Abstract
The current scientific understanding of adolescent depression is incomplete, requiring further research and attention. This review of Selective Serotonin Reuptake Inhibitors (SSRIs) in the context of adolescent depression seeks to inform adolescents about the mechanisms in which SSRIs affect the body, common side effects associated with this class of antidepressants, and the efficacy rates of SSRIs in their population group. This review also underscores the gaps in research regarding both adolescent depression and adolescent antidepressant usage. When considering the use of prescription drugs, especially ones that have large implications towards neurological function, it is essential to understand all facets of the medication. This review provides adolescents and their families with direct information that will inform their thinking about SSRI use. This review considers academic and popular sources in collating evidence for the impact and efficacy of SSRIs on adolescents. Through careful analysis of the consequences and benefits associated with SSRI usage, this review provides a comprehensive scientific overview of SSRIs. To inform adolescents and their families, this review will first offer a mechanistic overview of the SSRI drug class, next evaluate evidence for the neurological effects of SSRIs on the adolescent brain, and then highlight clinical testing of two specific SSRIs, Fluoxetine and Escitalopram. Both the implications of SSRIs on adolescent brain development and their possible short-term and long-term negative side effects are considered in this review. Most importantly, this review draws attention to the multitude of unknowns surrounding SSRI usage in adolescents and urges researchers to continue evaluating the implications of early antidepressant usage. With an adolescent centered viewpoint and a focus on extensivity, this report provides adolescents and their families with the resources to make personalized decisions about SSRI exposure.
Key Words
Adolescent depression
Fluoxetine
Escitalopram
Major Depressive Disorder
Selective Serotonin Reuptake Inhibitors
Serotonin Theory of Depression
Serotonin
Introduction
Overview of Depression
The earliest documented cases of depression date back to the 4th century BCE, when the mental health condition was initially classified as “melancholia” by Greek physician Hippocrates. This condition has been recorded for over 2 millennia, however, its prevalence has been increasing at an elevated rate in recent decades. Increased rates of depression are not only due to a growing number of depressed individuals, but also due to changes in medical diagnostics. Prior to the twentieth century, depressive symptoms were regarded as a problem of nerves by medical professionals. Medical diagnosis of depression began to change in the 1970s, resulting in depression, rather than anxiety, becoming a more common classification for people suffering from high stress (1). Medical professionals decided on nine key criteria for diagnosing patients with depression: sleep disturbances, pleasure reduction, thoughts of worthlessness, fatigue, attention deficits, weight changes, psychomotor disturbances, suicidal thoughts, and depressed mood (2).
| Core Symptoms of Major Depressive Disorder |
| One or Both of the Following |
| A diminished or irritable mood |
| Decreased interest or pleasure (anhedonia) |
| And Four or More of the Following |
| Feelings of guilt or worthlessness |
| Fatigue or loss of energy |
| Concentration problems |
| Suicidality or thoughts of death |
| Weights gains or weight loss (5% changes in weight) |
| Psychomotor retardation or activation (change in activity) |
| Hypersomnia or insomnia (change in sleep) |
Table 1. A comprehensive list of nine biological, affective, somatic, and cognitive symptoms of depression. Repurposed from the Indian Journal of Psychiatry under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License. 10.4103/psychiatry.IndianJPsychiatry_446_18
A person with five out of these nine symptoms possesses a sufficient number of symptoms to be diagnosed with depression (2). This development in medical diagnosis can be mainly attributed to political factors and economic motivations. Through these changing classifications of depression, the branch of psychiatry became a more respected branch of medical science and pharmaceutical companies were able to make immense profits (1) from the development of antidepressants during the 1950s.
The American Psychiatric Association defines depression as a common and serious medical illness that negatively affects how you feel, the way you think, and how you act. Depression differs from common temporary feelings of sadness in regard to duration and circumstance. Feelings of sadness are temporary, usually subsiding after a few hours or days. Depression is characterized by consistent feelings of sadness or a lack of motivation that extends beyond 2 to 3 days. Generally, patients are diagnosed as having depression after exhibiting the aforementioned symptoms for over two weeks (3). Normal feelings of sadness are caused by outside events or pressures in one’s life. On the contrary, depression is a mood disorder that is caused by an imbalance of neurotransmitters, genetics, medical conditions, medication, and external events (4). Major depressive disorder is more complex than regular sadness, and its complete causes and effects are still not fully understood.
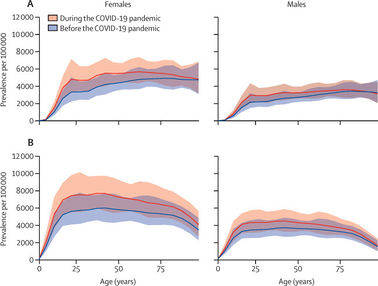
Although psychiatrists are more frequently diagnosing patients with depression in comparison to prior eras, data shows that overall depression rates, both globally and nationally, are on the rise. Metrics released by the World Health Organization illustrate that following the COVID-19 pandemic, the global prevalence of anxiety and depression increased by 25% (5). A study published in the Journal of Psychiatry Research provides data about the long term trends of global depression, showing that the condition has been on the rise for the past few decades. The study quantifies this claim, stating that worldwide cases of depression increased from 172 million in 1990 to 258 million in 2017, representing an increase of approximately 50% (6).
Figure 1. Global prevalence of major depressive disorder (A) and anxiety disorders (B) before and after adjustment for (ie, during) the COVID-19 pandemic, 2020, by age and sex. Repurposed from The Lancet under the Creative Commons CC-BY. 10.1016/S0140-6736(21)02143-7
The United States is among the countries with the most citizens suffering from MDD. CNN reports that, as of March, 2023, about 18% of adults in the United States say they are depressed or are receiving treatment for depression (7). Many American politicians and psychiatrists cite a lack of support as the main factor behind growing national levels of depression. A separate CNN article outlined that the ability to access mental health services actually went down following the pandemic (8). Combined, these factors have produced a sharp rise in nationwide levels of depression, increasing the scale of antidepressant usage for both adolescents and adults. With rates of depression growing in magnitude, it is quintessential that adolescents, as well as the greater global populations, are aware of the condition as well as the relative merit of different treatment options.
History of Depression in Adolescents
The history of depression in adolescents has been characterized by profound scientific misunderstanding and dismissal. Although cases of depression in adolescents were reported as early as the 17th century, early theories of depression suggested that the developing brains of youth did not have the imperative psychological systems to suffer from MDD, an extremely severe form of depression (9). It was only in 1975, when the National Institute of Mental Health met with the goal of discussing adolescent depression, that basic diagnostic criteria were established for this population (9). The established symptoms for adolescent depression include depressed mood or irritability, diminished pleasure, significant weight loss, insomnia, psychomotor impairment, fatigue, feelings of worthlessness, diminished ability to think or concentrate, and recurrent thoughts of death (10). If 5 or more of these symptoms are expressed for longer than a two-week duration, adolescents would be diagnosed as having a major depressive episode (10). Though having similar symptoms as adult depression, adolescent depression more commonly manifests in the form of social withdrawal and isolation. Although now accepted as an existent condition, until recently, scientists continued to believe that symptoms of childhood depression, including sadness, self-doubt, and social withdrawal, were universal characteristics of early development, and that they should not be categorized as MDD. Early misdiagnoses and misunderstandings created a scarcity of accurate information about adolescent depression. The effects of this misdiagnosis and misrepresentation persist today in the form of minimal guidelines and standardized procedures for treating adolescents with SSRIs.
