Summary
Objective
To summarize the characteristics of total hand degloving injury and investigate the curative effect of microsurgery.
Methods
A total of 46 patients with total hand degloving injury were enrolled in this study. The injury classification and treatment methods were as follows: Type I (11 cases), treated by replantation of the gloved skin; Type II (6 cases), treated by reconstruction using thumb wrap-around flap and second toe; Type III (4 cases), treated by reconstruction using bilateral second toe with dorsal foot flap; Type IV (9 cases), treated by replantation in situ or reconstruction; Type V (16 cases), treated by replantation or abdominal flap reconstruction.
Results
Of the patients who received Type I treatment, five completely survived, whereas eight had finger necrosis. In Type II, both the reconstructed fingers and hand flaps survived. For four patients who received Type III treatment, eight reconstructed fingers survived. In Type IV, two patients with reconstructed fingers survived, whereas the six with replantation in situ had necrosis of the partial palmar or hand dorsum skin. In Type V, nine patients with reconstructed fingers survived, and five cases with abdominal skin flap reconstruction and one case with anterolateral femoral flap survived. The restoration of hand appearance and function was the best in patients who received replantation. For reconstruction cases, however, the hand function was recovered to the basic self-care level. In cases with abdominal flap reconstruction, the hand function showed poor recovery.
Conclusion
Total hand degloving injury can be classified into different types according to the injury degree. The appropriate microsurgical treatment based on these types can produce better curative effect.
Keywords
degloving injury;flap;microsurgery;reconstruction;replantation
1. Introduction
Total hand degloving injury is one of the most serious hand injuries.1 ; 2 When the wrist is injured while operating a high-speed rolling or a weight-pressing machine, the individual pulls his/her hand outward with a jerk due to conditional reflexes. At this point, the skin of the hand has been pressed by the machine or weight. The injury mechanism is that the loose connections between the superficial soft-tissue structure of the skin and the deep bone, joint, and tendon are broken, resulting in separation of superficial tissues (e.g., skin and subcutaneous tissue) from deep tissues (bone, joint, and tendon), subsequently causing degloving injury of the hand.3
A majority of total hand degloving injuries are mechanical injuries, and the degree of injury is related to the force of tearing, extrusion, and rolling.4 The degloving plane of the hand generally lies in the superficial flexor or extensor tendon. However, it is difficult to perform dermoplasty for these type of injuries because of the structural integrity of the underlying skeleton.5 ; 6 Examination of cases with complete degloving of the hand shows that the dorsal hand vein and the palmar artery are usually retained in the proximal end, and thus, it is possible to replant this end; however, the distal end cannot be replanted as no vessels are generally retained here. In certain cases, the degloved skin cannot be used again because of extensive damage or contusion. Thus, there are certain difficulties while treating such patients.
Degloving injury of the hand can cause exposure of bones, joints, tendons, and other important structures in the wound surface. This requires early repair. Otherwise, the condition will cause necrosis of the bones, joints, and tendons, which may seriously affect the recovery of hand function.7 A number of treatment methods are available for degloving injury of the hand. Wrap-around abdominal flap reconstruction is a simple operative method, and can help cover the wound; however, the postoperative function recovery is not ideal.8 ; 9 Although a combination of an anterolateral thigh flap and pedicled groin flap was useful in reconstructing an injured hand, the restoration of function and appearance of the hand was not good.10 Multiple free contiguous toes for repairing degloving injury of the hand restores part of hand functions and has been reported to have better curative effect. However, the complicated surgical procedures and multiple vascular anastomotic stomas will cause poor blood supply, wide donor site, large trauma, and other defects. Therefore, this treatment is still controversial.11 ; 12 In this study, five kinds of surgical methods were performed on 46 patients with total hand degloving injury in Ruihua Hospital Affiliated to Soochow University from December 1999 to May 2012. The characteristics of total hand degloving injury were summarized, and the curative effect of microsurgical treatment was investigated.
2. Patients and methods
2.1. Patients
A total of 46 patients [33 men and 13 women; age, 18–58 years (average 32 years] with total hand degloving injury were enrolled in this study. Of the 46 patients, 23 were injured in the left hand, and the remaining 23 were injured in the right hand. The injury was caused by a roller or roller crush (n = 25 cases), printing machine (n = 14 cases), and noodle press (n = 7 cases). The time from injury occurrence to surgery was 1–10 hours (average, 3 hours).
