Summary
Esophagogastroduodenoscopy (EGD) is regarded as a relatively safe procedure; however, it carries a very low incidence of severe adverse events. Perforation is a rare complication of EGD, and it may further lead to pneumoperitoneum or pneumoretroperitoneum. The occurrence of large bowel perforation after EGD is extremely rare, and it has never been reported in the international literature. Herein, we present a case of concurrence of pneumoperitoneum and pneumoretroperitoneum as a result of sigmoid perforation after EGD. In our case, the probable mechanism of the perforation may have stemmed from the excessive inflation of air that passed through the gastrointestinal tract to the sigmoid colon, causing the increased intraluminal pressure, and then prompting a healed asymptomatic diverticulitis leak again.
Keywords
Esophagogastroduodenoscopy ; Large bowel ; Perforation ; Pneumoperitoneum ; Pneumoretroperitoneum
Introduction
Esophagogastroduodenoscopy (EGD) is commonly performed to diagnose gastrointestinal diseases, and it carries a low risk of adverse events, including cardiopulmonary adverse events, infection, perforation, and bleeding [1] . Perforation may occur at the esophagus, stomach, or duodenum and further lead to pneumoperitoneum or pneumoretroperitoneum; however, the occurrence of large bowel perforation after EGD is extremely rare and has never been reported in the international literature. We report a patient who presented with pneumoretroperitoneum and pneumoperitoneum, caused by a perforated sigmoid diverticulum, after undergoing EGD.
Case report
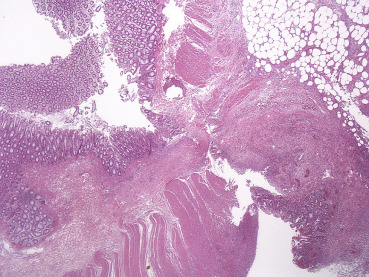
A 75-year-old woman presented with once blood-tinged stool passage a few hours prior to admission. No exaggerating factor, relieving factor, or associated symptom was reported. The patient had no associated family history and denied consuming alcohol or tobacco. She had been diagnosed to have coronary artery disease 10 years ago, and she has been receiving antiplatelet therapy with clopidogrel regularly since then. At admission, physical examination revealed normal vital signs and pale conjunctiva, but no abdominal tenderness was shown. Laboratory tests showed the following results: hemoglobin, 10.3 g/dL (normal range, 12.0–15.0 g/dL); platelet, 296,000/mm3 (150,000–350,000/mm3 ); white blood cell count, 17,230/mm3 (5000–13,000/mm3 ); prothrombin time, 10.7 seconds (International Normalized Ratio, 1.06 seconds); high sensitivity C-reactive protein, 13.124 mg/dL (0–0.748 mg/dL). Her plain abdominal X-ray scan showed normal bowel gas pattern (Fig. 1 ). EGD revealed no active bleeding lesion in the upper gastrointestinal tract. A few hours after the EGD, she experienced a sudden onset of abdominal pain and the pain was progressing. Her physical examination revealed diffuse tenderness over the abdomen and mild rebounding pain. The abdominal ultrasonography showed negative findings. The abdominal computed tomography revealed significant pneumoretroperitoneum and pneumoperitoneum; multiple outpouchings of the intestine with adjacent fat stranding were found along the sigmoid colon (Fig. 2 ). The patient received open laparotomy, and a whole-layered perforation from a sigmoid diverticulum was identified (Fig. 3 ). The pathology report showed acute diverticulitis with perforation (Fig. 4 ). She received critical care in intensive care unit postoperatively, and recovered uneventfully.
|
|
|
Figure 1. Plain abdominal X-ray shows normal bowel gas pattern. |
|
|
|
Figure 2. (A) Transverse view of abdominal computed tomography shows multiple outpouching structures (arrows) along sigmoid colon with adjacent fat stranding. (B) Coronal view of abdominal computed tomography shows significant pneumoretroperitoneum (arrow) and pneumoperitoneum (arrowhead). |
|
|
|
Figure 3. Gross examination of the specimen of segmental resection of the sigmoid colon shows a small spherical outpouching along the intestinal wall, measuring 1.5 cm × 0.9 cm × 0.9 cm, with the section of the diverticula penetrating through the muscular layer into epiploic appendage. |
|
|
|
Figure 4. Pathology report shows acute diverticulitis with perforation. |
Discussion
Perforation of the upper gastrointestinal tract is a rare complication of EGD, and it may further lead to peritonitis or mortality if diagnosis is delayed. Unusual abdominal pain after endoscopic examination and the appearance of intra-abdominal extraluminal air may indicate gastrointestinal tract perforation, and early diagnosis leads to a better outcome.