Depression in Adolescents
Many teenagers and young adults, who are the subject of greater numbers of clinical studies than solely adolescents, suffer from depression. Young adults, who are typically defined as individuals between 18–30 years of age, are the most at-risk population for the development of depression (11). Anxiety and depression are becoming increasingly prevalent among young adults in the US, with both disorders increasing by 63% from 2005 to 2017 (11). While depression negatively affects people of all age groups, its high prevalence within young adults is especially troubling because it further exacerbates the difficulties of navigating life at a pivotal time, marked by both physical and psychological development. While the exact causes of the heightened prevalence of depression in young adults is not certain, researchers and psychiatrists agree that academic stressors, genetics, and modern social media are major contributing factors. In several studies conducted by the Child Mind Institute, teenagers and young adults who spent the most time on Instagram, Facebook, and other platforms were shown to have substantially, from 13 to 66 percent, higher rates of reported depression than those who spent less time (12). Social media continues to negatively impact youth mental health, contributing to widespread depression. As previously noted, academic stress is another key component behind depression in youth. A separate study conducted at a prestigious university in China found that students who were exposed to a high academic stress environment experienced anxiety, which further contributed to depression (13). School-related stress has been observed to compound itself with other stressors, further contributing to increased levels of depression in young adults (13). Finally, a family history of depression can be a determinant of adolescent depression (14). Gender and specific stress responses are other ways that depression can be influenced by genetics. In terms of risk, current evidence suggests that genetic influences on an adolescent’s risk for developing depression are moderate but relevant (15). Combined, these three factors have been closely linked to adolescent depression, and are an area that are critical to consider during the development of new treatment strategies.
Selective Serotonin Reuptake Inhibitors
The increase in depression has resulted in the development of various antidepressants that seek to mitigate depressive symptoms. Currently, there is no cure for depression. The most commonly used class of antidepressants is the selective serotonin reuptake inhibitor (SSRI) class. SSRIs were developed in the 1970s, revolutionizing antidepressants and their capabilities. These new antidepressants provided a safer alternative to monoamine oxidase inhibitors and tricyclic antidepressants, two previous drug classes that had been associated with many severe side effects.
As a class, SSRIs target serotonin levels in the brain to reduce depressive characteristics. The first SSRI, zimelidine, was developed in the late 1970s by Arvid Carlsson. While this antidepressant was initially prescribed successfully throughout Europe, it was eventually linked to severe side effects, such as hypersensitivity reactions and Guillain-Barre syndrome, ultimately leading to the drug's withdrawal from global markets. Later, the Eli Lilly company introduced a new SSRI, Fluoxetine. Clinical trials for fluoxetine lasted 7 years and the drug was released in January of 1987. Currently, fluoxetine and its 4 other SSRI counterparts: citalopram, escitalopram, paroxetine, and sertraline, are the first line of antidepressants for clinicians globally. SSRIs are used to primarily treat depression, but can also treat patients with general anxiety disorder and bulimia nervosa.
All selective serotonin reuptake inhibitors have similar mechanisms of action. However, the drug class differs with regard to efficacy, metabolism, rate of elimination from the body, and interactions with other prescription drugs an individual may be using simultaneously (16). Moreover, specific dosages, respective kinetics, and possible side effects vary across the SSRI class. Medical professionals should carefully consider specific attributes of SSRIs before deciding on the most suitable antidepressant.
Common Treatments
Aside from selective serotonin reuptake inhibitors, many other antidepressants are utilized to treat MDD. There are seven total classes of antidepressants, which include selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors, atypical antidepressants, serotonin modulators, tricyclic antidepressants, monoamine oxidase inhibitors, and NMDA antagonists (17). Across these classes, over 30 antidepressants have been approved by the FDA to treat MDD (17). Each antidepressant targets a specific neurotransmitter in the synapse, either serotonin or norepinephrine, allowing them to modulate mood and lessen depressive feelings.
Aside from antidepressants, various other treatments for MDD in adolescents exist, although many lack extensive research into their efficacy and mechanisms. A review of alternative treatments for MDD outlines St John’s wort, folate, S-adenosylmethionine, acupuncture, exercise, Omega-3 fatty acids, and therapy as other options for treating the condition(18).
Purpose
This review, centered around Selective Serotonin Reuptake Inhibitors in the context of adolescent depression, seeks to inform adolescents about the function of SSRIs, common side effects associated with SSRIs, the efficacy of SSRIs in this population group, areas of adolescent depression that require further exploration, and other aspects of the antidepressant class that are not clearly outlined by commonly used search engines.
Methods
The approach taken to extensively review selective serotonin reuptake inhibitors and their implications toward adolescents is detailed as follows. This review offers a holistic and bipartisan review of SSRIs. This review was compiled using the Google Scholar, Pubmed, ScienceDirect, ResearchGate, and Google search engines. Articles from the journal of psychiatric research, Childmind Institute, The Lancet, the journal of clinical psychiatry, British journal of clinical pharmacology, ScienceDirect, Mayo Clinic, Harvard Health, Nature News, the journal of adolescent health, journal of psychiatry & neuroscience, the Nordic journal of psychiatry, the journal de l’Academie canadienne de psychiatrie de l’enfant et de l’adolescent, the journal of psychopharmacology, and Frontiers are cited in this review. Key search terms included: “selective serotonin reuptake inhibitors,” “serotonin,” and “depression.” All searches included the term “adolescents,” and where insufficient literature was found, the term was removed to find information regarding general depression and SSRI efficacy. Statistics surrounding general depression were found through popular articles, while scholarly and scientific articles were utilized to gather information regarding clinical trials, longitudinal trends, and specific effects of SSRIs.
Papers were initially screened through abstract and title. Studies that demonstrated sufficient credibility, either by aligning with other reviews on the topic or coming from well-respected authors, and that had more than five outside citations, were included in this review. Articles older than 1990 were exempt. Papers pertaining to adolescents, as compared to all populations, were favored in this review. Specific studies were excluded if they focused on mood disorders other than depression, or if they referenced treatments that were not specific to MDD. Additionally, opinions and commentaries from medical researchers were excluded. The data extracted from sources included main findings, experimental protocols, and statistical outcomes. Variance in protocol and experimental design were accounted for through a synthesis of all extracted data. Overlapping patterns and consistencies were preferred over raw data. The prevalence of common side effects, efficacy of antidepressants, and causes of depression were expressed in terms of conclusions rather than their specific quantifications, as each review contained separate criteria and methods. This methodology allowed for cohesive analysis of SSRI usage in adolescents. Some animal studies were included, however human trials were favored. All included studies met ethical standards as outlined by the National Institute of Health and American Psychological Association.
The limitations of this review surround its limited variety of search engines and a general lack of sources that was confronted. Gaps in literature emerged when searching for articles that pertained to longitudinal studies, specific side effects, and treatment options. This review called attention to these gaps, but also acknowledges that the information included within this review may possess less validity and may be prone to generalizations. Through a critical assessment of quality, credibility, and relevance, this review provides a comprehensive and replicable overview of selective serotonin reuptake inhibitors and their impacts towards adolescents.
Age Limits of SSRIs
Depression in Adolescents
Current metrics illustrate that major depressive disorder has been increasing among adolescents, but specifically in adolescent girls (19). As a population, adolescents have reported higher instances of stress, anxiety, and self-harm throughout the 2000s (20). This general trend throughout the 21st century was further exacerbated by the COVID 19 pandemic. The percent of adolescents who reported depressive symptoms increased from 5% in the pre-pandemic period to 6.2% in the pandemic period (21). The onset of major depressive disorder in all populations has been linked to alterations of physical aspects in the brain. Changes in the volume of the frontal cortex, changes in shape of the left thalamus, decreased gray matter intensity in the ventral striatum, and increased cortical thickness in the left inferior parietal gyrus have been observed in patients suffering from depression (22). There is not currently a comprehensive scientific understanding of what impacts these physical changes have on the brain, and further research is being conducted into specific treatments that target these transformations. Specific brain alterations that have been commonly observed in adolescents suffering from depression include greater grey-matter volumes in the dorsolateral prefrontal cortex and lower grey-matter volumes in the hippocampus (23). These alterations suggest that adolescents experiencing depression were more likely to experience delayed brain maturation and an increased level of neuronal reorganization (23). Common symptoms associated with depression in adolescents are low mood or irritability, cognitive disturbances, sleep disturbances, negative self-perception, and suicidal ideation (24). Scientists and psychiatrists have a basic understanding of the effects of MDD on the developing brain, but a lack of comprehensive research leaves questions about specific neurological alterations unanswered. Currently known long-term effects of childhood depression include a heightened rate of recurrence in adulthood, increased risk of bipolar disorder, and an exacerbated chance of substance abuse later in life (25).
