Keywords
Acetylcholine;Vasospasm;Significant fixed stenosis
Cigarette smoking is an important preventive risk factor for coronary atherosclerosis and coronary spasm [1]. The morbidity increases annually in lifestyle-related disease, such as hypertension, diabetes mellitus, and dyslipidemia, whereas the percentage of smokers among adults has decreased not only in Japan, but all over the world. However coronary abnormal vasomotor response to acetylcholine has increased in Japanese patients during 17 years [2]. The purpose of this study was to clarify differences of clinical characteristics, and correlated factors for coronary spasm in patients with vasospastic angina (VSA) between two decades.
Details of study design, protocol of acetylcholine (ACh)-provocation testing, definition of coronary spasm, data collection and follow-up were described previously [3]. Briefly, this was a retrospective, observational study. After exclusion of 117 from 1877 consecutive patients undergoing acetylcholine (ACh)-provocation testing between January 1991 and December 2010, the remaining 1760 patients were analyzed. Based on the date of ACh-provocation testing, the patients were divided into 2 period groups: the former (1991–2000, n = 1055), and the latter (2001–2010, n = 705) group. We compared the clinical characteristics and correlated factors for coronary spasm between the groups. The study protocol was approved by the Human Ethics Review Committee of Kumamoto University and a signed consent form was obtained from each subject.
Variables were compared with the chi-square test of Fishers exact test, and the unpaired t test, as appropriate. Logistic regression analysis was used to compute odds ratios (ORs) and 95% confidence intervals (CI) as estimates for correlated factors of coronary spasm. A two-tailed P-value of < 0.05 denoted the presence of a statistically significant difference. All statistical analyses were performed with The Statistical Package for Social Sciences software version 23.0 (IBM Corporation, Armonk, New York).
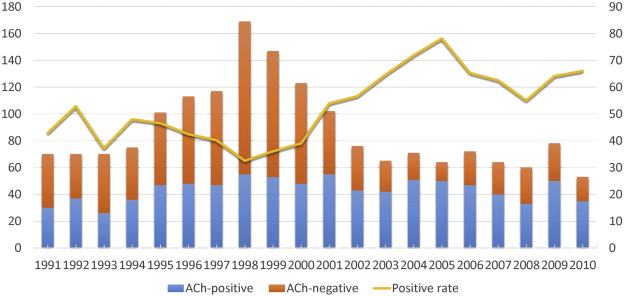
Table 1A shows clinical characteristics of entire cohort, VSA patients, and non-VSA patients. Among 1760 all patients who underwent ACh-provocation test, the patients in the latter group were more likely to be elderly female, and have higher BMI, diabetes mellitus, hypertension, and dyslipidemia, but less likely to have current smoking and family history of ischemic heart disease (IHD), compared to those in the former group. Fig. 1 shows annual changes of the results of ACh-provocation test between 1991 and 2010. ACh-provoked coronary spasm was observed frequently in the latter period, compared to the former period [446/705 (63.3%) vs. 427/1055 (40.5%), P < 0.001]. Similarly, even in 873 VSA patients, those in the latter group were more likely to be female, and have higher BMI, hypertension, and dyslipidemia, but less likely to have current smoking and family history of IHD, compared to those in the former group. We performed simple and multiple logistic regression analyses to compare differential correlated factors for coronary spasm between the 2 periods (Table 1B). Multiple logistic regression analysis identified that current smoking (OR: 1.66, 95% CI: 1.25–2.20), family history of IHD (OR: 2.74, 95% CI: 1.88–3.98), and significant organic stenosis (OR: 2.44, 95% CI: 1.73–3.44) were significant positive correlates but dyslipidemia (OR: 0.71, 95% CI: 0.52–0.96) was negative correlates with coronary spasm in the former period, whereas elderly (OR: 1.43, 95% CI: 1.01–2.02), dyslipidemia (OR: 2.37, 95% CI: 1.84–3.05), and significant organic stenosis (OR: 1.59, 95% CI: 1.15–2.20) were significant positive correlates in the latter period.
