Summary
Objective
Laparoendoscopic single-site (LESS) adrenalectomy is a promising minimally invasive technique, however, the current evidence has not confirmed its long-term effectiveness in primary aldosteronism (PA). We conducted a study to analyze the long-term efficacy of LESS adrenalectomy in patients with PA.
Methods
A total of 49 patients who had been clinically confirmed with PA who had an indication for unilateral adrenalectomy were included in this study. Perioperative data were obtained for all patients. Blood pressure and the levels of serum aldosterone, renin, and potassium were checked periodically. The median follow-up was 16.5 months.
Results
No intra- or early post-operative complication occurred. All LESS adrenalectomies were completed successfully, except one with laparoscopic conversion. Hypokalemia was resolved in all cases and no patient required potassium supplements after surgery. Post-operative cure of hypertension was achieved in 63% of our patients. Overall, 84% of our PA patients had clinical improvement in blood pressure control after surgery.
Conclusions
Our long-term experience revealed that LESS adrenalectomy is a safe and effective approach, which demonstrated comparable long-term cure and improvement of hypertension to a conventional laparoscopic series in treating PA.
Keywords
primary aldosteronism;laparoendoscopic single-site surgery;adrenalectomy
1. Introduction
Primary aldosteronism (PA) is one of the few surgically curable causes of hypertension. PA is usually caused by aldosterone-secreting adenomas (APA) in the unilateral or bilateral adrenal gland, however, it may also be caused by small hyperplastic or multiple nodular lesions. According to a screening study in Japan, PA is found in 3.3–10% of hypertensive patients and is the most common cause of secondary hypertension.1; 2 ; 3 To date, unilateral adrenalectomy is still the treatment of choice in patients with APA and unilateral hyperplasia.
Laparoscopic adrenalectomy has become the recommended procedure for unilateral APA or hyperplasia due to less postoperative pain and shorter convalescence when compared with its open surgery counterpart.4 ; 5 A recent revolution in surgery, the laparoendoscopic single-site surgery (LESS), has been widely implemented in various surgical indications including adrenalectomy.6; 7; 8; 9; 10; 11; 12 ; 13 Preliminary results have revealed comparable safety and efficacy in removing benign adrenal lesions to the conventional laparoscopic approach, but with additional clinical benefits of less postoperative pain, and a shorter hospital stay.14 ; 15
Among a larger series of LESS adrenalectomies, APA is the most common surgical indication, comprising up to 50% of all cases.11; 16; 17 ; 18 However, as a promising and emerging minimally invasive technique, the current evidence has not confirmed its long-term effectiveness in this most common surgical indication. Therefore, we conducted a study to analyze the long-term efficacy of LESS adrenalectomy in patients with PA.
2. Materials and methods
2.1. Patients
We maintain a prospective database of all LESS performed in our department, including LESS adrenalectomy since January 2007. This study is a retrospective review of prospectively collected data from this database.
Between October 2009 and October 2014, 105 LESS adrenalectomies were performed by a single surgeon (YCT) who is experienced in laparoscopic adrenalectomy. We shifted our adrenalectomy to the LESS approach in 2009, except in cases with a tumor size >6 cm where the risk of malignancy is high, or cases with a body mass index (BMI) > 45 because of difficulty in maintaining pneumoperitoneum under a single port design. Based on this database, we identified 49 patients who had been clinically confirmed (by saline infusion and captopril tests) to have PA to be included in this study. Those PA patients who had inconclusive abdominal contrast-enhanced computed tomography (CT) results underwent adrenal scintigraphy using 131I-6 b-iodomethyl-19-norcholesterol (NP-59) SPECT/CT and/or adrenal venous sampling (AVS) for lateralization. The baseline characteristics of these 49 patients are listed in Table 1.
| No. of patients | 49 |
|---|---|
| Age (y) | 50.8 (11.5) |
| Sex (M:F) | 28/21 |
| BMI | 27.8 (7.2) |
| Operative time (min) | 112.7 (52.3) |
| Specimen weight (g) | 18.6 (9.3) |
| Right/left side tumor | 22/27 |
| Histopathology | |
| Adrenocortical adenoma (APA) | 47 |
| Nodular adrenal hyperplasia | 1 |
| Hyperplasia (IHA) | 1 |
| Median follow up (mo), (range) | 16.5 (3–60) |
| No. lost to follow up (%) | 3 (6.1) |
Data expressed as mean (SD) or absolute number of patients.
APA = aldosterone-secreting adenomas; BMI = body mass index; F = female; IHA = idiopathic hyperaldosteronism; M = male; SD = standard deviation.