Variations Between Depression in Adolescents and Adults
Major Depression Disorder manifests similarly in both adolescents and adults, however, there are several key differences between the respective populations. While adolescents are more likely to experience vegetative symptoms, such as weight change, and physical disturbances when suffering from MDD, adults tend to exhibit anhedonia, a loss of pleasure, and a general loss of interest at greater rates (26). A major difference between the treatment of MDD in adults and adolescents is that tricyclic antidepressants, a class of antidepressants produced in the 1960s, have not successfully mitigated MDD during adolescent clinical trials (27). Currently, only two antidepressants are approved for usage in patients under the age of 18 suffering from depression: fluoxetine and escitalopram (26). This varies from adult populations, where SSRIs, serotonin and norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, and tricyclic antidepressants are approved as treatment options for MDD.
| Medication | Age (in years) | Diagnosis |
| Clomipramine (Anafranil) | 10 and older | Obsessive-compulsive disorder (OCD) |
| Duloxetine (Cymbalta, Drizmalma Sprinkle) | 7 and older | Generalized anxiety disorder |
| Escitalopram (Lexapro) | 12 and older | Major depressive disorder |
| Fluoxetine (Prozac) | 8 and older
7 and older |
Major depressive disorder
OCD |
| Fluvoxamine | 8 and older | OCD |
| Lurasidone (Latuda) | 10 and older | Bipolar depression |
| Olanzapine and fluoxetine, combination drug (Symbyax) | 10 and older | Bipolar depression |
| Sertraline (Zoloft) | 6 and older | OCD |
Table 2. FDA-approved antidepressants for children and teenagers. Repurposed from the Mayo Clinic from a public domain. https://www.mayoclinic.org/diseases-conditions/teen-depression/in-depth/antidepressants/art-20047502
Age Restrictions for SSRIs
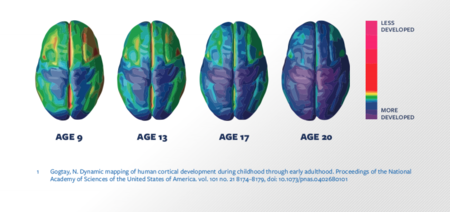
Fluoxetine, a type of modern SSRI, is approved by the FDA in patients older than 8, while escitalopram is approved in patients above the age of 12 (28). No other SSRIs have been approved to treat MDD in adolescents; however, fluvoxamine and sertraline have been approved to treat OCD in teenagers (29). While these age restrictions allow many adolescents to be treated with SSRIs, SSRIs are only prescribed by medical professionals as a last-resort in extreme circumstances. SSRIs, apart from fluoxetine and escitalopram, are not approved for usage in adolescents due to the heightened risks of self-harm and increased suicidal ideation in adolescents using SSRIs (24). Many concerns regarding impacts on brain development also surround the SSRI drug class. Little testing has been conducted regarding the effects of SSRIs on brain development in adolescents, however, a recent study that clinically exposed developing rodents to SSRI antidepressants found conclusive evidence of brain alterations. The study outlines that rodents who were exposed to SSRIs experienced abnormal raphae circuitry, a neurological system responsible for releasing serotonin to other parts of the brain, and changes in cortical network function (30). A further study that reviewed fMRI images in adolescents that were exposed to SSRIs found that this exposure increased the size of the right ventrolateral prefrontal cortex and the hippocampus (31). In general, little is known about the physical effects that SSRIs can have on the developing brain, and further research is needed to understand the possible consequences of early antidepressant usage. More specifically, research into SSRI exposure in areas such as the prefrontal cortex, that mature towards the end of the neurological development spectrum (32), would significantly improve the scientific understanding of the implications that SSRIs can have towards the developing brain. Most age restrictions associated with SSRIs and other types of antidepressants seek to prevent premature usage that could result in unknown and under-researched side effects.
Figure 2. Brain development from age 9 to 25. Repurposed from PNAS. 10.1073/pnas.0402680101
Mechanism of Action and Metabolism
Selective serotonin reuptake inhibitors treat depressive symptoms through a complex process. This section will outline the step by step actions performed throughout the body to ingest, utilize, and metabolize SSRIs. After being taken orally, SSRIs pass through the stomach and into the small intestine where they are absorbed by the bloodstream. Once in the bloodstream, SSRIs cross the blood-brain barrier through facilitated diffusion, where they then begin to affect neuronal function (33). In brief, SSRI antidepressants regulate the movement and expression of serotonin within the brain. Each SSRI antidepressant has varying effects on serotonin, however, all SSRIs affect many of the same neurological molecules, transmitters, and transporters. In terms of metabolic breakdown, nearly all SSRIs are metabolized through hepatic oxidative metabolism in the liver, which entails enzymatic degradation by members of the cytochrome P450 enzymatic family.
Serotonin is the target of SSRI action. Neurotransmitters such as serotonin act as chemical messengers throughout the nervous system. In the form of electrical impulses called action potentials, neurotransmitters transmit a neurological message from the presynaptic terminal of one nerve, across the synapse, to the postsynaptic receptors on the next nerve. These chemical messages stimulate bodily functions, including movement, sensation, and cognition (34). Serotonin’s specific effect on a postsynaptic target, and resulting physiological effects, depends on the receptor it binds to. There are three main types of cellular responses once a neurotransmitter binds to a receptor. These include excitatory responses that continue the transmission of neurological information, inhibitory responses that prevent the propagation of further signals, and modulatory responses in which serotonin can influence the levels of other neurotransmitters in the central nervous system. The current scientific understanding of serotonin holds that the neurotransmitter is associated with seven total postsynaptic receptors. 5-HT3 is the only ionotropic receptor of serotonin, and is classified as excitatory, facilitating the depolarization of postsynaptic neurons through the manipulation of K+, Na+, and Ca++ channels (35). 5-HT4, 5-HT6, and 5-HT7 receptors are metabotropic and are all linked to the activation of adenylyl cyclase (36). Classified as excitatory, these receptors increase neuronal stimulation. 5-HT1 and 5-HT5 receptors are also metabotropic but classified as inhibitory, lowering the likelihood of a postsynaptic action potential (36). Depending on which 5-HT receptor a serotonin neurotransmitter binds, there can be varying effects on postsynaptic neurotransmission, and consequently, bodily function.
