Summary
Background
We introduced a modified laparoscopic technique, dual-incision laparoscopic adrenalectomy (DILA), using a newly designed multichannel trocar, and we evaluated its perioperative outcomes and operative costs and compared them to those of conventional laparoscopic adrenalectomy (CLA).
Methods
We retrospectively reviewed the medical records of 127 patients who underwent CLA with four trocars or DILA with two trocars at Seoul St. Marys Hospital, Seoul, Korea between October 2007 and September 2014. We analyzed the patients' surgical outcomes and perioperative morbidities.
Results
DILA was performed in 45 patients and CLA in 82 patients. There were no significant differences in operative time (DILA: 77.1 ± 28.4 minutes vs. CLA: 76.6 ± 28.0 minutes, p = 0.595) or estimated blood loss during surgery (DILA: 150.0 ± 85.5 mL vs. CLA: 175.5 ± 50.5 mL, p = 0.697). There were no differences in postoperative hospital stay, visual analog scale pain score, or postoperative complication rates between the two groups. However, the operative cost was significantly lower in the DILA group (DILA 813,603 ± 48,600 Korean won vs. CLA 968,368 ± 56,456 Korean won, p < 0.001).
Conclusion
This study demonstrated that DILA is a safe and feasible surgical approach for adrenal diseases. DILA may reduce the operative cost significantly compared with CLA.
Keywords
adrenalectomy;cost;laparoscopy;multichannel port
1. Introduction
Since laparoscopic adrenalectomy was first reported in 1992 by Gagner et al,1 it has become widely accepted as a standard operative modality for various adrenal gland diseases. The advantages of laparoscopic surgery over conventional open surgery are shorter hospital stays, more rapid recovery, reduced incisional morbidity, improved cosmesis, and greater cost effectiveness.2; 3 ; 4 To date, several modified and less invasive techniques, such as single port laparoscopic adrenalectomy (SPLA), have been reported by several investigators.5 ; 6 However, there have been controversies concerning whether single port surgery (SPS) has significant advantages over conventional laparoscopic surgery using multiport approaches, specifically in the area of a solid organ surgeries such as adrenalectomy.7 These techniques have not yet gained definite momentum because of their intrinsic technical difficulties, including loss of triangulation and interference between instruments, as well as a lack of suitable instruments. Furthermore, SPS generally requires a longer operative time, specially designed equipment and a highly experienced surgeon.8 ; 9
The authors have also been performing SPS for several diseases and have reported their experiences.10 ; 11 In this study, we introduced a modified laparoscopic technique for adrenal diseases, dual-incision laparoscopic adrenalectomy (DILA), using a newly designed multichannel trocar. Furthermore, we analyzed the operative outcomes between DILA and conventional laparoscopic adrenalectomy (CLA) and verified the cost effectiveness of DILA compared with CLA.
2. Patients and methods
2.1. Patients
From October 2007 to September 2014, we collected data prospectively and retrospectively from the medical records of 133 patients who underwent a laparoscopic adrenalectomy at Seoul St. Marys Hospital, Seoul, Korea. Two types of surgical approaches were used: conventional laparoscopic surgery with four trocars and dual incision laparoscopic surgery using a multichannel trocar. We excluded six patients from the present study who underwent concomitant laparoscopic surgeries, such as laparoscopic cholecystectomy or colon surgery, which inevitably required additional trocars and operative time. This study was approved by the Institutional Review Board of the ethics committee of our hospital.
The three surgeons who were enrolled in this study had performed CLA surgeries for at least 5 years. DILA was initially introduced in May 2012 and, since then, it has been performed consistently by one surgeon after patients provide their consent.
2.2. Clinical outcomes
Demographic data, including age, sex, body mass index, American Society of Anesthesiologists score, and size of the adrenal gland on computed tomography (CT) scans, were compared between the DILA and CLA groups. The confirmative pathology after surgery was also verified. The operative parameters, such as intraoperative blood loss volume, transfusion rate, conversion rate to open surgery, operative time and operative costs, and the postoperative parameters, which included the number of postoperative days spent in the hospital, the surgical complications and the visual analog scale (VAS) pain scores, were recorded for each procedure. The VAS pain score was routinely assessed 12 hours after surgery.12
The operative time consisted of the duration of the entire procedure from skin incision to wound closure. The operative costs were calculated by summing the cost of the disposable surgical supplies and items. This value was abstracted from the operating room resource utilization reports. The surgical fee, anesthesia fees, and all of the postsurgery costs, including hospital room costs, were not included in the operative costs. All costs are presented in Korean won (KRW).