| All patients | VSA patients | Non-VSA patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1991–2000 2001–2010 P value | 1991–2000 2001–2010 P value | 1991–2000 2001–2010 P value | |||||||
| n | 1055 | 705 | 427 | 446 | 628 | 259 | |||
| Age (mean ± SD) | 62.2 ± 10.8 | 64.4 ± 11.0 | < 0.001 | 63.4 ± 9.9 | 64.3 ± 10.8 | 0.178 | 61.4 ± 11.4 | 64.5 ± 11.3 | < 0.001 |
| Gender (male) (%) | 570 (54.0) | 333 (47.2) | 0.005 | 266 (62.3) | 221 (49.6) | < 0.001 | 304 (48.4) | 112(43.2) | 0.161 |
| BMI | 23.5 ± 3.4 | 23.9 ± 3.8 | 0.021 | 23.4 ± 3.1 | 23.9 ± 3.9 | 0.027 | 23.6 ± 3.5 | 23.9 ± 3.4 | 0.270 |
| BMI > 25 | 307 (31.1) | 246 (35.2) | 0.072 | 112(28.1) | 152 (34.3) | 0.051 | 195 (33.1) | 94 (36.9) | 0.291 |
| Current smoking (%) | 528 (50.6) | 307 (43.5) | 0.004 | 252 (59.3) | 208 (46.6) | < 0.001 | 276 (44.6) | 99 (38.2) | 0.082 |
| Diabetes mellitus (%) | 180(17.1) | 167 (23.9) | 0.001 | 83 (19.5) | 96 (21.7) | 0.426 | 97(15.5) | 71 (27.6) | < 0.001 |
| Hypertension (%) | 357(33.9) | 362 (51.4) | < 0.001 | 147 (34.4) | 215 (48.2) | < 0.001 | 210(33.6) | 147 (57.0) | < 0.001 |
| Dyslipidemia (%) | 340 (32.3) | 403 (57.3) | < 0.001 | 139 (32.6) | 267 (60.0) | < 0.001 | 201 (32.1) | 136(52.7) | < 0.001 |
| Family history of IHD (%) | 153 (14.7) | 76(10.8) | 0.019 | 95 (22.4) | 50(11.2) | < 0.001 | 58 (9.4) | 26(10.1) | 0.751 |
| CKD (eGFR < 60) | 178 (20.8) | 141 (20.7) | 0.966 | 79 (23.6) | 84(19.5) | 0.175 | 99(19.0) | 57 (22.7) | 0.230 |
| Organic stenosis | 211 (20.0) | 146 (20.7) | 0.717 | 126 (29.5) | 106 (23.8) | 0.055 | 85 (13.5) | 40(15.4) | 0.458 |
|
|
|
Fig. 1. Annual changes of the results of ACh-provocation testing between 1991 and 2010. |
| 1991–2000 | 2001–2010 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Simple logistic regression | Multiple logistic regression | Simple logistic regression | Multiple logistic regression | |||||||||
| OR 95% CI | P value | OR 95% CI | P value | OR | 95% CI | P value | OR 95% CI | P value | ||||
| Elderly (age > 75 yrs) | 0.77 | 0.53–1.12 | 0.168 | 0.67 | 0.42–1.05 | 0.081 | 1.64 | 1.20–2.23 | 0.002 | 1.43 | 1.01–2.02 | 0.045 |
| Female | 0.54 | 0.42–0.68 | < 0.001 | – | – | – | 0.90 | 0.72–1.13 | 0.360 | – | – | – |
| BMI > 25 | 0.75 | 0.58–0.97 | 0.030 | 0.92 | 0.68–1.25 | 0.579 | 1.00 | 0.79–1.28 | 0.980 | 0.98 | 0.75–1.28 | 0.872 |
| Current smoking | 1.95 | 1.54–2.47 | < 0.001 | 1.66 | 1.25–2.20 | < 0.001 | 1.17 | 0.93–1.47 | 0.174 | 1.12 | 0.87–1.44 | 0.386 |
| Diabetes mellitus | 1.03 | 0.77–1.38 | 0.829 | 0.80 | 0.56–1.15 | 0.223 | 1.18 | 0.89–1.57 | 0.247 | 0.80 | 0.59–1.10 | 0.171 |
| Hypertension | 0.77 | 0.61–0.98 | 0.036 | 0.88 | 0.66–1.19 | 0.411 | 1.37 | 1.09–1.73 | 0.007 | 1.14 | 0.88–1.47 | 0.336 |
| Dyslipidemia | 0.79 | 0.62–1.00 | 0.053 | 0.71 | 0.52–0.96 | 0.024 | 2.44 | 1.93–3.07 | < 0.001 | 2.37 | 1.84–3.05 | < 0.001 |
| Family history of IHD | 2.71 | 1.97–3.74 | < 0.001 | 2.74 | 1.88–3.98 | < 0.001 | 1.19 | 0.82–1.72 | 0.356 | 1.34 | 0.89–2.00 | 0.159 |
| eGFR < 60 | 1.22 | 0.90–1.66 | 0.208 | 1.15 | 0.81–1.63 | 0.445 | 0.96 | 0.71–1.29 | 0.780 | 0.80 | 0.58–1.10 | 0.167 |