| Receptor | Human Locus | Distribution | Effector Mechanism |
| 5-HT1A | 5q11.2-13 | Hippocampus, amygdala, septum, entorhinal cortex, hypothalamus, raphae nuclei | Inhibition of adenylyl cyclase, opening of K+ channels |
| 5-HT1Dα | 1p34.3-36.3 | Not distinguishable from 5-HT1Dβ | Inhibition of adenylyl cyclase |
| 5-HT1Dβ | 6q13 | Substantia nigra, basal ganglia, superior colliculus | Inhibition of adenylyl cyclase |
| 5-HT1E | ? | ? | Inhibition of adenylyl cyclase |
| 5-HT1F | 3p11 | Cerebral cortex, striatum, hippocampus, olfactory bulb | Inhibition of adenylyl cyclase |
| 5-HT2A | 13q14-21 | Claustrum, cerebral cortex, olfactory tubercle, striatum, nucleus accumbens | Stimulation of phosphoinositide-specific Phospholipase C, closing of K+ channels |
| 5-HT2B | 2q36.3-37.1 | ? | Stimulation of phosphoinositide-specific Phospholipase C |
| 5-HT2C | Xq24 | Choroid plexus, globus pallidus, cerebral cortex, hypothalamus, septum, substantia nigra, spinal cord | Stimulation of phosphoinositide-specific Phospholipase C |
| 5-HT3 | ? | Hippocampus, entorhinal cortex, amygdala, nucleus accumbens, solitary tract nerve, trigeminal nerve, motor nucleus of the dorsal vagal nerve, area postrema, spinal cord | Ligand-gated cation channel |
| 5-HT4 | ? | Hippocampus, olfactory tubercle, substantia nigra | Stimulation of adenylyl cyclase |
| 5-HT5A | 7q36 | ? | Inhibition of adenylyl cyclase |
| 5-HT5B | 2q11-13 | ? | ? |
| 5-HT6 | ? | ? | Stimulation of adenylyl cyclase |
| 5-HT7 | 10q23.3-24.3 | Cerebral cortex, septum, thalamus, hypothalamus, amygdala, superior colliculus | Stimulation of adenylyl cyclase |
Table 3. Serotonin Receptors Present in the Central Nervous System and their respective functions. Repurposed from Basic Neurochemistry: Molecular, Cellular and Medical Aspects. 6th edition. https://www.ncbi.nlm.nih.gov/books/NBK28234/
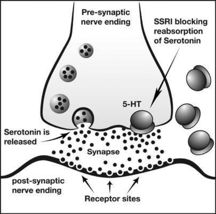
Although it plays a critical role in brain activity, Serotonin is predominantly located in the gastrointestinal tract. In actuality, only 10 percent of the body’s serotonin is found throughout the central nervous system (37). However, as a chemical messenger, serotonin is essential to numerous bodily processes. Serotonin affects many behavioral and neuropsychological processes including mood, anger, appetite, memory, and attention (38). Serotonin is vital to mental health and emotional well-being, and when the body lacks sufficient amounts of serotonin, serious problems can arise. The development of SSRIs in the 1970s was based on the serotonin hypothesis of depression, in which proponents of the theory believed that a lack of serotonin in the brain caused depressive symptoms. This foundational belief was central to the development of SSRIs, a type of antidepressant that seeks to artificially increase the levels of serotonin throughout the brain by preventing serotonin reuptake. Serotonin reuptake, a mechanism in which excess serotonin is reabsorbed by the neuron from which it was released, is a key process in regulating serotonin levels in the central nervous system. As serotonin is no longer in the synapse, it cannot bind to postsynaptic receptors and transport information. The serotonin transporter (SERT) is the transport responsible for serotonin reuptake, undergoing conformational changes in shape to allow for one serotonin molecule to exit the synaptic cleft during each cycle. Serotonin neurotransmitters that have undergone reuptake will be reabsorbed into the presynaptic terminals. SSRIs inhibit the serotonin transporter, delaying neurons from reabsorbing serotonin and allowing the serotonin to stimulate postsynaptic receptors for an extended period (39).
Figure 3. Schematic diagram showing mechanism of action of SSRIs. These agents block the reuptake of serotonin at the presynaptic membrane, thus increasing its concentration at the postsynaptic nerve terminal membrane. Repurposed from The Journal of Perinatology. 10.1038/sj.jp.7211352.
This excess excitability of postsynaptic receptors directly elevates mood and combats feelings of sadness and despair that usually accompany depression. Unlike other forms of antidepressants, SSRIs solely target serotonin and have little effect on the bodily levels of other neurotransmitters, such as dopamine and norepinephrine. Effects on the neurotransmitter histamine are described later. While all SSRIs use a similar method of action, there are subtle differences between the mechanisms of action of each drug: each SSRI differs in their potencies at blocking serotonin reuptake (40). With varying levels of inhibition, some SSRIs maintain higher concentrations of serotonin in the synapse.
When SSRIs enter the liver before circulation or reenter the liver any time after reaching the central nervous system, they begin to be metabolized. SSRIs vary with regard to the duration of their metabolism, a period that can mostly be correlated with the half-lives of each specific SSRI. The complete clearance, the time it takes for the drug to completely exit the body, of most SSRIs is around six days. Fluoxetine takes the longest to metabolize of any SSRI, leaving the body completely after twenty-five days (41). All SSRIs are metabolized in the liver by the cytochrome P450 system. The Cytochrome P450 (CYP) system, which is composed of hemeprotein complexes, is responsible for catalyzing a diverse range of oxidative reactions throughout the body (42). The Cytochrome P450 system is a common mechanism for the metabolism of various drugs. Twelve enzymes belonging to the CYP1, 2, and 3 families are responsible for the biotransformation of many foreign substances, including around 75% of all drugs in clinical use (43). SSRIs are metabolized through two distinct phases of Cytochrome P450 biotransformation. Phase I reactions introduce a reactive or polar group, to the SSRIs. In this phase, known as oxidation, CYP enzymes catalyze the removal of electrons from the SSRIs to convert the drug to a more water-soluble form. During Phase II, this new version of the drug is then conjugated to form a polar compound in a reaction catalyzed by transferase enzymes, enzymes that transfer specific functional groups from one molecule to another (44). Further processing can sometimes occur, however, this two-phase process generates a more polar and inactivated version of an SSRI that can be eliminated from the body through urination or excretion. It is important to note that most SSRIs require more than one CYP enzyme to be completely metabolized (45).
The Cytochrome P450 complex can be actively inhibited or induced by various molecules, including those that it metabolizes. Some selective serotonin reuptake inhibitors inhibit the CYP2D6 protein of the Cytochrome P450 (46), decreasing the production and enzymatic activity of the complex. On top of CYP2D6, fluoxetine significantly inhibits CYP2C9, CYP2C19, and CYP3A4 (47). Another SSRI, fluvoxamine, also inhibits CYP1A2, CYP2C19, CYP2C9, and CYP3A4 (46). All other SSRIs inhibit a varying combination of CYP complexes to a lesser extent. An important property of SSRIs is that they can both inhibit and be metabolized by the same enzyme, or inhibit an enzyme and be metabolized by another (48). This complex and nuanced system of CYP mediated metabolism is essential to the elimination of SSRIs from the body. The many enzymes that break down SSRIs also increase the potential for harmful drug interactions.
| Antidepressant | Major elimination pathway | Other elimination pathways | Inhibitory effect on CYP isoenzyme |
| Citalopram | CYP2C19 | CYP3A4, CYP2D6 | CYP1A2, CYP2B6, CYP2C19, CYP2D6 |
| Escitalopram | CYP2C19 | CYP3A4, CYP2D6 | CYP2D6, CYP2C9 |
| Fluoxetine (active metabolite norfluoxetine) | CYP2D6 | CYP2C9, CYP2C19, CYP3A4 | CYP2D6, CYP2C9, CYP2C19, CYP3A4, CYP1A2 |
| Fluvoxamine | CYP1A2, CYP2D6 | CYP1A2, CYP2C19, CYP2C9, CYP3A4, CYP2D6 | |
| Paroxetine | CYP2D6 | CYP3A4 | CYP2D6, CYP1A2, CYP2C9, CYP2C19, CYP3A4 |
| Sertraline | CYP2B6 | CYP2C19, CYP2C9, CYP3A4, CYP2D6 | CYP2D6, CYP1A2, CYP2C9, CYP2C19, CYP3A4 |
Table 4. Antidepressants and CYP enzymes. Repurposed from ResearchGate under Creative Commons Attribution-NonCommercial 4.0 International. 10.2147/NDT.S157708
Understanding the parts of the Cytochrome P450 system that are involved in the metabolism of SSRIs is important to understanding the contradictions associated with the drug class. The CYP450 system plays a significant role in metabolizing numerous drugs, including SSRIs, leading to opportunities for drug interactions. As a result, there are a multitude of risks associated with SSRIs when combined with other prescription and recreational drugs. Other pharmaceutical drugs that can interact with SSRIs include non-steroid anti-inflammatory drugs, antiplatelets, theophylline, clozapine, pimozide, lithium, triptans, and other antidepressants (49). These drugs utilize similar mechanisms for elimination as SSRIs, leading to increased chances of interaction. Alcohol and coffee are cited as other products that may cause unwanted interactions with SSRI usage (49). Drug interactions can delay, decrease, or enhance the absorption of either drug and cause adverse effects.
Efficacy of SSRIs
The serotonin theory of depression has been the backbone of the scientific community’s understanding of depression for decades, shaping modern antidepressants and treatments. At its core, the serotonin theory of depression attributes depressive symptoms to a depletion of serotonin within the brain. Once widely accepted, recent studies have called into question the validity of the principle. Ideas about the plausibility of the serotonin theory of depression have split the scientific community.
A recent review from Moncrieff et al critically analyzed the serotonin theory of depression (46). The goal of this comprehensive meta review was to evaluate evidence from previous works in order to come to a conclusion about whether depression correlates with lowered serotonin concentration or activity in the central nervous system. Using reports from seventy-five sources, the review concluded that there is insufficient evidence to propose that depression is associated with, or caused by, lower serotonin concentrations or activity (50). Prior to this review, many science researchers had long doubted the validity of the serotonin theory of depression. These findings did not surprise most members of the field, who had already assumed that the serotonin theory of depression was far too simplistic to explain a complex condition like MDD.