All of the patients underwent routine preoperative CT to determine the location and size of the adrenal gland. In some patients, an endocrine function test, such as high dose or low dose dexamethasone suppression tests and plasma rennin activity, was performed in the Department of Endocrinology, Seoul St. Marys Hospital prior to surgery if the patients had diabetes mellitus, hypertension, or Cushings syndrome.
2.3. Surgical procedures
Generally, there were few differences between the operative methods performed during the DILA and CLA procedures, except for the difference in trocar use.
The patients were placed in right or left lateral decubitus in the reverse Trendelenburg position at approximately 60°. The table was flexed at the waist area of the patient to increase the space between the subcostal margin and the iliac crest.
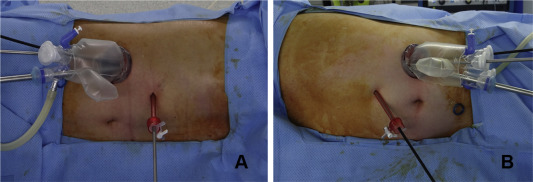
For the DILA procedure, an incision at least 20 mm in length was made at the right or left upper abdominal quadrant, depending on the location of the adrenal gland that was scheduled for surgery, and then the multiport device was inserted. The precise incision size for the multichannel trocar was determined by the size of the tumor on CT scans, and the size was generally approximately 20% smaller than the length of the short axis of the tumor. An additional 5-mm trocar was inserted at the subxiphoid area. We used a specially designed multichannel trocar (Glove Port; Nelis, Seoul, Republic of Korea) consisting of two rings and four trocar channels with gas insufflation and exsufflation lines (Fig. 1). The finished product is similar to the homemade glove port commonly used for other SPS or dual incision surgeries. The trocar consists of transparent material and allows for smooth and safe introduction of the instruments. It also enables intracorporeal crossing and rearrangement of the instruments. Therefore, the interference between instruments is reduced. Furthermore, the trocar can introduce a 10-mm scope, an additional liver retractor (Snake Liver Retractor, Artisan medical, Medford, NJ, USA) and a grasper during right adrenalectomy, as well as, in the case of left adrenalectomy, a 10-mm scope, a grasper with gauze, a dissector, endo-clips or a 5-mm ultrasonic scalpel (Harmonic ACE; Ethicon Endo-Surgery, Cincinnati, OH, USA) inserted through it. In addition to the multichannel trocar, an additional 5-mm trocar was introduced at the subxiphoid area, and a 5-mm ultrasonic scalpel, a dissector or endo-clips were inserted through it during right adrenalectomy. In cases of left adrenalectomy, only a 5-mm grasper was inserted through the 5-mm trocar (Fig. 2).
|
|
|
Figure 1. A specially designed multichannel trocar (Glove Port; Nelis, Seoul, Republic of Korea), consisting of two rings and four trocar channels with gas insufflation and exsufflation lines. |
|
|
|
Figure 2. An extracorporeal view of dual incision laparoscopic adrenalectomy (A) right; (B) left. |
For CLA, four trocars were inserted, as follows: during a right adrenalectomy, one 10-mm trocar was inserted approximately 2 cm to the right and 2 cm above the umbilicus for the scope. For a left adrenalectomy, this trocar was inserted at the same location on the opposite side, and three additional 5-mm trocars were inserted for the working instrument and retractor at the right or left upper abdominal quadrant below the subcostal margin.
