Summary
Background
Preservation of the external branch of the superior laryngeal nerve (EBSLN) during thyroidectomy is important because its injury may lead to frequent occurrence of vocal fatigue and the inability to perform superenergetic phonation. Most studies on the anatomy of EBSLN have been performed in Western countries and, thus, have some limitations in their application to Koreans. We explored the anatomy of EBSLNs using intraoperative neuromonitoring (IONM) in Korean adults.
Methods
Between August 2011 and December 2011, 50 patients underwent thyroidectomy at Korea University, Anam Hospital in Seoul, Korea. IONM was performed with the NIM response 3.0 system.
Results
Forty-two total thyroidectomies and eight lobectomies were performed with IONM and 92 EBSLNs were evaluated. Type I EBSLN was observed in 15 of the 92 nerves (16.3%), type IIa EBSLN was noted in 52 (56.5%) and type IIb EBSLN was noted in 25 (27.2%). Patients with types IIa and IIb were at higher risk of injuries and these types were more frequently observed (83.7%) compared with previous Western studies. We found that 35.9% of distal insertion sites of EBSLNs were located within 1 cm of the center of the cricoid cartilage.
Conclusion
Surgeons should pay close attention to preserving the EBSLN during thyroidectomy in Korean patients because their EBSLNs are more frequently located beneath the superior thyroid vessels.
Keywords
intraoperative neuromonitoring;superior laryngeal nerve;thyroidectomy
1. Introduction
Most endocrine surgeons have focused on preserving the recurrent laryngeal nerve (RLN) due to its common complications (such as hoarseness, dysphagia, and aspiration) during thyroidectomy. Therefore, the clinical importance of the external branch of the superior laryngeal nerve (EBSLN) has been less emphasized and receives little attention during thyroidectomy. However, the EBSLN innervates the cricothyroid muscle; superenergetic phonation and the frequent occurrence of voice fatigue may result from injury to this nerve, which can negatively affect patient quality of life after surgery. Therefore, the importance of preserving this nerve has been greatly emphasized.1; 2; 3; 4; 5 ; 6
The superior laryngeal nerves arise from the inferior ganglion of the tenth cranial nerve, descend alongside the pharynx posterior to and then medial to the internal carotid artery, and then divide into a larger internal branch and a smaller external branch. The EBSLN descends posterior to the sternothyroid muscle and the superior thyroid artery to supply the inferior constrictor and cricothyroid muscle.7
Most surgeons have still not routinely performed the identification of the EBSLN during thyroidectomy because this procedure is invasive and harmful to postoperative voice outcome. Recently, intraoperative neuromonitoring (IONM) was reported to be helpful and less invasive in identifying EBSLN during thyroidectomy, which was thought to be almost impossible in the past.8 ; 9 Such findings have increased surgical interest and recognition of the usefulness and effectiveness of intraoperative neuromonitoring. Selvan et al10 identified the anatomic location of the EBSLN using IONM in their study of 35 thyroid patients and proposed a new EBSLN classification that is different from the previous cadaver-based EBSLN classification.
Most studies on the anatomy of EBSLN have been performed in Western countries and, based on the cadavers, they have limitations in the application to Korean adults during thyroidectomy. For this reason, we explored the anatomy of EBSLNs using IONM during thyroidectomy in Korean adults.
2. Materials and methods
2.1. Patients
A total of 50 patients with thyroid tumors underwent thyroidectomy at the Korea University Anam Hospital in Seoul, Korea, between August 2011 and December 2011. Approval to conduct this study was obtained from the Institutional Review Board of Korea University. Exclusion criteria were (1) previous thyroid surgery or other surgery involving neck dissection, (2) large goiter or Graves disease, (3) previous history of radiation to the neck, and (4) neuromuscular disease.