| Organic stenosis | 2.55 | 1.93–3.38 | < 0.001 | 2.44 | 1.73–3.44 | < 0.001 | 1.92 | 1.44–2.57 | < 0.001 | 1.59 | 1.15–2.20 | 0.005 |
Although the percentage of smokers decreased in recent, ACh-provoked abnormal response has increased in the present study, which were consistently in agreement with previous study [2]. The present study indicated that current smoking was a risk factor for coronary spasm in the former period, but was not in recent. It is possible that risk factors for coronary spasm might have changed among two decades because a lifestyle of Japanese has changed in Western-style recently. However, significant organic stenosis was correlated with coronary spasm consistently among two decades. Previous study reported that coronary spasm occurs at sites of atherosclerotic lesion, and plays a potential role in atherosclerosis progression [4]. Atherosclerotic disease has increased in Japanese with a change in lifestyle. It might be a reason why coronary abnormal response has increased. Furthermore, significant organic stenosis is an important factor in VSA patients because previous studies showed that VSA patients with significant organic stenosis had a high risk for future cardiovascular events [3] ; [5]. Consequently, cardiologist should pay attention to atherosclerotic risk factors in the management of VSA patients, and should not miss coronary spasm in the management of patients with obstructive coronary artery disease who complain of chest pain unexplained by the presence of organic stenosis only.
In conclusions, our results suggested that clinical characteristics, correlated factors for coronary spasm in VSA patients have changed among two decades, but significant fixed stenosis was an invariable correlated factor for coronary spasm.
Disclosure
The authors declare no conflict of interest.
References
- [1] K. Takaoka, M. Yoshimura, H. Ogawa, et al.; Comparison of the risk factors for coronary artery spasm with those for organic stenosis in a Japanese population: role of cigarette smoking; Int. J. Cardiol., 72 (2000), pp. 121–126
- [2] S. Sueda, H. Kohno, A. Oshita, et al.; Coronary abnormal response has increased in Japanese patients: analysis of 17 years' spasm provocation tests in 2093 cases; J. Cardiol., 55 (2010), pp. 354–361
- [3] M. Ishii, K. Kaikita, K. Sato, et al.; Acetylcholine-provoked coronary spasm at site of significant organic stenosis predicts poor prognosis in patients with coronary vasospastic angina; J. Am. Coll. Cardiol., 66 (2015), pp. 1105–1115
- [4] Y. Ozaki, D. Keane, P.W. Serruys; Progression and regression of coronary stenosis in the long-term follow-up of vasospastic angina; Circulation, 92 (1995), pp. 2446–2456
- [5] Y. Takagi, J. Takahashi, S. Yasuda, et al.; Prognostic stratification of patients with vasospastic angina: a comprehensive clinical risk score developed by the Japanese Coronary Spasm Association; J. Am. Coll. Cardiol., 62 (2013), pp. 1144–1153
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?