiting | Upper GI series, US, CT | Exophytic pancreatic pseudocyst/chylous mass | Drainage of cyst | — |
| 23 | F | 31 | Abdominal distension and early satiety | Upper GI series, CT | Mesenteric cyst | Enucleation of cyst | — |
| 24 | M | 45 | Abdominal distension | CT | Mesenteric cyst | Excision of cyst | — |
| 25 | F | 22 | Abdominal distension | US | Ovarian cyst | Excision of cyst | — |
| 8 | M | 27 | Left lower quadrant pain and weight loss | Barium enema, CT | Exacerbation of Crohns disease | Excision of cyst and bowel resection for Crohns disease | Associated with Crohns disease |
| 26 | M | 48 | Epigastrium pain radiating to the back | US, CT, angiography | Pancreatic/mesenteric cyst | Surgery (details not clear) | — |
| 26 | F | 46 | Pain in the right flank with microscopic hematuria | IVP, CT, angiography | Renal / mesenteric cyst | Surgery (details not clear) | — |
| 27 | M | 40 | Lower abdominal pain, | US, CT | Mesenteric cyst | Excision of cyst | — |
| 4.5 kg weight loss | |||||||
| 28 | M | 20 | 6-mo history of severe post prandial pain | CT, barium enema | — | Enucleation of cyst | Initially investigated and treated for peptic ulcer disease |
| 29 | F | 35 | Acute abdomen | Skiagram | Acute intestinal obstruction | Excision of cyst | Conservative management for similar attack previously; multiple cysts at surgery |
| 30 | F | 26 | Incidental finding at laparotomy for sterilization | — | — | Excision of cyst | — |
| 31 | F | 59 | Low grade fever and lower abdominal pain | Barium enema, US, CT | Mesenteric cyst | Enucleation of cyst | |
| 14 | M | 66 | Incidental finding on routine US abdomen | CT, EUS, ERCP, MRCP | Pancreatic cystadenoma / cystadenocarcinoma | Enucleation of cyst | — |
| 16 | M | 74 | Acute abdomen | CT | Contained rupture of abdominal aortic aneurysm | Chyloma deroofed and drained | — |
| 32 | F | 27 | Right lower abdominal pain, nausea | US, CT | Adnexal torsion | Excision of cyst | — |
| 33 | M | 67 | Abdominal fullness | Upper GI series, enteroscopy | Pedunculated polyp in the proximal jejunum | Endoscopic resection with snare cautery polypectomy | — |
| 15 | F | 62 | Pelvic and abdominal pain, fullness | US, CT | Ovarian mass | Excision of cyst with small bowel resection | — |
| 34 | M | 62 | Acute abdomen | AXR, CT | Acute pancreatitis with non-specific intra-abdominal cystic mass | Partial excision of cyst | Conservative management for 48 h |
| 35 | M | 58 | Chronic abdominal in the right lower quadrant. | US, CT, MRI | — | Laparoscopic excision | — |
AXR = abdominal x-ray; CT = computed tomography; ERCP = endoscopic retrograde cholangiopancreatography; EUS = endoscopic ultrasound; F = female; IVP = intravenous pyelography; M = male; MRCP = magnetic resonance cholangiopancreatography; MRI = magnetic resonance imaging; Upper GI = upper gastrointestinal; US = ultrasound.
3.2. Imaging
Most patients had some form of imaging done preoperatively. The initial workup depended on which medical speciality the patients first presented to. Abdominal computed tomography (CT; n = 15) was the most frequent mode of imaging performed, followed by ultrasonography (n = 9). A preoperative diagnosis of mesenteric cyst was made in 4 patients based on CT.
Ultrasound is often used in the initial evaluation of a suspected abdominal mass and may show a fluid filled cystic structure. This can often be confused with large ovarian cysts, as with the case described above. CT or magnetic resonance imaging may provide additional information on the origin of the cyst and the relationship of the lesion to visceral organs and vessels. This aids in planning the surgical approach, especially if minimally invasive surgery is considered.
3.3. Management
Surgical management of the mesenteric cysts included excision of cysts (n = 7), enucleation (n = 4), cyst excision associated with bowel resections (n = 2), chyloma deroofing (n = 1), drainage (n = 1), endoscopic resection (n = 1), and laparoscopic resection (n = 1). Two of 19 patients failed conservative management and later required surgery. One individual presented as a case of acute pancreatitis whereas the other patient had a similar attack of subacute intestinal obstruction prior to the index admission. No recurrence was reported following surgical intervention.