2.2. Injury classification
Based on severity, the total hand degloving injury was classified into the following five types: (1) Type I (11 cases): The degloved skin was from the wrist to the proximal plane of fingers 1–5. The degloved skin was complete, without contusion (7 cases) or with light contusion (4 cases). The entire musculoskeletal unit of the finger was intact, with normal blood circulation in fingers 1–5. (2) Type II (6 cases): The degloved skin was from the wrist to the proximal plane of fingers 1–5. The degloved skin was seriously contused or with defect. The entire musculoskeletal unit of the thumb was intact, with defect from the distal to proximal plane of fingers 2–5. (3) Type III (4 cases): The degloved skin was from the wrist to the proximal plane of fingers 1–5. The degloved skin was seriously contused or with defect. There was defect distal to all the five planes of the metacarpophalangeal joint or finger body was damaged. (4) Type IV (9 cases): The degloved skin was from the wrist to fingertips 1–5 or completely gloved, and the gloved skin was complete. The entire musculoskeletal unit was intact, but without blood circulation in fingers 1–5. (5) Type V (16 cases): The degloved skin was from the wrist to 1–5 fingertips or completely degloved. The degloved skin in this type was seriously contused or with defect. The entire musculoskeletal unit of the thumb was intact.
2.3. Microsurgical treatment methods
The microsurgical treatment methods adapted for different types of injury in this study were as follows: (1) Type I: The patients were treated by replantation of gloved skin, with revascularization. The dorsal hand vein, palm-side vein, and ruptured common palmar digital artery were anastomosed. The dorsal skin and palmar skin of the hand were slightly thinned and dressed with light pressure. (2) Type II: The replantation was constructed using thumb wrap-around flap with dorsal foot flap and second toe with dorsal foot flap. (3) Type III: The replantation was constructed using bilateral second toes with dorsal foot flap. (4) Type IV: Gloved skin replantation with revascularization was performed in seven cases. For two cases with seriously contused skin, the replantation was constructed using thumb wrap-around flap with dorsal foot flap and second toe with dorsal foot flap. (5) Type V: The replantation was constructed using thumb wrap-around flap with dorsal foot flap and second toe with dorsal foot flap in nine cases. Replantation using bilateral free anterolateral femoral flaps was performed in one case. The remaining six cases received abdominal wrap-around flap reconstruction after amputation of the middle finger segment distal to the flexor digitorum superficialis tendon.
The area of the dorsal foot skin flap was from 9 cm × 6 cm to 17 cm × 11 cm. The great toe was intercepted at the interphalangeal joint, and the second toe was intercepted at the metatarsophalangeal joint. The dorsal donor area of the foot was replanted using full-thickness skin abdominal flap. Three to six weeks after the surgery, the flap pedicle was amputated; 3 months later, surgical syndactyly division (two to three times) or flap thinning surgery was performed. For one patient who received replantation using bilateral free anterolateral femoral flaps, the surgical syndactyly division or flap thinning surgery was performed after 3 or 6 postoperative months, respectively.
3. Results
3.1. Overall results
For 11 cases with Type I injury, after vascular anastomosis and replantation, five survived completely. Two cases experienced complete necrosis of fingers 1–5. Therefore, we performed finger amputation, and the wound surface was treated with reconstruction using an abdominal skin flap. After surgery, however, the hand function was lost completely. The remaining four cases with partial finger necrosis received finger amputation. Six cases with Type II injury were treated with second toe wrap-around flap reconstruction with foot dorsal flap and hallux nail flap reconstruction with dorsal flap of the foot. After surgery, both the reconstructed fingers and the hand flaps survived. For four cases with Type III injury, after reconstruction using bilateral second toes, the eight reconstructed fingers survived. For nine cases with Type IV injury, after replantation or reconstruction, two cases with reconstructed fingers survived. In seven cases with replantation in situ, the palmar skin or hand dorsal skin became necrotic, which was subsequently treated by secondary reconstruction using skin flap. In the 16 cases with Type V injury, thumb nail flap or hallux nail flap for reconstruction was used in nine cases; six cases opted for abdominal flap; and one case received bilateral lateral femoral flaps. In the nine cases using the thumb nail flap or hallux nail flap, the reconstructed fingers survived. Of the six cases who received abdominal flap, five survived. These patients received surgical syndactyly division or skin flap thinning surgery (1–3 times) in the late stages. The flap survived in the patient who received bilateral lateral femoral flaps. This patient received surgical syndactyly division or skin flap thinning surgery (two times) in the late stages. The postoperative complication was mainly the injury to the donor site. For cases with transplantation of tissue in foot, the foot shape and function were slightly altered, with obvious scar in the donor site.