2.2. Surgical method and intraoperative neuromonitoring of the EBSLN
All procedures were performed by a single surgeon (H.Y.K.) using the classic open thyroidectomy method. The NIM response 3.0 system (Xomed Medtronics, Jacksonville, FL, USA) was used in all cases. Lobectomy was performed for patients with benign tumors or those with indeterminate tumors such as follicular neoplasm. In cases of malignancy, lobectomy was only considered in women under the age of 45 who had a single tumor smaller than 0.5 cm in size. Otherwise, total thyroidectomy was performed. The central neck node dissection was performed in all patients with malignant disease and the lateral neck node dissection was performed in patients who had lateral neck lymph node enlargement on preoperative computed tomography scan.
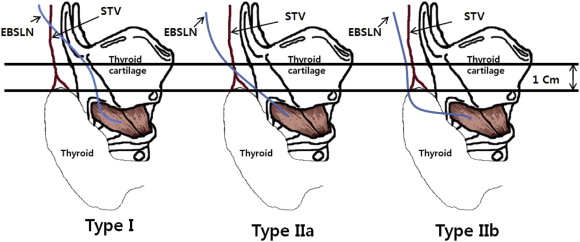
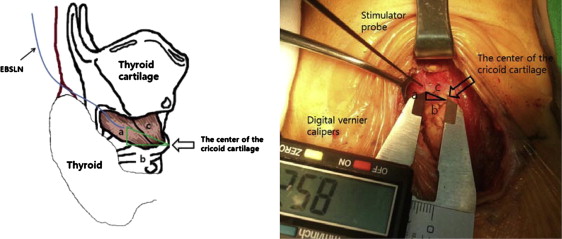
Patients were placed in the supine position with neck extension using a shoulder pillow after the induction of general anesthesia using electromyogram (EMG) and an endotracheal tube (Xomed Medtronics). A ground electrode was applied to the posterior part of the right shoulder. After draping, a 5-cm-sized collar incision was made in the natural skin crease of the lower neck. We performed subplatysmal dissection to the hyoid bone for identifying the relationship EBSLN and superior thyroidal vessels. After raising the myocutaneous flaps, the strap muscles were separated and retracted at midline to permit exposure of the thyroid gland. The middle thyroid vein was ligated using a Harmonic Scalpel (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA). After the vagus and recurrent laryngeal nerves were identified, a stimulator probe (strength: 1 mA) was placed on these nerves to confirm the absence of muscle paralysis before identification of the EBSLN. The avascular space between the cricothyroid muscle and the superior thyroid vessels was dissected, and a stimulator probe was applied to the cricothyroid muscle to identify the EBSLN. The stimulator probe was set to 0.5 mA, and this setting was not increased. A positive signal was determined by observing repetitive contractions of the cricothyroid muscle or an auditory signal.8 The EBSLN was traced from the distal to the proximal site using IONM to determine the relationship between the EBSLN and the superior thyroid vessels. If identifying the relationship was difficult due to lower incision or large gland, the additional incision was made laterally in previous incision for the procedures. We classified the anatomy of the EBSLN into types I, IIa, and IIb using Cernea classification as follows. In type I, the EBSLN crosses the superior thyroidal vessels at least 1 cm above a plane horizontal to the upper edge of the superior thyroid pole; in type IIa, the distance is shorter than 1 cm and is not below the plane; in type IIb, the EBSLN is below the plane (Fig. 1).1 We also measured the distance from the center of the cricoid cartilage to the distal insertion of the EBSLN in the cricoid muscle using digital vernier calipers under IONM guidance (Fig. 2). If the superior thyroid vessels interfered with this measurement, then they were ligated and a lobectomy was performed using a Harmonic Scalpel (Ethicon Endo-Surgery Inc.). EBSLN of the contralateral lobe was examined using the same maneuver as in cases with total thyroidectomy.
|
|
|
Figure 1. Cernea classification of the EBSLN. In type I, the EBSLN crosses the superior thyroidal vessels at least 1 cm above the plane horizontal to the upper edge of the superior thyroid pole; in type IIa, the distance is shorter than 1 cm and is not below the plane; in type IIb, the EBSLN is below the plane. EBSLN = external branch of the superior laryngeal nerve. |
|
|
|
Figure 2. Anatomic distances from the center of the cricoid cartilage to the distal insertion site of the EBSLN. a = height; b = width; c = oblique side; EBSLN = external branch of the superior laryngeal nerve. |
2.3. Statistical analyses
The relationships between EBSLN classification and patient demographic variables were evaluated using Fishers exact test and Pearsons Chi-square test. All statistical tests were performed at the 5% level of significance (p < 0.05) using the Statistical Package for the Social Sciences (SPSS) version 18.0 for Windows (SPSS Inc., Chicago, IL, USA).