Although the serotonin theory of depression has become controversial in recent years, most psychiatrists do not believe that ending the usage of SSRIs is necessary. A consensus from other psychological researchers is that current clients should not discontinue the usage of SSRIs without proper consultation, as there are many side effects associated with SSRI discontinuation (51). Dr. Michael Bloomfield, head of the translational psychiatry research group at University College London, maintains that there is consistent evidence that antidepressant medicines can still be helpful in the treatment of depression and even possibly life-saving (52). Overall, many scientists continue to promote the usage of SSRIs to patients, as they have been proven to be effective at mitigating some aspects of depressive symptoms.
While a majority of scientists have accepted the conclusion proposed by Moncrieff et al, some scientists point out errors in the way the study was conducted as evidence to continue to support the serotonin theory of depression. This controversy was ignited following the publication of a review by Jauhar et al. This counter-review concludes that Moncrief’s review was conducted using inconsistent methodology and with substantial bias and manipulation of results (53). The second review promotes that a more reasonable conclusion of the data gathered by Moncrief’s team is that tryptophan depletion and decreased plasma tryptophan in individuals with depression indicate a role for 5-HT in those vulnerable to or suffering from MDD, and that molecular imaging suggests the system is perturbed (52). The importance of serotonin in depression is still a topic of debate and an area that requires further exploration, analysis, and funding. One aspect of SSRI function that scientists are more certain about is the effects of SSRIs on other biogenic amines. Histamine, a neurotransmitter with similar characteristics to serotonin, is affected by SSRI exposure in the form of reuptake inhibition (54). Researchers at the Imperial College London confirmed that histamine directly dampens serotonin release in the brain (55). With this finding, scientists concluded that the increased levels of neuronal histamine following SSRI treatment lowered the presence of serotonin in the brain. Scientists are now focusing on the implications of histamine, a neurotransmitter usually associated with allergies and immune responses, on SSRIs and its role in depression.
The efficacy of SSRIs in adolescents is an under-researched area of medicine, yet, various studies indicate that fluoxetine has been observed to reduce depressive symptoms in patients under the age of 18 (56). A meta-review of fluoxetine concludes that the efficacy of fluoxetine is well established in the treatment of major depressive disorder (57). This declaration follows the analysis of numerous clinical controlled trials involving patients with major depressive disorders (58). However, a separate study conducted by Hetrick et al puts forth that other SSRIs can actually have detrimental effects on adolescents. The study observed that of the young patients who were exposed to various SSRIs, there was a marked increased risk of suicidal ideation across participants (58). A further meta-review from Garland et al emphasizes that thus far, no SSRI has consistently demonstrated positive results for depression in pre-pubertal children (59). This study directly contradicts the previous notions of fluoxetine efficacy. The current scientific understanding regarding the efficacy of SSRIs in adolescents is that all SSRIs, with the exception of fluoxetine, have little to no effect on the depressive symptoms of the age group, and that fluoxetine may only slightly decrease depressive symptoms.
Possible Side Effects in Adolescents
Another critical factor of antidepressant usage in adolescents pertains to possible side effects. Weighing the possible risks and side effects associated with a drug must be considered before usage. While many recipients of antidepressants are keen on finding the drug that brings the fewest unwanted side effects, ultimately there is no singular antidepressant that guarantees minimal side effects. It is also important to note that reactions to antidepressants vary across individuals. Currently, the SSRI antidepressant class is regarded as the safest for general use, as it has the fewest major side effects of any antidepressant class.
One review outlines suicide-related behaviors, switching to mania, and serotonin syndrome as possible side effects of SSRI usage (60). A different review outlines that the first three months of SSRI usage see the greatest risk of suicidal ideation and attempt (61). Another review from Lagerberg et al found that SSRI-treatment did not increase the risk of suicidal ideation in adolescents or adults (62). Risk of suicidal behavior in adolescents is another crucial area of SSRIs that requires further analysis in order to understand the full scope of risks associated with early SSRI usage. The other previously mentioned symptom, serotonin syndrome, is a condition caused by a medically induced buildup of serotonin in the body. Symptoms commonly include diarrhea, seizures, muscle rigidity, and in extreme cases, death. A separate overview from the Child Mind Institute warns that other minor side effects of SSRI use can include headache, nausea, stomachaches, drowsiness, dry mouth, insomnia, agitation, activation, dizziness, reduced sexual desire, and an impact on appetite (63). The harmful, and possibly fatal, side effects of SSRIs must be disclosed to adolescents and carefully considered before usage.
This extensive list of side effects associated with SSRIs, but also general antidepressants, brings into question other treatment options for MDD that may produce fewer alternative effects. Some comparative treatments for Major Depressive Disorder include: cognitive behavioral counseling (CBT), a type of therapy that helps one understand thoughts and behavior, interpersonal therapy (IPT), which focuses on relationships with others, and exercise. A meta review regarding the efficacy of cognitive behavioral therapy in patients with mood disorders found that CBT is equally as effective as traditional medications for mitigating depressive symptoms in patients with mild depression (64). However, one clinical trial proposes that, in terms of patients with severe depression, cognitive behavioral therapy has a similar efficacy to that of a placebo (65). A separate meta review pertaining to interpersonal therapy asserts that pharmacotherapy was more effective than IPT at mitigating depression (66). This is not to say that IPT is ineffective, as IPT treatment on patients with subthreshold depression significantly prevented the onset of major depression (67). Regular IPT treatment has also been observed to significantly reduce relapse rates (67). Finally, a meta review by Recchia et al found that exercise had similar efficacy at mitigating MDD as antidepressants (68). Many alternative treatments to antidepressants show promising results, and require further analysis to completely evaluate their merit. This review analyzes antidepressants, specifically SSRIs, as they continue to be the most commonly prescribed treatment for MDD.
A combination of the aforementioned treatment forms, including CBT, IPT, and antidepressants, has also shown promise for mitigating depression in all populations. A meta analysis by Whiston et al found that a combined treatment of cognitive behavioral therapy and interpersonal therapy proved to be more effective than solely IPT (69). A meta review from the National Institute for Health and Care Research found that a combined use of selective serotonin reuptake inhibitors and cognitive behavioral therapy proved to be more effective than either treatment alone. Individuals exposed to a combined treatment were 27% more likely to see a reduction of depressive symptoms by half than those receiving psychotherapy alone, while 25% more likely to see this same decrease when compared to those receiving only drug treatment (70).
The Unknowns about SSRI Responses in Adolescents
The recommended treatment pathway for adolescents experiencing MDD is a non-drug approach in the form of cognitive behavioral or interpersonal therapy. This sequential treatment is the same for all age groups, however, specific pharmacotherapy treatments differ between adults and adolescents. In cases of severe onset of depression, antidepressants, most predominantly in the form of SSRIs, are used to treat patients. Treatment for adolescents is less standardized, as less research has been conducted surrounding the effects and safety of SSRIs in adolescents. Historically, certain patient groups, including adolescents, have been excluded from clinical trials because scientists regarded them as vulnerable populations (71). With a rise of antidepressant use by approximately half a percent within the adolescent population in the United States (72), focus has shifted toward the lack of safety data associated with SSRIs in this group. The consequence of developing antidepressants that have historically been curated for only adult populations is that modern SSRIs have lower efficacy rates in adolescents. Treating adolescent depression requires the development of new treatments that solely focus on the adolescent population, meaning that they may not provide benefits to adult populations (27).
A meta review of adolescent depression highlights withdrawal symptoms, following unexpected pauses in SSRI use, as another area of adolescent SSRI use that requires further research. The review emphasizes that a systematic study is required to identify withdrawal symptomatology and better understand the long-term effects of SSRI treatment on depressive disorders (73). Withdrawal symptoms in adults have been more extensively studied. One review outlines dizziness, light-headedness, insomnia, fatigue, anxiety/agitation, nausea, headache, and sensory disturbance as common symptoms of adult withdrawal (74). While one source (75) currently suggests that withdrawal symptoms may be less severe in adolescents, further testing must be performed to support this assumption.