The follow-up was performed for 6 months–9.2 years (average, 3.6 years). For patients with anastomosis and replantation, the restoration of hand appearance and function was the best. For patients with reconstruction using the hallux nail flap or thumb nail flap, the hand function recovered to the basic self-care level. For patients with reconstruction using abdominal flap and anterolateral thigh flap, the restoration of hand was not good, and only the holding function was recovered (Table 1).
| Injury type | Treatment | Functional outcome |
|---|---|---|
| I | Replantation of the gloved skin, with revascularization | Good hand function restoration in finger survival cases and complete hand function loss in necrosis cases. |
| II | Reconstruction using thumb wrap-around flap and second toe | The holding, catching, and pinching functions were restored. |
| III | Reconstruction using bilateral second toes with dorsal foot flap | The holding, catching, and pinching functions were restored. |
| IV | Replantation in situ or reconstruction | The hand shape and basic functions were restored. |
| V | Replantation or abdominal flap reconstruction | Only the holding function was restored. |
3.2. Typical cases
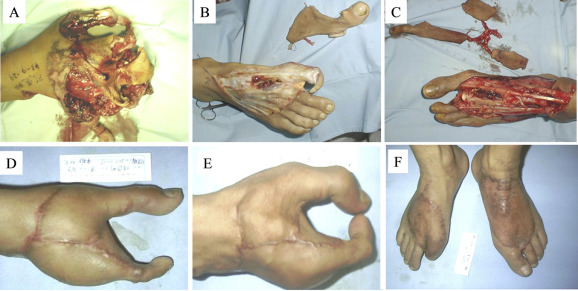
Case 1 (female; age, 43 years): The total hand degloving injury was caused by compaction of printing machine roller, and she was hospitalized 2 hours later. An examination of her hand showed that the degloving injury occurred at the left hand from the distal forearm to the fingertips. Both the deep fascia of the forearm and the muscle units remained intact. Acute debridement was performed under brachial plexus block, and then six dorsal hand veins, five palmar veins, and the ruptured common palmar digital artery were anastomosed. The dorsal skin and palmar skin of the hand were slightly thinned and dressed with light pressure. After 12 days, the replanted skin and the five fingers survived. After 12 months, there was repeated exudate at the distal index finger. X-ray showed absorption of the ungual phalanx. Therefore, distal finger amputation was performed. Follow-up 2 years later showed that the texture of the palm and dorsum of the hand was good, and the finger shape was excellent. The thumb abduction function, and finger flexion and extension functions recovered satisfactorily. The sensory function of the fingers was restored to Grade S2–S3 ( Fig. 1).
|
|
|
Figure 1. Total hand degloving injury (Case 1). (A) Before surgery. (B) Palm side immediately after surgery. (C) Dorsal side immediately after surgery. (D) Palm side at 2 years after surgery. (E) Dorsal side at 2 years after surgery. (F) Finger flexion function at 2 years after surgery. |
Case 2 (male; age, 24 years): The total hand degloving injury was caused by compaction of printing machine roller. He was hospitalized 1 hour later. An examination of his hand showed that the degloving injury occurred at the left hand. The skin was damaged from the proximal palm and dorsum of the hand to the fingertips. The phalangeal joints, tendon, nerve, and intrinsic muscles of the hand were relatively complete. Classic acute debridement was performed under a combination of brachial plexus block and epidural anesthesia, reserving the thumb. The fingers 2–5 were amputated at the metacarpophalangeal joint. The hallux nail flap with the right foot dorsal flap was used to reconstruct the thumb and repair the radical skin defect of the palm and dorsum of the hand (tigers mouth area). The second toe wrap-around flap with left foot dorsal flap was used to reconstruct the middle finger and repair the ulnar skin defect of the palm and the dorsum of the hand. After surgery, all the middle finger and thumb flaps survived. Follow-up after half a year showed that the flaps of palm and dorsum of the hand were not bulky, and the abduction function of the thumb was recovered. The flexion and extension functions of the metacarpophalangeal joint were normal, and could complete the digital opposition motion. The sense of the reconstructed finger and flap was recovered to Grade S2, with good healing in the donor site in the foot skin. There was no obvious cicartricial contracture in the replanting area or problems with walking ( Fig. 2).