3. Results
3.1. Demographic data and operative data
The mean patient age was 49.9 years (range, 22–77). There were 43 females and seven males in our study. The mean body mass index (BMI) of the patients was 25.58 ± 0.34 kg/m2 (range, 18.75–34.92). Forty-two total thyroidectomies and eight lobectomies were performed with IONM. There were four patients with benign disease, including two follicular adenomas and 46 patients with papillary thyroid carcinoma. The mean weight of the thyroid lobe was 9.7 ± 0.45 g (range, 2.20–22.70).
3.2. Anatomic distribution of the external branch of the superior laryngeal nerve
A total of 92 EBSLNs were evaluated and classified as either type I, IIa, or IIb according to Cernea classification. Type I EBSLN was observed in 15 of 92 nerves (16.3%), type IIa EBSLN in 52 (56.5%), and type IIb EBSLN in 25 (27.2%; Table 1). Incidences of types IIa and IIb EBSLNs, which put patients at greater risk for intraoperative injury, were more frequently observed (83.7%) in our study compared with previous Western studies. There was no distributional difference according to sex or between the right and left sides (p > 0.05). Type I EBSLN was more frequently observed in obese patients (BMI > 30) and in large glands (weight >15 g; p < 0.05). These results are shown in Table 2.
| Cernea classification | Each side | |
|---|---|---|
| Number | % | |
| Type I | 15 | 16.3 |
| Type IIa | 52 | 56.5 |
| Type IIb | 25 | 27.2 |
| Total | 92 | 100 |
EBSLN = external branch of the superior laryngeal nerve.
| EBSLN Classification | p value | |||
|---|---|---|---|---|
| Type I, n (%) | Type IIa, n (%) | Type IIb, n (%) | ||
| Right side | 9 (19.6) | 25 (54.3) | 12 (26.1) | 0.699 |
| Left side | 6 (13.0) | 27 (58.7) | 13 (28.3) | |
| Male | 3 (27.3) | 3 (27.3) | 5 (45.5) | 0.114 |
| Female | 12 (14.8) | 49 (60.5) | 20 (23.7) | |
| BMI < 30 | 9 (11.5) | 47 (60.3) | 22 (28.2) | 0.031* |
| BMI ≥ 30 | 4 (44.4) | 3 (33.3) | 2 (22.2) | |
| Lobe weight < 15 g | 8 (10.8) | 43 (58.1) | 23 (31.1) | 0.011* |
| Lobe weight ≥ 15 g | 4 (50.0) | 3 (37.5) | 1 (12.5) | |
- p < 0.05 is statistically significant.
BMI = body mass index; EBSLN = external branch of the superior laryngeal nerve.
3.3. Anatomic distances from the center of the cricoid cartilage to the distal insertion site of the EBSLN to the cricothyroid muscle
We measured the mean anatomic distances from the center of the cricoid cartilage to the distal site of the EBSLN. Height (a) was 3.53 ± 2.92 mm, the width (b) was 10.14 ± 4.41 mm, and an oblique side (c) was 11.81 ± 4.78 mm (Table 3). At the insertion sites of EBSLNs to the cricothyroid muscle, there were eight nerves (8.7%) within 5 mm, 25 (27.2%) within 5–10 mm, 55 (59.8%) within 10–20 mm, and four (4.3%) within 20–30 mm from the center of the cricoid cartilage. The 35.9% of insertion sites of the EBSLN (c) to the cricothyroid muscle were located within 1 cm from the center of the cricoid cartilage (Table 4).
