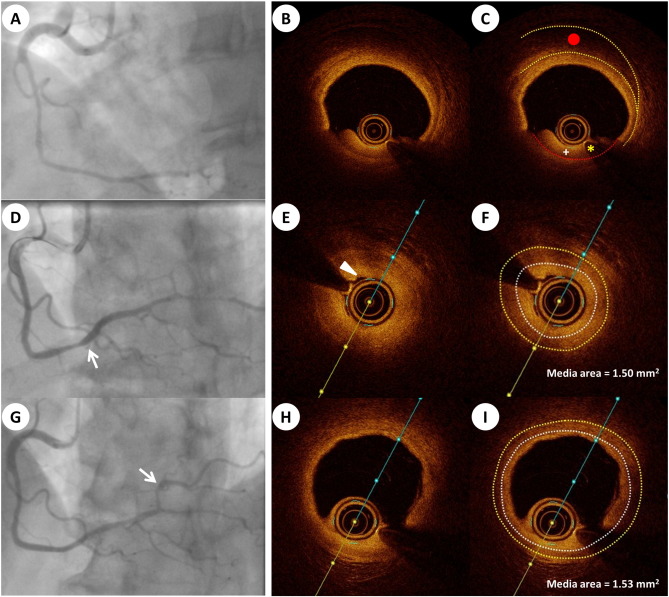
A 69-year-old woman with a history of treated hypertension, presented with sudden onset chest pain, at rest, and evidence of ST-segment elevation in the inferior leads of a 12-lead electrocardiogram. Urgent coronary angiography demonstrated an abrupt lumen calibre reduction extending from segment 2 of the right coronary artery (RCA) into the posterior descending artery, with preserved Thrombolysis In Myocardial Infarction (TIMI) 3 flow (Fig. 1A). The postero-lateral branch of the RCA was sub-totally occluded. Having confirmed patency of the infarct-related artery and complete resolution of the patients symptoms, we proceeded to evaluate the RCA with OCT. We demonstrated a false lumen with intramural haematoma at the lesion site, without clear evidence of intimal disruption (Fig. 1B and C). The patient suffered transient worsening of chest pain and ST-segment changes while the OCT catheter was distally occlusive. Interpretation of the angiographic and OCT findings suggested a diagnosis of spontaneous coronary artery dissection (SCAD) without intimal disruption and led us to take a relatively conservative strategy, limiting intervention to plain old balloon angioplasty (POBA) of the mid- and distal segments of the RCA with a 2.0 × 15 mm compliant balloon to enhance distal flow. Angiographic assessment post-POBA, revealed evidence of an iatrogenic dissection in the mid-vessel, with preserved TIMI-3 flow in all branches (Fig. 1D). At this time, the patient was haemodynamically stable and asymptomatic, therefore further intervention was avoided. Repeated angiography, on day 7, demonstrated improved luminal calibre in the affected segments and re-canalisation of the postero-lateral branch (Fig. 1G). The patient was asymptomatic and discharged on dual antiplatelet therapy for six months.
|
|
|
Fig. 1. A: Angiographic assessment demonstrating a diffuse tubular stenosis from segment 2 of the RCA; B and C: OCT image demonstrating false lumen with intramural haematoma (red point) and showing residual blood artefact (plus sign) (yellow border: external elastic membrane; red border: luminal contour; *: wire artefact); D: final angiographic assessment, at time of index procedure, demonstrating minor balloon-related dissection in the mid-vessel (arrow); E: OCT cross section in the mid-RCA showing medial layer thickness, with folding of the luminal intimal contour (arrow head); F: qualitative analysis of medial area (external elastic membrane (yellow border) – Internal Elastic Membrane (white border)) did not change when comparing the vessel with normal medial layer; G: improved intraluminal calibre with postero-lateral branch re-canalisation (arrow) on repeated angiography; H and I: OCT image showing a relatively normal vessel anatomy in the proximal RCA and the medial area of 1.53 mm2; Abbreviation: RCA = right coronary artery; OCT = optical coherence tomography. |
SCAD is a non-traumatic and non-iatrogenic separation of the coronary artery wall with associated intramural haematoma. The 2-dimensional lumenogram provided by coronary angiography has obvious limitations in detecting a pathological process affecting the arterial wall. Evidence of arterial wall staining is suggestive of intimal disruption (type 1 angiographic SCAD) and an abrupt calibre change with or without restoration of distal vessel calibre (type 2a & 2b angiographic SCAD, respectively) is a feature that should raise suspicion of a diagnosis of SCAD [1]. However, the pathognomonic appearance of type 1 SCAD is only observed in less than 1/3 of SCAD cases [2]. In SCAD cases without pathognomonic angiographic findings, the use of intra-coronary imaging modalities, particularly the high resolution (10 μm) provided by OCT, can visualise intimal disruption, intramural haematoma, and false lumen for SCAD diagnosis [3] ; [4]. However, there are potential limitations with OCT in the setting of SCAD, including the difficulty of blood clearance in a lesion with complete collapse of the lumen, and challenging image interpretation due to the appearance of high and low attenuating regions within the ‘false lumen’ zone [5].
In our case, dissection is observed at the level of the external elastic membrane with a low attenuation area observed behind the collapsed intima-media complex (Fig. 1B and C). Failure to clear the lumen of blood can pose challenges in the interpretation of the images and it is important not to overinterpret cross sectional images in isolation but instead to assess sequential images within the affected segment. The collapsed intima-media complex may be misinterpreted as a ‘diseased’ segment but measurement of the medial area and comparison with a normal reference segment confirm equivalent areas and strengthen the diagnosis of intramural compression, particularly when observed in associated with luminal contour folding (Fig. 1E, F, H and I).
Currently, our experience highlights the important role OCT plays in the diagnosis of SCAD, when angiographic assessment is ambiguous, and its potential for guiding therapeutic decision making. Early recognition may avoid unnecessary and potentially harmful intervention and allow a tailored approach to the ongoing care and risk modification for this challenging group of patients.
Conflict of interest
None.
References
- [1] J. Saw; Coronary angiogram classification of spontaneous coronary artery dissection; Catheter. Cardiovasc. Interv., 84 (2014), pp. 1115–1122
- [2] J. Saw, E. Aymong, T. Sedlak, C.E. Buller, A. Starovoytov, D. Ricci, S. Robinson, T. Vuurmans, M. Gao, K. Humphries, G.B. Mancini; Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes; Circ. Cardiovasc. Interv., 7 (2014), pp. 645–655
- [3] T. Nishiguchi, A. Tanaka, Y. Ozaki, A. Taruya, S. Fukuda, H. Taguchi, T. Iwaguro, S. Ueno, Y. Okumoto, T. Akasaka; Prevalence of spontaneous coronary artery dissection in patients with acute coronary syndrome; Eur. Heart J. Acute Cardiovasc. Care, 5 (2016), pp. 263–270
- [4] T.W. Johnson, D. Smith, J.W. Strange, C. Bucciarelli-Ducci, R. Lowe, A. Baumbach; Spontaneous multivessel coronary intramural hematoma: an insight with OCT; JACC Cardiovasc. Imaging, 5 (2012), pp. 1070–1071
- [5] V. Vizzi, T.W. Johnson, N. Jenkins, J.W. Strange, A. Baumbach; Dynamic separation of coronary artery medial and adventitial layers with vasospasm: new insights using OCT; Int. J. Cardiol., 167 (2013), pp. 2344–2345
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?