|
|
|
Figure 2. Total hand degloving injury (Case 2). (A) Before surgery. (B and C) Incised flap during surgery. (D) Hand appearance at 6 months after surgery. (E) Finger function at 6 months after surgery. (F) Donor site at 6 months after surgery. |
4. Discussion
When the hand suffers from alien violence or roller compaction, the body produces a protective reflex and strongly retracts, which leads to hand skin and soft-tissue degloving. Hand soft tissues including skin, subcutaneous fascia, vascular blood vessels, nerve, bone and tendon are degloved together,13 which are characterized by irregular margins, contusion, and avulsion of the skin. As a result, the blood vessels, nerves, tendons, bones, and joints are often not in the same plane. Meanwhile, vascular intima is seriously contused, and even the arteries and nerves are drawn out. The dorsum skin of the hand is often avulsed from the superficial layer of the deep fascia. The palm-side skin is often avulsed from superficial palmar aponeurosis. The finger skin is often avulsed from the flexor tendon sheath and superficial extensor tendon. After a degloving injury, the superficial veins of skin are all damaged. Although part of the skin is connected with the root of the finger or the proximal part of the finger tendons, the digital artery is often damaged due to pulling.
In total hand degloving injuries, the palmar vein and dorsum vein of the hand generally attach to the plane of the metacarpophalangeal joint, and the veins proximal to the plane attach to the deep fascia layer, but not to the degloved skin. The veins distal to the plane mostly attach to the degloved skin, thereby creating conditions for a successful replantation. As the fingers often have arterial blood, the venous return is not sufficient. Whether the venous return is unobstructed directly relates to the survival of finger and skin. Therefore, establishment of adequate venous return is very important during surgical procedures. The fractured artery plane is at the metacarpophalangeal joint plane in the thumb, and at the proximal segment of the proximal plane in the fingers. Similarly, the proximal artery remains in the palm, with the distal artery in the degloved skin, thus creating surviving conditions for fingers without arterial blood circulation. The anastomosis or transplantation of bridging vein in this plane can reconstruct the blood circulation.14 ; 15 In replantation cases of this study, there was blood circulation in most fingers, and the degloved skin integrity was good, with no obvious contusion or light contusion, whereas the degloved skin in most other cases is either incomplete or severely bruised. Therefore, the skin condition is the key for successful replantation. However, it is not easy to judge the skin condition accurately, and this is mainly based on experience.16
According to severity, total hand degloving injury is often classified into five types: I, II, III, IV, and V, and then the corresponding treatment programs are formulated. In this study, there were 11, 6, 4, 9, and 16 cases with Types I, II, III, IV, and V total hand degloving injury, respectively. All cases were successfully treated by microsurgery. Follow-up shows that all the treatment methods can complete the wound coverage, and the damage to the donor site is reduced to the minimum. Replantation cases had the best restoration of hand appearance and function. In cases with reconstruction using the hallux nail flap or thumb nail flap, the hand function can recover to the basic self-care level. Of course, the particular surgery scheme is not completely in accordance with the aforementioned typing scheme. Other factors including age, general condition of patient, and surgical experience should also be considered during categorization and subsequent surgery.11 ; 17 In this study, there were patients with older age and poor body condition. After traditional reconstruction using abdominal skin flap, only the holding function of hand was recovered. For two replantation cases with necrosis in all fingers and partial skin in the palm and dorsum of the hand, after secondary amputation of fingers 1–5, the reconstruction using abdominal flap is also adopted.
In conclusion, hand degloving injury often causes exposure of tendon, bone, and joint, and thus, earlier wound coverage and functional exercise are very important.18 ; 19 Clinical classification according to the characteristics of degloving injury and the corresponding treatment methods can help physicians make a correct judgment on the patients condition, enabling them to choose the appropriate therapy. Thus, prompt and timely surgical procedures can be provided. This not only can completely repair the hand wound and obtain better hand appearance and function, but also can reduce the damage to the donor site, shorten the treatment time, and reduce the pain of patients, thereby reducing their physical and mental burden.