| Value | Each side | |||
|---|---|---|---|---|
| Minimum (mm) | Maximum (mm) | Mean (mm) | Standard deviation (mm) | |
| Height (a) | 0.00 | 17.50 | 3.53 | 2.92 |
| Width (b) | 1.47 | 22.50 | 10.14 | 4.41 |
| Oblique side (c) | 1.88 | 25.20 | 11.81 | 4.78 |
EBSLN = external branch of the superior laryngeal nerve.
| Oblique side (C) | Each side | |
|---|---|---|
| Number | % | |
| <5 mm | 8 | 8.7 |
| 5 mm ≤ C < 10 mm | 25 | 27.2 |
| 55 | 59.8 | |
| 10 mm ≤ C < 20 mm | 4 | 4.3 |
| 20 mm ≤ C < 30 mm | 92 | 100 |
EBSLN = external branch of the superior laryngeal nerve.
4. Discussion
Cernea classification, which we used in this study, is one of the most popular worldwide classifications of the external branch of the superior laryngeal nerve.1 Another famous one is Kierner classification. Kierner et al2 classified the topographic variants of EBSLN into four types as follows: In type I, the EBSLN crosses the superior thyroid artery (STA) more than 1 cm above the upper pole of the thyroid; in type II, the EBSLN crosses the STA less than 1 cm above the upper pole of the thyroid gland; in type III, the EBSLN crosses the STA under the cover of the upper pole of the thyroid gland; and, in type IV, the EBSLN descends dorsally to the artery and crosses the branches of the STA immediately above the upper pole of the thyroid gland. Because Cernea and Kierner classifications are very similar, each type in Cernea classification, other than type IV, corresponds to a type in Kierner classification. Kierner et al2 emphasized that type IV has a high risk of injury during thyroidectomy due to the neighboring operative field of ligation of the STA.
In our study, types IIa and IIb EBSLN, which put patients at greater risk for injury during thyroidectomy, were observed in 77 (83.7%) of 92 nerves. Our findings are remarkably different from the previous Western studies. Cernea et al1 reported that 37% of all patients had either type IIa or IIb EBSLNs, while Kierner2 reported 44%, and Seven11 reported 48%. In Eastern studies, Aina12 reported 83.7% of patients with type IIa or IIb, and Chuang13 reported 77.8%, which is similar to our study findings. This difference may be relatively well explained by racial variations between Western and Eastern countries, although Pagedar et al14 reported 91% type IIa and IIb nerves of the total EBSLNs in their Western study (Table 5).
| Author | Race | EBSLN No. | Type ni (%) | Type I (%) | Type IIa (%) | Type IIb (%) | Risk group (%) (types IIa + IIb) |
|---|---|---|---|---|---|---|---|
| Cernea (1992) | Brazil | 30 | 3.0 | 60.0 | 17.0 | 20.2 | 37.0 |
| Kierner (1998) | Austria | 52 | 13.0 | 42.0 | 30.0 | 14.0 | 44.0 |
| Aina (2000) | 218 | 7.3 | 16.0 | 51.8 | 24.8 | 76.6 | |
| Malay | 106 | 17.9 | 61.3 | 20.8 | 82.1 | ||
| Chinese | 43 | 16.3 | 53.5 | 30.2 | 83.7 | ||
| Indian | 45 | 17.8 | 44.4 | 37.8 | 82.2 | ||
| Others | 8 | 12.5 | 62.5 | 25 | 87.5 | ||
| Hurtado-Lopez (2001) | Mexico | 84 | 6.0 | 16.7 | 41.7 | 35.7 | 77.4 |
| Bellantone (2001) | Italy | 459 | 11.6 | 58.6 | 19.6 | 10.2 | 29.8 |
| Furlan (2003) | Brazil | 72 | 47.0 | 31.0 | 22.0 | 52.0 | |
| Seven (2003) | Turkey | 60 | 10.0 | 51.8 | 37.1 | 11.1 | 48.2 |
| Mishra (2007) | Indian | 78 | 7.69 | 28.2 | 53.54 | 10.25 | 63.79 |
| Chuang (2008) | Chinese | 86 | 6.0 | 16.2 | 39.5 | 38.3 | 77.8 |
| Pagedar (2009) | Canadian | 178 | 7.3 | 42.7 | 48.3 | 91.0 | |
| Selvan (2009) | Indian | 70 | 20.0 | 8.6 | 2.9 | 68.5 | 71.4 |
| Present study (2011) | Korean | 92 | 16.3 | 56.5 | 27.2 | 83.7 |
EBSLN = external branch of the superior laryngeal nerve.