Pneumoperitoneum is the presence of air or gas in the peritoneal cavity. By contrast, pneumoretroperitoneum is the presence of air or gas in the retroperitoneal space, and usually indicates a perforation of gut facing retroperitoneal tissue. This event was reported to be a complication of endoscopic retrograde cholangiopancreaticography or colonoscopy; however, it rarely happened after routine EGD [2] . So far, only less than five cases [2] ; [3] ; [4] ; [5] had been reported in the international literature as pneumoretroperitoneum with no evidence of gut perforation after an EGD examination. To the authors’ knowledge, there has been no reported case of large bowel perforation after a routine EGD. In this case, the patient presented with a concurrence of pneumoperitoneum and pneumoretroperitoneum as a result of sigmoid perforation after EGD.
A plain abdominal X-ray can show classic pneumoretroperitoneum and pneumoperitoneum in the case of extreme gas emission. An abdominal computed tomography scan can display small amounts of free air, and it is the most sensitive examination for diagnosis. Ultrasonography examination is a noninvasive examination and can provide many diagnostic findings in real time, but it is relatively dependent on a skilled operator and experience in diagnosing free air in peritoneum and retroperitoneum.
Endoscopy-related viscus perforation can be caused by different mechanisms. Traumatic perforation is usually associated with interventional procedures (e.g., biopsy, polypectomy, mucosal resection or submucosal dissection [6] ) and is less commonly associated with a direct instrument tear or penetration [7] . Pneumatic perforation is the consequence of high-pressure insufflations, resulting in excessive distension of the bowel wall and rupture. Perforation commonly occurs at points of previous lesions or a weak point of the bowel such as diverticula with or without diverticulitis, inflammation, neoplastic processes, or scar of recent operations [8] . Katz et al [9] proposed a mechanism of air dissection through the bowel wall without perforation: the air might initially be forced through weak points in the mucosa, tracking along perineural planes and vascular sheaths to reach the peritoneal cavity or extraperitoneal tissue. In our case, the probable mechanism of the perforation may be the excessive inflation of air that passed through the gastrointestinal tract to the sigmoid colon, thereby causing increased intraluminal pressure, and then prompting a healed asymptomatic diverticulitis to leak again.
In conclusion, the occurrence of large bowel perforation after EGD is extremely rare. It would be prudent to look for occult lesions in the lower gastrointestinal tract (e.g., diverticulitis) if an unusual complication occurs after a routine EGD that does not yield any remarkable finding.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] T. Ben-Menachem, G.A. Decker, D.S. Early, J. Evans, R.D. Fanelli, D.A. Fisher, et al.; Adverse events of upper GI endoscopy; Gastrointest Endosc, 76 (2012), pp. 707–718
- [2] W.C. Martin, N. Nagai, W. Diner, E.C. Texter Jr.; Benign retroperitoneal emphysema associated with upper gastrointestinal endoscopy; Arch Intern Med, 138 (1978), pp. 759–761
- [3] D. Katz, S. Selesnick; Massive pneumoperitoneum and pneumoretroperitoneum after gastroscopy; report of a case and review of the literature; Am J Dig Dis, 1 (1956), pp. 512–520
- [4] A. Girardi, I. Piazza, G. Giunta, G. Pappagallo; Retroperitoneal, mediastinal and subcutaneous emphysema as a complication of routine upper gastrointestinal endoscopy; Endoscopy, 22 (1990), pp. 83–84
- [5] Z. Fireman, J. Bar-Ziv, B. Lurie; Retroperitoneal, mediastinal, and subcutaneous emphysema as a complication of routine upper gastrointestinal endoscopy; Endoscopy, 26 (1994), pp. 329–330
- [6] S. Siboni, D. Bona, E. Abate, L. Bonavina; Tension pneumoperitoneum following endoscopic submucosal dissection of leiomyoma of the cardia; Endoscopy, 422 (2010), p. E152
- [7] S.J. Taub, C. Nagurka, J.B. Raskin; Tension pneumoperitoneum as a nontraumatic complication of upper gastrointestinal endoscopy; Gastrointest Endosc, 26 (1980), pp. 153–154
- [8] N.S. Park, J.H. Choi, D.H. Lee, Y.J. Kim, E.S. Kim, S.W. Jung, et al.; Pneumoretroperitoneum, pneumomediastinum, peumopericardium, and subcutaneous emphysema after colonoscopic examination; Gut Liver, 1 (2007), pp. 79–81
- [9] D. Katz, R. Cano, M. Antonelle; Benign air dissection of the esophagus and stomach at fiberesophagoscopy; Gastrointest Endosc, 19 (1972), pp. 72–74
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?