Summary
Hepatocellular carcinoma (HCC) occurring in pregnancy is very rare. The prognosis is usually poor because of unclear clinical presentation. A 30-year-old woman who suffered from HCC during pregnancy underwent hepatectomy twice, and resection for pulmonary metastasis once. A healthy infant was delivered after the first hepatectomy. Currently, she remains disease free 55 months after the second hepatectomy and 39 months after pulmonary metastatectomy. Moreover, she had another healthy infant 37 months after pulmonary metastatectomy. Aggressive resection of recurrent HCC may prolong life, and pregnancy should not alter the treatment strategy for HCC.
Keywords
hepatocellular carcinoma;pregnancy;surgical resection
1. Introduction
Cancer in pregnancy is rare and coexistence of hepatocellular carcinoma (HCC) with pregnancy is extremely rare.1 HCC in pregnancy is usually asymptomatic at the early stages and is therefore beyond diagnosis and therapy at presentation. Liver resection remains the main therapeutic option for HCC, but the recurrence rate is still high.2
For HCC in pregnancy, resection of tumor without termination of pregnancy has been suggested.3 However, no long-term survival after recurrence of HCC in pregnancy has been reported to the best of our knowledge. Herein, we report a rare case of a woman with HCC during pregnancy who underwent hepatectomy twice and resection for pulmonary metastasis once. She had long-term survival and had a second healthy delivery after treatment of HCC.
2. Case report
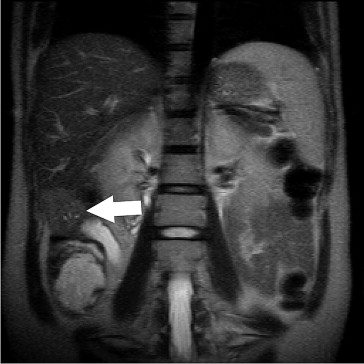
A 30-year-old woman presented with her first pregnancy at 25 weeks gestation. She received routine pregnancy check-up and abdominal ultrasonography incidentally revealed a tumor mass over the right lobe of the liver. She was seronegative for both hepatitis B and C viruses. The maternal serum α-fetoprotein was 305 ng/mL (normal range: < 12 ng/mL). Magnetic resonance imaging showed a 42-mm hepatic mass with an irregular margin at the inferior part of segment (S)6 (Fig. 1). We performed subsegmentectomy of S6 and cholecystectomy at 26 weeks gestation. No cirrhosis was found during the operation. The pathology reported an HCC, which was poorly differentiated, with a free resection margin. The patient recovered uneventfully and was discharged home on postoperative day 8.
|
|
|
Figure 1. Magnetic resonance imaging showed a 42-mm hepatic mass in the inferior part of segment 6, with a slightly high signal on no-fat-saturated T2-weighted imaging (arrow). |
Abdominal ultrasonography at 39 weeks gestation showed a hypoechoic tumor, 33 mm in size over the right lobe of the liver. A male infant weighing 3.396 kg was delivered by Cesarean section due to dysfunctional labor, which was performed at gestational week 41. One week later, computed tomography showed a lobulated hypervascular mass about 47 mm in S7 of the liver (Fig. 2). Wedge resection of S7 was carried out one month after delivery with an uneventful recovery.
|
|
|
Figure 2. Computed tomography showed a hypervascular mass, 47 mm in size, over segment 7 of the liver (arrow). |
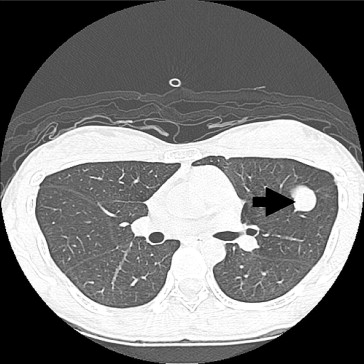
During the following period, the serum α-fetoprotein level was within the normal range. However, a well-defined nodule, 7 mm in size over the lingular segment of the left lung was noted by chest computed tomography 14 months after the previous operation (Fig. 3). Wedge resection of the anterior segment of the left lung was performed. The pathology reported the nodule as metastatic HCC.
|
|
|
Figure 3. Computed tomography showed a well-defined nodule, 7 mm in size, over the upper lobe of the left lung (arrow). |
The patient was pregnant again 29 months after lung resection and a healthy male infant was delivered at gestational week 36. At present, the patient remains free of HCC 55 months after the second hepatectomy and 39 months after pulmonary metastatectomy.