Furlan et al15 tried to identify some intrinsic risk factors that can enhance an iatrogenic injury of the EBSLN and suggested that individual stature and volume of the hemithyroid gland are probably involved in the risk of surgical EBSLN injury. Cernea et al1 also suggested that the size of the thyroid gland was probably related to the proximity of the EBSLN and the gland. Therefore, surgeons should be careful when operating on patients with a large goiter. In our study, there was no distributional difference according to sex or between the right and left sides (p > 0.05), but we cannot be sure whether there is no distributional difference according to sex because there is a big sex disequilibrium (male:female, 7:43). By contrast, type I in Cernea classification was more frequently observed in obese patients (BMI > 30) and in those with large glands (weight > 15 g) in our study. Our findings may have resulted from our small sample size as well as because our exclusion criteria included a large goiter or Graves disease.
Naidoo et al.16 examined the shortest distance from the most superior point of the thyroid gland to the EBSLN and emphasized the possibility of injury to the EBSLN during thyroidectomy. They recommended staying on the superior pole of the thyroid without going off the gland at all and even leaving a bit of the capsule of the superior pole of the thyroid gland. Selvan et al10 also measured the distance from the cricoid cartilage to the point of nerve entry into the cricoid muscle and used these data to produce a new EBSLN classification. Ozlugedik et al17 suggested that the knowledge of the relationship among the EBSLN, the inferior constrictor muscle, the oblique line of the thyroid cartilage, and the sternothyroid muscle will be useful for avoiding unexpected surgical complications.
We measured the distance from the center of the cricoid cartilage to the distal insertion point of the EBSLN to the cricoid muscle to demonstrate that the EBSLN innervates the cricothyroid muscle very close to the center of the cricoid cartilage in some cases. Recently, more surgeons have been using heat-induced devices like the Harmonic Scalpel (Ethicon Endo-Surgery Inc.) in thyroid surgery because these devices make it easy to dissect and ligate perithyroidal tissues (e.g., vessels, ligaments), and they also save operative time and provide surgical assistance for knot tying. During thyroidectomy, heat-induced devices can inadvertently be placed directly on the EBSLN, which has disastrous consequences. Therefore, surgeons should take care not to place the active blade of heat-induced devices on the EBSLN during surgical procedures. One such procedure is the dissection of the superior thyroid pole from the cricothyroid muscle by laterally retracting the thyroid. The other is when the thyroid is dissected from the pretracheal fascia after all complicated procedures are complete. The active blade tip of the device might not be clearly identified during these procedures, particularly in endoscopic and robotic settings. In our study, a noteworthy 35.9% of the insertion sites of the EBSLN to the cricothyroid muscle were located within 1 cm of the center of the cricoid cartilage.