Other areas in need of further research that were previously outlined in this review include: suicidal behavior in adolescents, the role of serotonin in adolescent depression, and physical effects on the adolescent brain. These areas are critical to an improved understanding of adolescent depression and the benefits and consequences that arise during SSRI treatment.
Longitudinal Studies
The long term effects of prolonged SSRI use in adolescents are another gap in scientific knowledge. With SSRI treatment in adolescents beginning only decades ago, many long-term risks associated with the treatment have not been properly analyzed. One review outlines sexual dysfunction, weight gain, and sleep disturbance as known long-term effects of SSRI usage in adults (76). Adolescent rats that were exposed to fluoxetine experienced long-lasting decreases in behavioral reactivity to forced swimming stress and enhanced sensitivity to sucrose and to anxiety-eliciting situations in adulthood. These behavioral changes indicate that early SSRI use may lead to substantial changes in the developing nervous system (79). On the contrary, antidepressants have positive effects on functioning, namely social interactions and cognitive developments, when used consistently by children and adolescents with MDD (77). Early effective treatment for MDD also reduces the risk of long-term negative outcomes and has a sustained positive effect on functioning and life satisfaction into adulthood (78).
Overall, there continues to be a general lack of literature pertaining to the longitudinal effects of antidepressants in adolescents. Further clinical studies must be conducted in order to better inform adolescents who are considering SSRI treatment.
Discussion
This review highlights the current scientific understanding regarding selective serotonin reuptake inhibitors. Collectively, there is a lack of sufficient data to make sound decisions about the use of SSRIs. Although some reviews (80/81) propose that the improvements associated with certain SSRIs outweigh the possible risks in adolescents, others may find that there is generally insufficient data regarding SSRI effects in adolescents, and specifically, the long-term effects of SSRI use and effects on brain maturation, to confidently make this claim. To reiterate, the current scientific understanding surrounding SSRIs upholds that specific SSRIs, such as fluoxetine, can have positive impacts on adolescents diagnosed with MDD. However, it is also acknowledged that SSRIs can have extremely negative side effects, namely suicidal ideation and developmental impairment of the brain. Studies conducted by found Hazell and Christiansen et al (60/61) found correlation between SSRI exposure in adolescents and an increased risk of completed and attempted suicide. However, predicting an individual’s response to a pharmaceutical drug is not currently possible, meaning that scientists cannot predict with absolute certainty whether an individual may experience these side effects. Additionally, researchers currently do not understand the full scope of the effects that SSRIs have on a developing brain, although specific brain alterations have been clinically observed. Another important aspect of SSRIs is that they have been observed to exacerbate other psychological conditions, such as bipolar disorder and mania, and lead to contradictions with other drugs.
Although there are many possible consequences associated with SSRI usage, SSRIs, specifically Fluoxetine, can be critical to improving the condition of adolescents suffering from depression. However, not all patients respond positively to the drug. If this is the case, Escitalopram, another type of SSRI, is the next choice for medical professionals. Research indicates that around half of depressed youth who do not respond to a first SSRI will respond to a second one (82). No other current treatment forms, including cognitive behavioral therapy and interpersonal psychotherapy, have the possibility of mitigating adolescent depression to the same extent that specific SSRIs do. While these non-medicated treatment forms for adolescent depression do offer benefits to patients, namely decreased negative feelings and increased emotional control, they do not address the underlying neurological systems that are at the root of the condition. However, using SSRIs is ultimately up to the discretion of adolescents and their families. This review provides adolescents with all viewpoints of SSRI usage to allow them to make more informed decisions about their mental health.
Acknowledgements
Dr. Dounas-Frazer, Dr. Wardlaw, Dr. McConnachie for providing review and feedback.
Literature Cited
- 1. Horwitz, A. V. (2010, March). How an age of anxiety became an age of depression. The Milbank quarterly. 10.1111/j.1468-0009.2010.00591.x
- 2. Chand, S. P., & Arif, H. (n.d.). Depression - statpearls - NCBI bookshelf. Depression. https://www.ncbi.nlm.nih.gov/books/NBK430847/
- 3. Staff, C. (2023, May 26). Sadness and depression. Centers for Disease Control and Prevention. https://www.cdc.gov/howrightnow/emotion/sadness/index.html#:~:text=But%20usually%2C%20the%20sadness%20goes,often%20or%20all%20the%20time
- 4. professional, C. C. medical. (n.d.-a). Depression: Causes, symptoms, types & treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/9290-depression
- 5. World Health Organization. (n.d.). Covid-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide#:~:text=COVID%2D19%20pandemic%20triggers%2025,of%20anxiety%20and%20depression%20worldwide
- 6. Liu et al. (2019, August 10). Changes in the global burden of depression from 1990 to 2017: Findings from the global burden of disease study. Journal of Psychiatric Research. 10.1016/j.jpsychires.2019.08.002
- 7. McPhillips, D. (2023, May 17). More than 1 in 6 adults have depression as rates rise to record levels in the US, survey finds. CNN. https://www.cnn.com/2023/05/17/health/depression-rates-gallup/index.html
- 8. LaMotte, S. (2021, May 3). Americans are not getting the mental health treatment they need, report says. CNN. https://www.cnn.com/2021/05/03/health/mental-health-treatment-us-wellness/index.html
- 9. Rao, U., & Chen, L.-A. (2009). Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues in clinical neuroscience. 10.31887/DCNS.2009.11.1/urao
- 10. Table 1, diagnostic criteria for primary DSM-IV depression disorders in ... Screening for Child and Adolescent Depression In Primary Care Settings: A Systematic Evidence Review for the U.S. Preventive Services Task Force. (n.d.). https://www.ncbi.nlm.nih.gov/sites/books/NBK35129/table/A58167/
- 11. Osorio, E. K., & Hyde, E. (2023, October 30). The rise of anxiety and depression among young adults in the United States. Ballard Brief. https://ballardbrief.byu.edu/issue-briefs/the-rise-of-anxiety-and-depression-among-young-adults-in-the-united-states
- 12. Miller, C. (2023, October 30). Does social media use cause depression?. Child Mind Institute. https://childmind.org/article/is-social-media-use-causing-depression/
- 13. Zhang et al. (n.d.). Associations between academic stress and depressive symptoms mediated by anxiety symptoms and hopelessness among Chinese college students. Psychology research and behavior management. 10.2147/PRBM.S353778
- 14. Thapar, A., Collishaw, S., Pine, D. S., & Thapar, A. K. (2012, March 17). Depression in adolescence. Lancet (London, England). 10.1016/S0140-6736(11)60871-4
- 15. Rice, F. (2010, September 20). Genetics of childhood and adolescent depression: Insights into etiological heterogeneity and challenges for future genomic research. Genome medicine. 10.1186/gm189
- 16. Marken, P. A., & Munro, J. S. (2000, December). Selecting a selective serotonin reuptake inhibitor: Clinically important distinguishing features. Primary care companion to the Journal of clinical psychiatry. 10.4088/pcc.v02n0602
- 17. Sheffler, Z. M. (2023, May 26). Antidepressants. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK538182/