For a left adrenalectomy, the splenic flexure of the colon was mobilized to expose the left kidney using an ultrasonic scalpel. Next, a dissection was performed between the spleen and the left kidney to visualize the left adrenal gland. The lower part of the pancreas tail was also dissected, and the mobilized pancreas tail was then raised upward using the grasper with gauze to create a space for surgery. Because the blood supply to the left adrenal gland is concentrated at the medial–inferior section, the superior–lateral part of the adrenal gland was dissected first. Then, the supply vessels were ligated with endo-clips and divided with an ultrasonic scalpel. After mobilization of the adrenal gland from the superior pole of the left kidney, a specimen was placed into a retrieval bag, which was introduced through the multichannel trocar in DILA or through the 10-mm port in CLA. In general, most operative cases for adrenal gland diseases are tumorous conditions; therefore, a trocar site extension sufficient for preserving the specimen is required. For DILA, the incision size was sufficiently extended, depending on the specimen size, at the beginning of the operation. However, for CLA, an extension of the 10-mm trocar site was performed in almost all of the cases. A closed suction drain was inserted to prevent fluid collection and to enable the early detection of bleeding. The drain was inserted through the additional 5-mm trocar site in DILA and through the outer 5-mm trocar site in CLA.
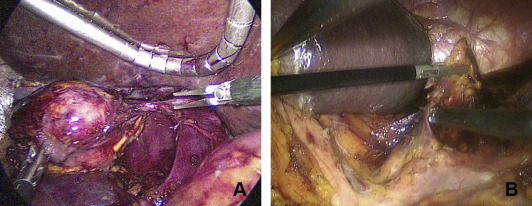
In right adrenalectomy cases, there were few differences compared with left adrenalectomy except for the anatomy around the adrenal gland. A liver retractor was routinely inserted through the multichannel port for superior retraction of the liver. The adrenal gland was easily exposed after mobilization of the liver by dissecting the triangular ligament. Generally, the right adrenal vein was inserted into the posterolateral aspect of the inferior vena cava, and great care was taken when dissecting the medial aspect of the adrenal gland (Fig. 3).
|
|
|
Figure 3. An intracorporeal view of dual incision laparoscopic adrenalectomy (A) right; (B) left. |
The resumption of oral intake occurred shortly after surgery. All of the patients initiated their diets immediately after recovering from anesthesia. If there were no specific complications, the patient was discharged after a normal diet became possible.
2.4. Statistical analysis
Means, standard deviations, and ranges were used as the numerical data. For comparisons between the groups consisting of categorical variables, Fishers exact test was used. Student t test and the Mann–Whitney U test were used for continuous variables. A p value < 0.05 was considered statistically significant.
3. Results
In total, 127 patients were enrolled in this study. Among them, DILA was performed in 45 patients, while CLA was performed in 82 patients. The demographic characteristics and pathologic diagnoses of the two groups are listed in Table 1. There were no statistically significant differences in age (52.6 ± 12.9 years vs. 49.2 ± 11.8 years, p = 0.133), sex ratio (M:F: 21:24 vs. 35:47, p = 0.711), American Society of Anesthesiologists score I/II/III (10/30/50 vs. 17/55/10, p = 0.970), or size of the adrenal mass (4.4 ± 2.7 cm vs. 4.5 ± 2.3 cm, p = 0.704). In the DILA group, the more common operative side was the right adrenal gland (27 of 45 cases, 56.5%), but in the CLA group, more than half of the cases (51 of 82 cases, 62.2%) involved the left adrenal gland (p = 0.031). There was one case of bilateral adrenalectomy in each group. From the perspective of pathologic findings, the most prevalent operative indication in both groups was functioning adenoma, such as from primary aldosteronism and Cushings syndrome (44.4% and 57.3%, respectively). The next most common operative indications in the DILA group were pheochromocytoma (37.8%) and nonfunctioning tumors, such as cortical adenomas (8.9%). In the CLA group, pheochromocytoma was also the second most common operative indication (26.8%), followed by nonfunctioning tumors (8.5%). There were two cases of malignant tumors in the DILA group and four cases in the CLA group. Three cases of ganglioneuromas were also included: two in the DILA group and one in the CLA group. One case of myelolipoma was involved in the CLA group. There were no statistically significant differences in pathologic diagnosis between the two groups (p = 0.657).