Analysis of the viscous fluid in all patients confirmed the presence of chylomicrons, cholesterol crystals, and triglycerides, which is diagnostic of chyle. There were no malignant changes in any of the cysts excised.
Surgical excision of the cyst appears to be the most commonly employed strategy. This may be associated with bowel resection.2 ; 8 Based on this review, it appeared that conservative management is not feasible as all patients underwent surgery to be relieved of their symptoms. There were no reports of chylous mesenteric cysts with successful conservative management. Symptomatic cysts lead patients to seek medical attention. These cysts harbor the risk of undergoing torsion, rupture, compressive effects with increase in size, resulting in obstructive symptomatology. The incidence of asymptomatic chylous mesenteric cyst is not known. Although excision of cyst was the procedure most commonly performed, “enucleation” has been reported by some authors. It is unclear as to what the authors meant by this technique. Partial excision of cyst, drainage and deroofing also appear to work without resulting in recurrence.
The limitations of this study include the exclusion case reports prior to 1980 and presentation of similar cysts in children from the review. Patients with nonchylous mesenteric cysts were not included. Articles in non-English were also excluded. Therefore, valuable information pertaining to chylous mesenteric cysts in the excluded literature may have been missed.
In conclusion, chylous mesenteric cyst is a rare entity that needs to be recognized whenever a preliminary diagnosis of cystic intrabdominal mass is made. A long pedicled cyst of the mesentery may appear to originate from the ovaries or from any other pelvic organs, mimicking a pelvic mass.
References
- 1 M.F. O'Brien, D.C. Winter, G. Lee, E.J. Fitzgerald, G.C. O'Sullivan; Mesenteric cysts. A series of six cases with a review of the literature; Irish J Med Sci, 168 (1999), pp. 233–236
- 2 R.J. Kurtz, T.M. Heimann, J. Holt, A.R. Beck; Mesenteric and retroperitoneal cysts; Ann Surg, 203 (1986), pp. 109–112
- 3 M. dePerrot, M.A. Bründler, M. Tötsch, G. Mentha, P. Morel; Mesenteric cysts. Towards less confusion?; Dig Surg, 17 (2000), pp. 323–328
- 4 E. Kwan, H. Lau, W.K. Yuen; Laparoscopic resection of a mesenteric cyst; Gastrointest Endosc, 59 (2004), pp. 154–156
- 5 H. Takiff, R. Calabria, L. Yin, B.E. Stabile; Mesenteric cysts and intra-abdominal cystic lymphangiomas; Arch Surg, 120 (1985), pp. 1266–1269
- 6 E.I. Egozi, R.R. Ricketts; Mesenteric and omental cysts in children; Am Surg, 63 (1997), pp. 287–290
- 7 C. Oh, C.A. Danese, D.A. Dreiling; Chylous cysts of the mesentery; Arch Surg, 94 (1967), pp. 790–793
- 8 S.R. Pomper, L.F. Berliner, T.V. Madhavan, W.C. Frederick, M.H. Worth Jr.; Mesenteric chylous cyst associated with Crohns disease; Am J Gastroenterol, 82 (1987), pp. 798–801
- 9 C.G. Levison, M. Wolfssohn; A mesenteric chylous cyst; Cal West Med, 24 (1926), pp. 480–482
- 10 N.R. Feins, J.G. Raffensperger; Cystic hygroma, lymphangioma, and lymphedema; J.G. Raffensperger (Ed.), Swensons Pediatric Surgery (5th ed.), Appleton & Lange, Norwalk, Conn (1990), pp. 172–173
- 11 C. Lockhart, A. Kennedy, S. Ali, D. McManus, S.D. Johnston; Mesenteric cysts: a rare cause of abdominal pain; Ulster Med J, 74 (2005), pp. 60–62
- 12 K.K. Prasad, M. Jain, R.K. Gupta; Omental cyst in children presenting as pseudoascites: report of two cases and review of the literature; Indian J Pathol Microbiol, 44 (2001), pp. 153–155