IONM has been applied in various surgical procedures to reduce complications resulting from postoperative nerve palsy. The use of IONM has been expanded since Dralle et al18 ; 19 reported its effectiveness for identifying and preserving the recurrent laryngeal nerve during thyroid surgery in a large clinical study. However, the lack of a standardized procedure for IONM during thyroidectomy has led to highly variable results, and these results produce misleading information that has increased the risk of recurrent laryngeal nerve injury.20 As a result, an international standards guideline for IONM was proposed for the recurrent laryngeal nerve in 2011.21 Until now, there was no consensus for IONM of the EBSLN,8 ; 10 and many studies reported variable results for the identification rate of the EBSLN, ranging from 20% to 100%.10; 21 ; 22 We identified the EBSLNs in all patients and classified them according to the Cernea classification system. We stimulated the recurrent laryngeal nerve to confirm the absence of muscle paralysis before identifying the EBSLN and carrying out dissection of the cricothyroid muscle to further identify the EBSLN using IONM in cases without repetitive contraction of the cricothyroid muscle. The 0.5-mA stimulation was only used to identify the EBSLN and was not increased to avoid global contractions.10
Even now, the identification of the EBSLN during thyroidectomy is controversial, but many studies have emphasized the importance of identification of the EBSLN during thyroidectomy. Friedman et al4 suggested that the EBSLN should be explored during thyroid surgery, and identification is possible in most cases. Cernea et al1 also reported a lower injury rate in cases where the EBSLN was identified using IONM in their study of 76 patients. In a prospective, randomized, blinded, comparative study, Hurtado-Lopez et al23 divided their patients into three groups as follows: Group 1, thyroidectomies without intentionally searching for the EBSLN; Group 2, thyroidectomies searching intentionally for the nerve; and Group 3, the control group. They found that patients in Group 1 had more voice alterations compared with patients in Group 2 (14% vs. 8%) and demonstrated the importance of intraoperative identification of the EBSLN during thyroidectomy. The procedure may be more useful in populations at greater risk for EBSLN injury, especially Koreans, a population that has a higher frequency of Cernea types IIa and IIb. But most surgeons have still not routinely performed the identification of EBSLN during thyroidectomy because of its risk to harm postoperative voice outcome. So, IONM may be more useful in the identification of the EBSLN because it is less invasive and more easily to detect the location of EBSLN, especially in endoscopic or robotic settings.
Our study has many limitations. First, this study is too small to represent the entire Korean population. Second, we tried to minimize false-positive identifications of EBSLNs by using low amplitude stimulation and dissection of the cricothyroid muscle in cases without repetitive contractions, but there is a possibility of false positivity in identifying the EBSLN. Third, it is difficult to compare our results with those of other studies because there are no international standardization guidelines for the EBSLN. Notwithstanding these limitations, to the best of our knowledge, this study was the first to identify and classify EBSLNs using IONM in Koreans and one of a few to present eastern data regarding the EBSLN. Moreover, the data on distal innervation site of EBSLN is extremely unique and worthy in worldwide.
Our results may help surgeons understand the anatomy of the EBSLN in Koreans and to preserve the nerve during thyroidectomy. In the near future, IONM of the EBSLN during thyroidectomy may become a standard procedure, especially in Koreans.
5. Conclusion
Surgeons should pay more attention to preservation of the EBSLN during thyroidectomy in Korean patients because EBSLNs in Koreans are more frequently located beneath the superior thyroid vessels. Intraoperative neuromonitoring may help to identify the external branch of the superior laryngeal nerve.
References
- 1 C.R. Cernea, S. Nishio, F.C. Hojaij; Identification of the external branch of the superior laryngeal nerve (EBSLN) in large goiters; Am J Otolaryngol, 16 (1995), pp. 307–311