- 18. Nahas, R., & Sheikh, O. (2011, June). Complementary and alternative medicine for the treatment of major depressive disorder. Canadian family physician Medecin de famille canadien. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3114664/
- 19. Wilson, S., & Dumornay, N. M. (2022, March). Rising rates of adolescent depression in the United States: Challenges and opportunities in the 2020s. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 10.1016/j.jadohealth.2021.12.003
- 20. Collishaw, S. (n.d.). Annual research review: Secular trends in child and Adolescent Mental Health. Journal of child psychology and psychiatry, and allied disciplines. 10.1111/jcpp.12372
- 21. Depression on the rise in adolescents during COVID-19 pandemic. CHOP Research Institute. (n.d.). https://www.research.chop.edu/cornerstone-blog/depression-on-the-rise-in-adolescents-during-covid-19-pandemic
- 22. Zhang, F.-F., Peng, W., Sweeney, J. A., Jia, Z.-Y., & Gong, Q.-Y. (2018, November). Brain structure alterations in depression: Psychoradiological evidence. CNS neuroscience & therapeutics. 10.1111/cns.12835
- 23. Straub, J., Brown, R., Malejko, K., Bonenberger, M., Grön, G., Plener, P. L., & Abler, B. (2019, July 1). Adolescent depression and brain development: Evidence from Voxel-based morphometry. Journal of psychiatry & neuroscience : JPN. 10.1503/jpn.170233
- 24. Orchard, F., Pass, L., Marshall, T., & Reynolds, S. (n.d.). Clinical characteristics of adolescents referred for treatment of depressive disorders. Child and adolescent mental health. 10.1111/camh.12178
- 25. Rao, U., & Chen, L.-A. (2009a). Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues in clinical neuroscience. 10.31887/DCNS.2009.11.1/urao
- 26. Rice et al. (2018, September 11). Adolescent and adult differences in major depression symptom profiles. Journal of Affective Disorders. 10.1016/j.jad.2018.09.015
- 27. Bylund, D. B., & Reed, A. L. (2007, October). Childhood and adolescent depression: Why do children and adults respond differently to antidepressant drugs?. Neurochemistry international. 10.1016/j.neuint.2007.06.025
- 28. Yan, T., & Goldman, R. D. (2019, August). Time-to-effect of fluoxetine in children with depression. Canadian family physician Medecin de famille canadien. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6693597/
- 29. Mayo Foundation for Medical Education and Research. (2022, March 19). What to know about antidepressants for kids and teens. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/teen-depression/in-depth/antidepressants/art-20047502
- 30. Simpson et al. (2011, September 30). Perinatal antidepressant exposure alters cortical network ... - PNAS. Perinatal antidepressant exposure alters cortical network function in rodents. 10.1073/pnas.1109353108
- 31. Gaffrey, M. S., Shenoy, R., & Luby, J. L. (2011, October). Effects of stimulants and ssris on brain function in children: Emerging clues from fmri studies. Child & adolescent psychopharmacology news. 10.1521/capn.2011.16.5.3
- 32. Konrad, K., Firk, C., & Uhlhaas, P. J. (2013, June 21). Brain development during adolescence: Neuroscientific Insights into this developmental period. Deutsches Arzteblatt international. 10.3238/arztebl.2013.0425
- 33. Warren, J. B. (2012, January). Antidepressants and the developing nervous system. British journal of clinical pharmacology. 10.1111/j.1365-2125.2011.04107.x
- 34. professional, C. C. medical. (n.d.). Neurotransmitters: What they are, functions & types. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/22513-neurotransmitters
- 35. 5-HT3 receptor. 5-HT3 Receptor - an overview | ScienceDirect Topics. (n.d.). https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/5-ht3-receptor#:~:text=5%2DHT3%20receptors%20are,Hannon%20and%20Hoyer%2C%202008
- 36. Frazer, A., & Hensler, J. G. (n.d.). Serotonin receptors - basic neurochemistry - NCBI bookshelf. Serotonin Receptors. https://www.ncbi.nlm.nih.gov/books/NBK28234/
- 37. professional, C. C. medical. (n.d.-b). Serotonin: What is it, Function & Levels. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/22572-serotonin
- 38. Berger, M., Gray, J. A., & Roth, B. L. (2009). The expanded biology of Serotonin. Annual review of medicine. 10.1146/annurev.med.60.042307.110802
- 39. Chu, A., & Wadhaw, R. (n.d.). Selective serotonin reuptake inhibitors - statpearls - NCBI bookshelf. Selective Serotonin Reuptake Inhibitors. https://www.ncbi.nlm.nih.gov/books/NBK554406/
- 40. Mayo Foundation for Medical Education and Research. (2019, September 17). The most commonly prescribed type of antidepressant. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825
- 41. Going off antidepressants - harvard health publishing. Harvard Health. (2022, May 15). https://www.health.harvard.edu/diseases-and-conditions/going-off-antidepressants
- 42. ScienceDirect. (n.d.). Cytochrome P450. Cytochrome P450 - an overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/medicine-and-dentistry/cytochrome-p450#:~:text=Cytochrome%20P450%20monooxygenases%20catalyze%20the,toxicants%20to%20more%20reactive%20intermediates
- 43. Zanger, U. M., & Schwab, M. (2013, January 16). Cytochrome P450 enzymes in drug metabolism: Regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacology & Therapeutics. 10.1016/j.pharmthera.2012.12.007
- 44. Zhao, M., Ma, J., Li, M., Zhang, Y., Jiang, B., Zhao, X., Huai, C., Shen, L., Zhang, N., He, L., & Qin, S. (2021, November 26). Cytochrome P450 enzymes and drug metabolism in humans. International journal of molecular sciences. 10.3390/ijms222312808
- 45. Thakur, M., Grossman, I., McCrory, D. C., Orlando, L. A., Steffens, D. C., Cline, K. E., Gray, R. N., Farmer, J., Dejesus, G., O’Brien, C., Samsa, G., Goldstein, D. B., & Matchar, D. B. (2007). Review of evidence for genetic testing for CYP450 polymorphisms in management of patients with nonpsychotic depression with selective serotonin reuptake inhibitors. Nature News. 10.1097/GIM.0b013e31815bf98f
- 46. Brøsen, K. (n.d.). Differences in interactions of ssris. International clinical psychopharmacology. 10.1097/00004850-199809005-00009
- 47. Brown, C. H. (2008, January 23). Overview of drug–drug interactions with ssris. U.S. Pharmacist – The Leading Journal in Pharmacy. https://www.uspharmacist.com/article/overview-of-drugdrug-interactions-with-ssris
- 48. Lynch, T., & Price, A. (2007, August 1). The effect of cytochrome P450 metabolism on drug response, interactions, and adverse effects. American Family Physician. https://www.aafp.org/pubs/afp/issues/2007/0801/p391.html
- 49. NHS. (n.d.). Cautions - Selective Serotonin Reuptake Inhibitors (SSRIs). NHS choices. https://www.nhs.uk/mental-health/talking-therapies-medicine-treatments/medicines-and-psychiatry/ssri-antidepressants/considerations/#:~:text=Some%20of%20the%20medicines%20that,low%2Ddose%20aspirin%20and%20clopidogrel
- 50. Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2022, July 20). The serotonin theory of depression: A Systematic Umbrella Review of the evidence. Nature News. 10.1038/s41380-022-01661-0
- 51. Borgogna, N. C., & Aita, S. L. (2022, November 3). Is the serotonin hypothesis dead? if so, how will clinical psychology respond?. Frontiers in psychology. 10.3389/fpsyg.2022.1027375
- 52. MacKenzie, R. J. (n.d.). A popular theory about depression wasn’t “debunked” by a new review. Neuroscience from Technology Networks. https://www.technologynetworks.com/neuroscience/articles/a-popular-theory-of-depression-wasnt-debunked-by-a-new-review-it-got-debunked-years-ago-363986
- 53. Jauhar, S., Arnone, D., Baldwin, D. S., Bloomfield, M., Browning, M., Cleare, A. J., Corlett, P., Deakin, J. F. W., Erritzoe, D., Fu, C., Fusar-Poli, P., Goodwin, G. M., Hayes, J., Howard, R., Howes, O. D., Juruena, M. F., Lam, R. W., Lawrie, S. M., McAllister-Williams, H., … Cowen, P. J. (2023, June 16). A leaky umbrella has little value: Evidence clearly indicates the serotonin system is implicated in depression. Nature News. 10.1038/s41380-023-02095-y
- 54. Hersey, M., Samaranayake, S., Berger, S. N., Tavakoli, N., Mena, S., Nijhout, H. F., Reed, M. C., Best, J., Blakely, R. D., Reagan, L. P., & Hashemi, P. (2021, July 28). Inflammation-induced histamine impairs the capacity of escitalopram to increase hippocampal extracellular serotonin. Journal of Neuroscience. 10.1523/JNEUROSCI.2618-20.2021