3. Discussion
HCC during pregnancy is a rare event, and only 48 cases have been reported in the literature since 1957.4 The risk factors are African descent, cirrhosis, positivity for hepatitis B surface antigen, multiparity, and a family history of HCC with long-term usage of oral contraceptives.5 ; 6 It has been reported that the 3-year survival rate and the median survival of HCC in pregnancy are only 13.6% and 18 months, respectively.4 As a result of poor prognosis of HCC in pregnancy, past reports have emphasized the need for termination of pregnancy as part of treatment.1 ; 7
The treatment strategy for HCC includes surgery, transarterial chemoembolization, systemic chemotherapy, radiofrequency ablation, and ethanol injection. Liver resection has been a main treatment for HCC, although the recurrence rate is high.2 ; 4 Currently, repeat hepatectomy seems to be a better choice for recurrent HCC.8 However, to the best of our knowledge, no long-term survival of recurrent HCC in pregnancy has been reported in the literature.
The most common site of extrahepatic recurrence of HCC is the lung. HCC during pregnancy with distant metastasis had been reported in 8/40 patients and the prognosis was poor.1 ; 4 However, pulmonary resection for metastatic HCC, as long as there is no concurrent cancer or other recurrence, could provide long-term survival.9 We suggest performing pulmonary metastatectomy to achieve long-term survival.
If recurrent HCC is noted in the third trimester of pregnancy, resection may be favored after delivery because the complications of anesthesia are potentiated due to pregnancy-related changes in physiology.10
In our case, the patient did not have any of the aforementioned risk factors. She was adamant about continuing the pregnancy and we performed curative resection at 26 weeks gestation. Although liver recurrence and pulmonary metastasis were found, respective R0 resections were done. Thirty-nine months after lung resection, there was no evidence of further recurrent tumor. Moreover, the patient became pregnant again 29 months after lung resection. The infants have done well. When physicians keep the safety of the fetus in mind and work in cooperation with gynecologists, we believe that pregnancy should not alter the treatment strategy for HCC.
Herein, we recommend that treatment for HCC during pregnancy should be similar to that for nonpregnant women. Complete excision of tumor without termination of pregnancy, even if there is liver recurrence and pulmonary metastasis, provides the greatest chance of survival for women with HCC during pregnancy. Moreover, there is also no evidence of contraindication for another pregnancy.
References
- 1 F.C. Cobey, R.R. Salem; A review of liver masses in pregnancy and a proposed algorithm for their diagnosis and management; Am J Surg, 187 (2004), pp. 181–191
- 2 C.C. Wu, S.B. Cheng, W.M. Ho, et al.; Liver resection for hepatocellular carcinoma in patients with cirrhosis; Br J Surg, 92 (2005), pp. 348–355
- 3 P. Gisi, R. Floyd; Hepatocellular carcinoma in pregnancy. A case report; J Reprod Med, 44 (1999), pp. 65–67
- 4 K.K. Choi, Y.J. Hong, S.B. Choi, et al.; Hepatocellular carcinoma during pregnancy: is hepatocellular carcinoma more aggressive in pregnant patients?; J Hepatobiliary Pancreat Sci, 18 (2011), pp. 422–431
- 5 M. Alvarez de la Rosa, D. Nicolás-Pérez, J.R. Muñiz-Montes, et al.; Evolution and management of a hepatocellular carcinoma during pregnancy; J Obstet Gynaecol Res, 32 (2006), pp. 437–439
- 6 W.Y. Lau, W.T. Leung, S. Ho, et al.; Hepatocellular carcinoma during pregnancy and its comparison with other pregnancy-associated malignancies; Cancer, 75 (1995), pp. 2669–2676
- 7 L.B. Jeng, W.C. Lee, C.C. Wang, et al.; Hepatocellular carcinoma in a pregnant woman detected by routine screening of maternal alpha-fetoprotein; Am J Obstet Gynecol, 172 (1995), pp. 219–220
- 8 C.C. Wu, S.B. Cheng, D.C. Yeh, et al.; Second and third hepatectomies for recurrent hepatocellular carcinoma are justified; Br J Surg, 96 (2009), pp. 1049–1057
- 9 C.M. Lam, C.M. Lo, W.K. Yuen, et al.; Prolonged survival in selected patients following surgical resection for pulmonary metastases from hepatocellular carcinoma; Br J Surg, 85 (1998), pp. 1198–1200
- 10 A. Jadon; Complications of regional and general anaesthesia in obstetric practice; Indian J Anaesth, 54 (2010), pp. 415–420
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?