- 2 A.C. Kierner, M. Aigner, M. Burian; The external branch of the superior laryngeal nerve: its topographical anatomy as related to surgery of the neck; Arch Otolaryngol Head Neck Surg, 124 (1998), pp. 301–303
- 3 T.I. Abelson, H.M. Tucker; Laryngeal findings in superior laryngeal nerve paralysis: a controversy; Otolaryngol Head Neck Surg, 89 (1981), pp. 463–470
- 4 M. Friedman, P. LoSavio, H. Ibrahim; Superior laryngeal nerve identification and preservation in thyroidectomy; Arch Otolaryngol Head Neck Surg, 128 (2002), pp. 296–303
- 5 B.J. Teitelbaum, B.L. Wenig; Superior laryngeal nerve injury from thyroid surgery; Head Neck, 17 (1995), pp. 36–40
- 6 X. Kochilas, A. Bibas, J. Xenellis, S. Anagnostopoulou; Surgical anatomy of the external branch of the superior laryngeal nerve and its clinical significance in head and neck surgery; Clin Anat, 21 (2008), pp. 99–105
- 7 H. Gray, P.L. Williams, L.H. Bannister; Grays Anatomy: The Anatomical Basis of Medicine and Surgery; (38th ed.)Churchill Livingstone, New York (1995)
- 8 W.B. Inabnet, T. Murry, S. Dhiman, J. Aviv, J.C. Lifante; Neuromonitoring of the external branch of the superior laryngeal nerve during minimally invasive thyroid surgery under local anesthesia: a prospective study of 10 patients; Laryngoscope, 119 (2009), pp. 597–601
- 9 G. Dionigi, L. Boni, F. Rovera, A. Bacuzzi, R. Dionigi; Neuromonitoring and video-assisted thyroidectomy: a prospective, randomized case-control evaluation; Surg Endosc, 23 (2009), pp. 996–1003
- 10 B. Selvan, S. Babu, M.J. Paul, D. Abraham, P. Samuel, A. Nair; Mapping the compound muscle action potentials of cricothyroid muscle using electromyography in thyroid operations: a novel method to clinically type the external branch of the superior laryngeal nerve; Ann Surg, 250 (2009), pp. 293–300
- 11 H. Seven, A.B. Calis, C. Vural, S. Turgut; Microscopic thyroidectomy: a prospective controlled trial; Eur Arch Otorhinolaryngol, 262 (2005), pp. 41–44
- 12 E.N. Aina, A.N. Hisham; External laryngeal nerve in thyroid surgery: recognition and surgical implications; ANZ J Surg, 71 (2001), pp. 212–214
- 13 F.J. Chuang, J.Y. Chen, J.F. Shyu, et al.; Surgical anatomy of the external branch of the superior laryngeal nerve in Chinese adults and its clinical applications; Head Neck, 32 (2010), pp. 53–57
- 14 N.A. Pagedar, J.L. Freeman; Identification of the external branch of the superior laryngeal nerve during thyroidectomy; Arch Otolaryngol Head Neck Surg, 135 (2009), pp. 360–362
- 15 J.C. Furlan, A.C. Cordeiro, L.G. Brandao; Study of some "intrinsic risk factors" that can enhance an iatrogenic injury of the external branch of the superior laryngeal nerve; Otolaryngol Head Neck Surg, 128 (2003), pp. 396–400
- 16 D. Naidoo, J.M. Boon, C.J. Mieny, P.J. Becker, A.N. van Schoor; Relation of the external branch of the superior laryngeal nerve to the superior pole of the thyroid gland: an anatomical study; Clin Anat, 20 (2007), pp. 516–520
- 17 S. Ozlugedik, H.I. Acar, N. Apaydin, I. Tekdemir, A. Elhan, A. Comert; Surgical anatomy of the external branch of the superior laryngeal nerve; Clin Anat, 20 (2007), pp. 387–391
- 18 H. Dralle, C. Sekulla, K. Lorenz, M. Brauckhoff, A. Machens, I.S.G. German; Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery; World J Surg, 32 (2008), pp. 1358–1366
- 19 H. Dralle, C. Sekulla, J. Haerting, et al.; Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery; Surgery, 136 (2004), pp. 1310–1322
- 20 F.Y. Chiang, K.W. Lee, H.C. Chen, et al.; Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation; World J Surg, 34 (2010), pp. 223–229
- 21 C. Page, M. Laude, D. Legars, P. Foulon, V. Strunski; The external laryngeal nerve: surgical and anatomic considerations. Report of 50 total thyroidectomies; Surg Radiol Anat, 26 (2004), pp. 182–185
- 22 J. Jonas, R. Bahr; Neuromonitoring of the external branch of the superior laryngeal nerve during thyroid surgery; Am J Surg, 179 (2000), pp. 234–236
- 23 L.M. Hurtado-Lopez, M.I. Pacheco-Alvarez, L. Montes-Castillo Mde, F.R. Zaldivar-Ramirez; Importance of the intraoperative identification of the external branch of the superior laryngeal nerve during thyroidectomy: electromyographic evaluation; Thyroid, 15 (2005), pp. 449–454
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?