| DILA (n = 45) | CLA (n = 82) | p | |
|---|---|---|---|
| Age (y) | 52.6 ± 12.9 | 49.2 ± 11.8 | 0.133 |
| Sex (male/female) | 21/24 | 35/47 | 0.711 |
| BMI (kg/m²) | 24.1 ± 3.7 | 23.7 ± 3.3 | 0.523 |
| ASA score I/II/III | 10/30/5 | 17/55/10 | 0.970 |
| Tumor size (cm) | 4.4 ± 2.7 | 4.5 ± 2.3 | 0.704 |
| Operative side | 0.031 | ||
| Right | 27 (60.0) | 30 (36.6) | |
| Left | 17 (37.8) | 51 (62.2) | |
| Both | 1 (2.2) | 1 (1.2) | |
| Diagnosis | 0.657 | ||
| Functioning adenoma | 20 (44.4) | 47 (57.3) | |
| Pheochromocytoma | 17 (37.8) | 22 (26.8) | |
| Nonfunctioning tumor type | 4 (8.9) | 7 (8.5) | |
| Malignant tumor | 2 (4.4) | 4 (4.9%) | |
| Other | 2 (4.4) | 2 (2.4%) |
Data are presented as mean ± SD or n (%).
ASA = American Society of Anesthesiologists; BMI = body mass index; CLA = conventional laparoscopic adrenalectomy; DILA = dual incision laparoscopic adrenalectomy.
The surgical outcomes and operative costs are summarized in Table 2. There were no conversions to open surgery in either group. However, one case required another 5-mm trocar in the DILA group to control accidental bleeding from the left adrenal vein. The mean operative times for DILA and CLA were 77.1 ± 28.4 minutes and 76.6 ± 28.0 minutes, respectively, and there was no significant difference between the two groups (p = 0.595). The estimated blood loss was similar between the two groups (150.0 ± 85.5 vs. 175.5 ± 50.5, p = 0.697). No patients required intraoperative transfusions of red blood cell substitution in either group. In terms of the postoperative VAS pain score, length of hospital stay, and resumption of oral intake, there were no statistically significant differences between the two groups. Only one patient suffered from postoperative complications in each group. One patient suffered from pulmonary edema and atelectasis in the DILA group, and the other patient suffered from arterial fibrillation in the CLA group. Both patients were treated with conservative care and were eventually discharged on the 6th postoperative day and 5th postoperative day, respectively, without any other sequelae. No late complications, including incisional hernia, were observed in either group, and there was no postoperative mortality in this study. As shown in Table 2, the mean operative cost was calculated to be 813,603 ± 48,600 KRW for DILA and 968,368 ± 56,456 KRW for CLA. The costs for DILA were significantly lower for CLA in all of the cases (p < 0.001). This observation demonstrates that the effective reduction of operative costs averaged approximately 16.0%.
| DILA (n = 45) | CLA (n = 82) | p | |
|---|---|---|---|
| Conversion (n) | 0 | 0 | |
| Operative time (min) | 77.17 ± 28.47 | 76.64 ± 28.09 | 0.595 |
| Blood loss (mL) | 102.73 ± 142.27 | 157.14 ± 161.83 | 0.035 |
| Transfusion (n) | 0 | 0 | |
| VAS pain score | 3.2 ± 1.6 | 3.5 ± 1.4 | 0.327 |
| Resumption of oral intake (d) | 1.0 ± 0.0 | 1.0 ± 0.2 | 0.225 |
| Postoperative hospital stay (d) | 4.3 ± 2.4 | 3.9 ± 1.7 | 0.260 |
| Postoperative complication (%) | 1 (2.2) | 1 (1.2) | 0.664 |
| Operative cost (KRW) | 813,603 ± 48,600 | 968,368 ± 56,456 | < 0.001 |
CLA = conventional laparoscopic adrenalectomy; DILA = dual incision laparoscopic adrenalectomy; KRW = Korean won; VAS = visual analog scale.