- 55. Brogan, C. (2021, August 17). Histamine could be a key player in depression, according to study in mice: Imperial News: Imperial College London. Imperial News. https://www.imperial.ac.uk/news/228353/histamine-could-player-depression-according-study/
- 56. Hetrick, S. E., Merry, S. N., McKenzie, J., Sindahl, P., & Proctor, M. (2007, July 18). Selective serotonin reuptake inhibitors (ssris) for depressive disorders in children and adolescents - hetrick, SE - 2007: Cochrane Library. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD004851.pub2
- 57. Gourion, D., Perrin, E., & Quintin, P. (n.d.). [fluoxetine: An update of its use in major depressive disorder in adults]. L’Encephale. 10.1016/s0013-7006(04)95453-x
- 58. Hetrick et al. (n.d.). Newer generation antidepressants for depressive disorders in children and adolescents. The Cochrane database of systematic reviews. 10.1002/14651858.CD004851.pub3
- 59. Jane Garland, E., Kutcher, S., Virani, A., & Elbe, D. (2016, February 1). Update on the use of ssris and snris with children and adolescents in clinical practice. Journal of the Canadian Academy of Child and Adolescent Psychiatry = Journal de l’Academie canadienne de psychiatrie de l’enfant et de l’adolescent. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4791100/
- 60. Hazell, P. (2022, April 1). Antidepressants in adolescence. Australian prescriber. 10.18773/austprescr.2022.011
- 61. Christiansen et al. (n.d.). SSRIs and risk of suicide attempts in young people - a Danish observational register-based historical cohort study, using propensity score. Nordic journal of psychiatry. 10.3109/08039488.2015.1065291
- 62. Lagerberg et al. (n.d.). Selective serotonin reuptake inhibitors and suicidal behaviour: A population-based Cohort Study. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 10.1038/s41386-021-01179-z
- 63. Medication for kids with depression. Child Mind Institute. (2023, July 27). https://childmind.org/article/medication-for-kids-with-depression/#side-effects-of-ssris-and-snris
- 64. Driessen, E., & Hollon, S. D. (2010, September). Cognitive behavioral therapy for mood disorders: Efficacy, moderators and mediators. The Psychiatric clinics of North America. 10.1016/j.psc.2010.04.005
- 65. Elkin et al. (1990, November). National Institute of Mental Health Treatment of Depression Collaborative Research Program. General Effectiveness of treatments. Archives of general psychiatry. 10.1001/archpsyc.1989.01810110013002
- 66. Cuijpers, P., Geraedts, A. S., van Oppen, P., Andersson, G., Markowitz, J. C., & van Straten, A. (2011, June). Interpersonal psychotherapy for depression: A meta-analysis. The American journal of psychiatry. 10.1176/appi.ajp.2010.10101411
- 67. Cuijpers, Donker, T., Weissman, M. M., Ravitz, P., Cristea, I. A., Clinical, F. the D. of, Address correspondence to Dr. Cuijpers ([email protected])., JC, M., MM, W., P, C., Al., E., J, B., K, van Z., L, M., 3rd, R. C., F, L., C, G., W, F., … Fitzsimmons-Craft, E. E. (2016, April 1). Interpersonal psychotherapy for Mental Health Problems: A comprehensive meta-analysis. American Journal of Psychiatry. https://doi.org/10.1176/appi.ajp.2015.15091141
- 68. Recchia et al. (2022, September 16). Comparative effectiveness of exercise, antidepressants and their combination in treating non-severe depression: A systematic review and network meta-analysis of Randomised Controlled Trials. British journal of sports medicine. 10.1136/bjsports-2022-105964
- 69. Whiston et al. (2019, October 16). Towards personalising treatment: A systematic review and meta-analysis of face-to-face efficacy moderators of cognitive-behavioral therapy and interpersonal psychotherapy for major depressive disorder. Psychological medicine. 10.1017/S0033291719002812
- 70. Cuijpers et al. (2022, January 10). A network meta‐analysis of the effects of psychotherapies ... World Psychiatry. 10.1002/wps.20701
- 71. Walkup, J. T. (2017, March 3). Antidepressant efficacy for depression in children and adolescents: Industry- and NIMH-funded studies. American Journal of Psychiatry. 10.1176/appi.ajp.2017.16091059
- 72. Welch, A. (n.d.). Most antidepressants ineffective in teens, study finds. CBS News. https://www.cbsnews.com/news/most-antidepressants-ineffective-in-teens-study/
- 73. Murphy et al. (2021, September). The knowns and unknowns of SSRI treatment in young people with ... The knowns and unknowns of SSRI treatment in young people with depression and anxiety: efficacy, predictors, and mechanisms of action. 10.1016/S2215-0366(21)00154-1
- 74. Zajecka , J., Tracy, K. A., & Mitchell, S. (1997, July). Discontinuation symptoms after treatment with serotonin reuptake inhibitors: A literature review. The Journal of clinical psychiatry. 10.4088/jcp.v58n0702
- 75. S;, B. et al. (2000, May). Selective serotonin reuptake inhibitor discontinuation syndrome: Proposed diagnostic criteria. Journal of psychiatry & neuroscience : JPN. https://pubmed.ncbi.nlm.nih.gov/10863885/
- 76. Ferguson, J. M. (2001, February). SSRI antidepressant medications: Adverse effects and tolerability. Primary care companion to the Journal of clinical psychiatry. 10.4088/pcc.v03n0105
- 77. Teng, T., Zhang, Z., Yin, B., Guo, T., Wang, X., Hu, J., Ran, X., Dai, Q., & Zhou, X. (2022, May 4). Effect of antidepressants on functioning and quality of life outcomes in children and adolescents with major depressive disorder: A systematic review and meta-analysis. Nature News. 10.1038/s41398-022-01951-9
- 78. Murphy et al. (2021b, September). The knowns and unknowns of SSRI treatment in young people with depression and anxiety: efficacy, predictors, and mechanisms of action. The Lancet Psychiatry. 10.1016/S2215-0366(21)00154-1
- 79. Iñiguez, S. D., Warren, B. L., & Bolaños-Guzmán, C. A. (2010, February 20). Short- and long-term functional consequences of fluoxetine exposure during adolescence in male rats. Biological Psychiatry. 10.1016/j.biopsych.2009.12.033
- 80. Doggrell, S. A. (2005, January). Fluoxetine--do the benefits outweigh the risks in adolescent major depression?. Expert opinion on pharmacotherapy. 10.1517/14656566.6.1.147
- 81. Cousins, L., & Goodyer, I. M. (n.d.). Antidepressants and the adolescent brain. Journal of psychopharmacology (Oxford, England). 10.1177/0269881115573542
- 82. Moreland, S., & Bonin, L. (n.d.). Patient education: Depression treatment options for children and adolescents (Beyond the Basics). UpToDate. https://www.uptodate.com/contents/depression-treatment-options-for-children-and-adolescents-beyond-the-basics/print
Tables
- 1. Patra, S. (2019). Assessment and management of pediatric depression. Indian journal of psychiatry. 10.4103/psychiatry.IndianJPsychiatry_446_18
- 2. Mayo Foundation for Medical Education and Research. (2022, March 19). What to know about antidepressants for kids and teens. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/teen-depression/in-depth/antidepressants/art-20047502
- 3. Frazer, A., & Hensler, J. G. (n.d.). Serotonin receptors - basic neurochemistry - NCBI bookshelf. Serotonin Receptors. https://www.ncbi.nlm.nih.gov/books/NBK28234/
- 4. Low, Y., Setia, S., & Lima, G. (2018, February). Drug-drug interactions involving antidepressants: Focus on desvenlafaxine. Neuropsychiatric disease and treatment. 10.2147/NDT.S157708
Figures
- 1. The Lancet. (2021, October 8). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic 10.1016/S0140-6736(21)02143-7
- 2. Gogtay et al. (2004, May 17). Dynamic mapping of human cortical development during childhood through early adulthood ... 10.1073/pnas.0402680101
- 3. Lattimore, K. A., Donn, S. M., Kaciroti, N., Kemper, A. R., Neal, C. R., & Vazquez, D. M. (2005, July 14). Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and effects on the fetus and newborn: A meta-analysis. Nature News. 10.1038/sj.jp.7211352
Document information
Published on 04/03/24
Submitted on 10/02/24
Volume 6, 2024
Licence: CC BY-NC-SA license