- 13 R.R. Ricketts; Mesenteric and omental cysts; Pediatric Surgery (5th ed.), Mosby-Year Book, Inc, St. Louis, MO (1998), pp. 1269–1275
- 14 T. Yasoshima, M. Mukaiya, K. Hirata, et al.; A chylous cyst of the mesentery: report of a case; Surg Today, 30 (2000), pp. 185–187
- 15 P. Covarelli, S. Arena, M. Badolato, et al.; Mesenteric chylous cysts simulating a pelvic disease: a case report; Chir Ital, 60 (2008), pp. 319–322
- 16 T.P. Ho, V. Bhattacharya, M.G. Wyatt; Chylous cyst of the small bowel mesentery presenting as a contained rupture of an abdominal aortic aneurysm; Eur J VascEndovasc Surg, 23 (2002), pp. 82–83
- 17 S.C. Liew, D.C. Glenn, D.W. Storey; Mesenteric cyst; Aust N Z J Surg, 64 (1994), pp. 741–744
- 18 F.H. Lahey, E.B. Eckerson; Retroperitoneal cysts; Am Surg, 100 (1934), pp. 231–237
- 19 A.K. Vaughn, W.M. Lees, J.W. Henry; Mesenteric cysts; Surgery, 23 (1948), pp. 306–317
- 20 H.F. Wykypiel, R. Margreiter; Chylous cyst formation following laparoscopic fundoplication; Wien Klin Wochenschr, 119 (2007), pp. 729–732
- 21 L. Sarli, P. Cortellini, C. Pavlidis, M. Simonazzi, N. Sebastio; Successful management of para-aortic lymphocyst with laparoscopic fenestration; Surg Endosc, 14 (2000), p. 373
- 22 M.D. Rifkin, A.B. Kurtz, M.E. Pasto; Mesenteric chylous (lymph-containing) cyst; Gastrointest Radiol, 8 (1983), pp. 267–269
- 23 H.E. Longmaid 3rd, J. Tymkiw, E.A. Rider; Sonographic diagnosis of a chylous mesenteric cyst; J Clin Ultrasound, 14 (1986), pp. 458–460
- 24 G.W. Phillips, A. Senapati, A.E. Young; Chylolymphatic mesenteric cyst: a diagnostic appearance on computed tomography; Br J Radiol, 61 (1988), pp. 413–414
- 25 S.H. Chin, J.S. Gill; A large chylous cyst of the mesentery simulating an ovarian cyst: a case report; Asia Oceania J Obstet Gynaecol, 13 (1987), pp. 273–276
- 26 H. Nakamura, T. Hashimoto, H. Akashi, S. Mizumoto; Distinctive CT-findings of unusual mesenteric cysts; J Comput Assist Tomogr, 11 (1987), pp. 1024–1025
- 27 S.K. Stevens, M. Nino-Murcia, R. Bloom, K.L. Chang; Mesenteric cyst with atypical computed tomography appearance; Clin Imaging, 13 (1989), pp. 119–121
- 28 A. Latif al-Arfaj, A. al-Kreedees; Mesenteric chylous cyst. Case report; Eur J Surg, 157 (1991), pp. 557–558
- 29 M.M. Kamat, N.K. Bahal, S.R. Prabhu, M.V. Pai; Multiple chylous cysts of abdomen causing intestinal obstruction; J Postgrad Med, 38 (1992), pp. 206–207
- 30 S.P. Jain; Chylous mesenteric and retroperitoneal cysts of developmental origin amongst Ethiopians: report of four cases; Ethiop Med J, 30 (1992), pp. 233–238
- 31 N. Fujita, Y. Noda, G. Kobayashi, et al.; Chylous cyst of the mesentery: US and CT diagnosis; Abdom Imaging, 20 (1995), pp. 259–261
- 32 A. Protopapas, D. Papadopoulos, A. Rodolakis, S. Markaki, A. Antsaklis; Mesenteric lymphangioma presenting as adnexal torsion: case report and literature review; J Clin Ultrasound, 33 (2) (2005), pp. 90–93
- 33 A. Wiesen, K. Sideridis, B. Stark, S. Bank; Mesenteric chylous cyst; Gastrointest Endosc, 63 (2006), p. 502
- 34 S. Akwei, N. Bhardwaj, P.D. Murphy; Benign mesenteric lymphangioma presenting as acute pancreatitis: a case report; Cases J, 2 (2009), p. 9328
- 35 G.D. Tebala, I. Camperchioli, V. Tognoni, M. Noia, A.L. Gaspari; Laparoscopic treatment of a huge mesenteric chylous cyst; JSLS, 14 (2010), pp. 436–438
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?