4. Discussion
Laparoscopic adrenalectomy has replaced open conventional surgery and has become a standard operative modality for various adrenal diseases. The benefits of laparoscopic adrenalectomy over conventional surgery have been demonstrated by several investigators. These benefits include shorter hospital stays, less blood loss, less postoperative pain, and improved cosmesis, as well as more rapid recovery. The efforts to maximize the procedures benefits have been leading surgeons to reduce invasiveness further, specifically by reducing the number of trocars. SPS is one of these modified techniques and has recently gained momentum in many surgical areas, such as cholecystectomy, appendectomy, and hernia repair.10 ; 11 However, in the area of laparoscopic adrenalectomy, SPS has not gained momentum due to its technical difficulties and longer operative time. Consequently, only a few studies using this approach have been reported.5; 6 ; 7
Ishida et al7 reported comparative results between SPLA and CLA. They reported that SPLA was feasible but required additional time for instrument adjustment, and there were more tissue regrasping maneuvers during surgery. Another investigator reported similar results, observing that SPLA appeared to require a longer operative time than CLA.13 Most authors who have reported favorable results with SPLA have commonly stated that specially designed laparoscopic instruments, such as articulating instruments, should be used to reduce the operative time.5 ; 7 Collectively, SPLA operations have had favorable results; however, they require a longer operation time, specially designed equipment (for SPS), advanced technical skill, and highly experienced surgeons. Additionally, adrenal gland surgery has anatomical differences compared with other surgical fields, i.e., monitoring the liver during the operation in the case of right adrenal gland diseases and dissecting under the spleen and pancreas tail in the case of left adrenal gland diseases. Furthermore, intrinsic problems of SPS, such as interference between instruments and lack of triangulation between the right and left instruments, also make SPLA very difficult. However, in DILA, the additional 5-mm laparoscopic instrument at the subxiphoid area and the liver retractor inserted through the multichannel trocar to raise the liver or pancreas tail, including the spleen, provide a similar surgical environment as for CLA. Furthermore, only conventional laparoscopic instruments enable DILA without compromising ergonomics. Therefore, a surgeon who has experience with CLA may perform DILA without a long learning curve.
In the near future, it is expected that surgical techniques and instruments for SPLA will be improved. However, DILA currently appears to be more applicable as a reduced port operation because it does not require specially designed instruments or a long learning curve, compared with SPLA.
In the present study, the operative time and conversion rate to open surgery, which may be used as parameters of surgical difficulty, revealed no significant differences between DILA and CLA. In terms of the postoperative outcomes, there were no significant differences in the length of hospital stay, postoperative pain score, or resumption of oral intake. There was only one case of postoperative complications in each group: pulmonary edema with atelectasis and atrial fibrillation, respectively. However, these complications were not directly associated with the operative method.
Some investigators have reported successful laparoscopic adrenalectomies in large benign tumors > 6 cm,14 ; 15 and in the present study, the largest adrenal gland size dissected using DILA was 8.5 cm. The operative time for this surgery was 85 minutes, estimated blood loss was 30 mL, and the length of the hospital stay was 4 days, which were favorable results without any operative and postoperative complications within the average range of this study. The reason for this similarity between surgery types might be that DILA provides an ergonomically similar operative environment to CLA.
CLA usually uses a four-port system, consisting of one 10-mm incision for a scope and three 5-mm incisions for working instruments. Intuitively, the total incision length is not different for DILA, which requires at least one 2-cm incision and one 5-mm incision. However, one of the skin incisions is usually extended for the extraction of large specimens during the last step of CLA because most of the operative indications for adrenal gland disease are tumorous conditions that require an intact specimen. Therefore, the total length of the skin incisions in DILA was no longer (or was shorter) than in CLA. However, the actual length of the total skin incisions could not be compared due to a lack of medical records.
In the present study, the operative cost of DILA was estimated to be less than that of CLA. This finding was presumably due to the reduced number of trocars; generally, four trocars were used for CLA and two trocars for DILA. Although the specially designed multichannel trocar used for DILA is slightly more expensive than the commonly used 10-mm trocar in our country, it is not more than twice the price. The amounts and costs of other devices and materials that were used during surgery did not differ significantly between DILA and CLA.
This study was a retrospective study that was performed in one hospital and that enrolled a relatively small number of patients. The use of the DILA method was at the discretion of the surgeon rather than by randomization; therefore, selection bias was likely to be present. In addition, the DILA method was recently developed, indicating that DILA might have been performed by more experienced surgeons. Consequently, differences in outcomes derived from the degree of surgeon experience might exist. Therefore, a prospective and randomized study would be necessary to perform a more accurate comparison of DILA and CLA.