References
- 1 D. Ulrich, N. Pallua; Treatment of avulsion injury of three fingers with a compound thoracodorsal artery perforator flap including serratus anterior fascia; Microsurgery, 29 (2009), pp. 556–559
- 2 C. Chen, X. Zhang, X. Shao, S. Gao, B. Wang, D. Liu; Treatment of thumb tip degloving injury using the modified first dorsal metacarpal artery flap; J Hand Surg Am, 35 (2010), pp. 1663–1670
- 3 R. Krishnamoorthy, G. Karthikeyan; Degloving injuries of the hand; Indian J Plast Surg, 44 (2011), pp. 227–236
- 4 L.K. Wong, R.D. Nesbit, L.A. Turner, L.A. Sargent; Management of a circumferential lower extremity degloving injury with the use of vacuum-assisted closure; South Med J, 99 (2006), pp. 628–630
- 5 M. Fujiwara, H. Fukamizu; Delayed wraparound abdominal flap reconstruction for a totally degloved hand; Hand Surg, 13 (2008), pp. 115–119
- 6 H. Koch, H. Moshammer, S. Spendel, G. Pierer, E. Scharnagl; Wrap-around arterialized venous flap for salvage of an avulsed finger; J Reconstr Microsurg, 15 (1999), pp. 347–350
- 7 R. Adani, I. Marcoccio, C. Castagnetti, L. Tarallo; Long-term results of replantation for complete ring avulsion amputations; Ann Plast Surg, 51 (2003), pp. 564–568
- 8 J.P. Pradier, C. Oberlin, E. Bey; Acute deep hand burns covered by a pocket flap-graft: long-term outcome based on nine cases; J Burns Wounds, 6 (2007), pp. e1–e32
- 9 S. Nazerani, M.H. Motamedi, T. Nazerani, B. Bidarmaghz; Treatment of traumatic degloving injuries of the fingers and hand: introducing the “compartmented abdominal flap”; Tech Hand Up Extrem Surg, 15 (2011), pp. 151–155
- 10 H. Senda, H. Muro, S. Terada, H. Okamoto; A case of degloving injury of the whole hand reconstructed by a combination of distant flaps comprising an anterolateral thigh flap and a groin flap; J Reconstr Microsurg, 27 (2011), pp. 299–302
- 11 B.P. Thomas, T.M. Tsai; Primary reconstruction of a degloved hand using multiple toe transfers on a single pedicle and a reversed radial artery flap; J Reconstr Microsurg, 20 (2004), pp. 3–6
- 12 A.M. Doctor, J. Mathew, S. Ellur, A.A. Ananthram; Three-flap cover for total hand degloving; J Plast Reconstr Aesthet Surg, 63 (2010), pp. e402–e405
- 13 P. Kitidumrongsook, A. Patradul, K. Pataradool; Resurfacing the degloved thumb up to the interphalangeal joint level with twin extended neurovascular island flaps; J Hand Surg Br, 31 (2006), pp. 562–565
- 14 A. Rodríguez-Lorenzo, C.H. Lin, C.H. Lin, W.C. Ching, Y.T. Lin; Replantation of a degloved hand with added arteriovenous anastomoses: report of two cases; J Hand Surg Am, 34 (2009), pp. 1864–1867
- 15 R. Adani, E. Pataia, L. Tarallo, R. Mugnai; Results of replantation of 33 ring avulsion amputations; J Hand Surg Am, 38 (2013), pp. 947–956
- 16 K. Ozaksar, T. Toros, T.S. Sügün, M. Kayalar, I. Kaplan, S. Ada; Finger replantations after ring avulsion amputations; J Hand Surg Eur Vol, 37 (2012), pp. 329–335
- 17 B.P. Thomas, E. Katsarma, T.M. Tsai; Replantation of total degloving of the hand: case report; J Reconstr Microsurg, 19 (2003), pp. 217–220
- 18 D.N. Deal, J. Barnwell, Z. Li; Soft-tissue coverage of complex dorsal hand and finger defects using the turnover adipofascial flap; J Reconstr Microsurg, 27 (2011), pp. 133–138
- 19 K.S. Kim, E.S. Kim, D.Y. Kim, S.Y. Lee, B.H. Cho; Resurfacing of a totally degloved hand using thin perforator-based cutaneous free flaps; Ann Plast Surg, 50 (2003), pp. 77–81
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?