5. Conclusion
This study demonstrated that DILA is a safe and feasible surgical approach for adrenal diseases. DILA had comparable surgical outcomes to CLA and was more cost effective. DILA effectively reduced the number of trocars and, consequently, further minimized trocar site injury, compared with CLA. DILA could also overcome the technical limitations of SPLA.
References
- 1 M. Gagner, A. Lacroix, E. Bolté; Laparoscopic adrenalectomy in Cushings syndrome and pheochromocytoma; N Engl J Med, 327 (1992), p. 1033
- 2 J. Ortega, C. Sala, S. Garcia, S. Lledo; Cost-effectiveness of laparoscopic vs open adrenalectomy: small savings in an expensive process; J Laparoendosc Adv Surg Tech A, 12 (2002), pp. 1–5
- 3 S.R. Schell, M.A. Talamini, R. Udelsman; Laparoscopic adrenalectomy for nonmalignant disease: improved safety, morbidity, and cost-effectiveness; Surg Endosc, 13 (1999), pp. 30–34
- 4 S.K. Thompson, A.V. Hayman, W.H. Ludlam, C.W. Deveney, D.L. Loriaux, B.C. Sheppard; Improved quality of life after bilateral laparoscopic adrenalectomy for Cushings disease: a 10-year experience; Ann Surg, 245 (2007), pp. 790–794
- 5 F. Tunca, Y.G. Senyurek, T. Terzioglu, Y. Iscan, S. Tezelman; Single-incision laparoscopic adrenalectomy; Surg Endosc, 26 (2012), pp. 36–40
- 6 B.C. Jeong, Y.H. Park, D.H. Han, H.H. Kim; Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study; J Endourol, 23 (2009), pp. 1957–1960
- 7 M. Ishida, A. Miyajima, T. Takeda, M. Hasegawa, E. Kikuchi, M. Oya; Technical difficulties of transumbilical laparoendoscopic single-site adrenalectomy: comparison with conventional laparoscopic adrenalectomy; World J Urol, 31 (2013), pp. 199–203
- 8 M.M. Lirici; Single site laparoscopic surgery: an intermediate step toward no (visible) scar surgery or the next gold standard in minimally invasive surgery?; Minim Invasive Ther Allied Technol, 21 (2012), pp. 1–7
- 9 A. Islam, A.O. Castellvi, S.T. Tesfay, A.D. Castellvi, A.S. Wright, D.J. Scott; Early surgeon impressions and technical difficulty associated with laparoendoscopic single-site surgery: a Society of American Gastrointestinal and Endoscopic Surgeons Learning Center study; Surg Endosc, 25 (2011), pp. 2597–2603
- 10 Y.S. Lee, J.H. Kim, E.J. Moon, et al.; Comparative study on surgical outcomes and operative costs of transumbilical single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy in adult patients; Surg Laparosc Endosc Percutan Tech, 19 (2009), pp. 493–496
- 11 T.H. Hong, Y.K. You, K.H. Lee; Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy; Surg Endosc, 23 (2009), pp. 1393–1397
- 12 A. Fiorelli, F. Morgillo, R. Milione, et al.; Control of post-thoracotomy pain by transcutaneous electrical nerve stimulation: effect on serum cytokine levels, visual analogue scale, pulmonary function and medication; Eur J Cardiothorac Surg, 41 (2012), pp. 861–868 discussion 868
- 13 Q. Hu, Y. Gou, C. Sun, K. Xu, G. Xia, Q. Ding; A systematic review and meta-analysis of current evidence comparing laparoendoscopic single-site adrenalectomy and conventional laparoscopic adrenalectomy; J Endourol, 27 (2013), pp. 676–683
- 14 J.F. Henry, F. Sebag, M. Iacobone, E. Mirallie; Results of laparoscopic adrenalectomy for large and potentially malignant tumors; World J Surg, 26 (2002), pp. 1043–1047
- 15 E. Kebebew, A.E. Siperstein, O.H. Clark, Q.Y. Duh; Results of laparoscopic adrenalectomy for suspected and unsuspected malignant adrenal neoplasms; Arch Surg, 137 (2002), pp. 948–951 discussion 952–943
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?