2.2. Operative technique
After induction of general anesthesia, the patient was placed in the prone jack-knife position. LESS adrenalectomy starts with a 2.0–3.0-cm skin incision just beneath the tip of the 12th rib. The subcutaneous tissues and fascia were dissected sharply. Using blunt finger dissection, the retroperitoneal space was created for the single-port placement. A homemade or commercial single port was placed in position through the incision.13 The capnoretroperitoneum is created by a carbon dioxide pressure of 15–20 mmHg. After pneumoretroperitoneum was established, a rigid 5-mm, 30° laparoscope and conventional 5-mm laparoscopic instruments were used for subsequent manipulation. Step-by-step, after creation of the retroperitoneal space by blunt dissection, the upper pole of the kidney was mobilized. Dissection of the adrenal gland started from medial side of the adrenal gland. For the right adrenal tumors, the adrenal arteries which cross the vena cava medially posteriorly were separated using a 5-mm LigaSure V Sealer/Divider (Covidien, Valleylab, Boulder, CO, USA). The short adrenal vein was then located, controlled, and transected using LigaSure (Covidien). Then, the right adrenal gland was completely mobilized by lateral and cranial dissection. For the left-sided adrenalectomy, dissection started from the inferior, medial border of the adrenal gland which is just above the anatomic landmark of the left renal artery. Then, the main left adrenal vein was identified, controlled, and transected using LigaSure (Covidien). After that, an extended mobilization of the upper pole of the kidney was performed. Thereafter, the inferior part of the gland could be identified and dissected. Both adrenal glands with the surrounding fatty tissue were removed in an en bloc manner and the completely mobilized specimen was placed in a retrieval bag.
2.3. Follow up
The median follow up was 16.5 months. Most of the patients returned to the clinic for follow up, except three patients who were lost to follow up after 3 months. Blood pressure and the levels of serum aldosterone, renin, and potassium were checked periodically. Postadrenalectomy clinical outcomes were judged on the basis of improvement of hypertension and hypokalemia. Hypertension was considered cured if blood pressure decreased to ≤140/90 mmHg shortly after adrenalectomy and antihypertensive medications were not required during the 1st year after adrenalectomy. Patients whose hypertension subsided within the 1st year but later returned were still classified as cured. Hypokalemia was considered resolved if serum potassium levels remained normal without potassium supplementation.
2.4. Statistical analysis
Summaries of continuous variables were calculated as the mean ± standard deviation. Continuous variables were tested for normality using the Shapiro–Wilks test. The Mann–Whitney U-test or the independent samples t-test was used for continuous variables depending on the normality of the variable. A p value < 0.05 was considered statistically significant. The learning and cumulative curve were generated with logarithmic regression model using SPSS computer software. Statistical analyses were performed using SPSS for Windows (Version 18.0, PASW, SPSS, Inc., Chicago, IL, USA).
3. Results
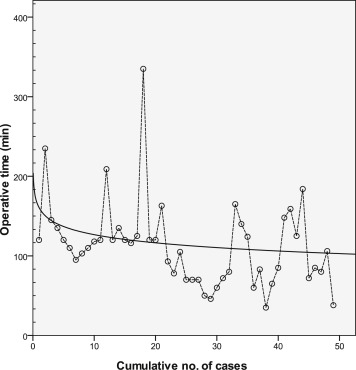
The perioperative outcomes are summarized in Table 1 ; Table 2. No conversions to open adrenalectomy were necessary and only one super-obese female patient (BMI > 45) was converted to a conventional laparoscopic approach due to inability to maintain a reasonable retroperitoneal space during the LESS retroperitoneal approach. The median operative time was 112.5 minutes with a range from 35 minutes to 237 minutes. The learning curve demonstrated in Figure 1 revealed a short learning period, whereby most of the learning occurs in the first 15–20 cases. Our learning curve became linear after the first 20 cases. The mean operative time revealed a significant reduction from 140.5 ± 56.7 minutes to 93.4 ± 40.9 minutes after the learning period (first 20 cases; p < 0.0001; Figure 1). The blood loss was minimal (<50 mL) in all cases. All cases had his/her adrenal tumor removed en bloc with its adrenal gland and had at least one main adrenal vein identified.
| No. of patients | |
|---|---|
| Conversion to conventional laparoscopy (%) | 1 (2) |
| Late postoperative complication | |
| Chronic wound pain | 1 |
| Erectile dysfunction | 2 |
| Total (%) | 3 (2) |
| Mean time to oral intake (day) | 0.2 (0.2) |
| Mean hospital stay (d) | 2.2 (.8) |
| Return to normal daily activity (d), (mean) | 3.9 (4.6) |
| Overall satisfaction with surgery (on POD 7) (%) | |
| Extremely satisfied | 31 (63) |
| Satisfied | 12 (25) |
| Average | 5 (10) |
| Unsatisfied | 1 (2) |
| Extremely unsatisfied | 0 |
Data expressed as mean (SD) or absolute no. of patients unless otherwise stated.
POD = postoperative day; SD = standard deviation.
|
|
|
Figure 1. Scatter plot (dash line) and learning curve (solid line) of operative time. |
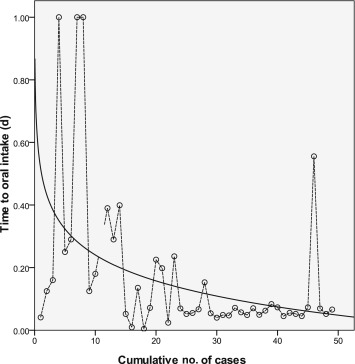
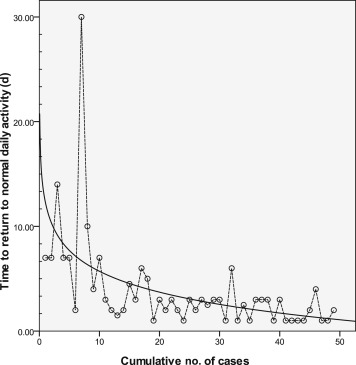
No intraoperative or early postoperative complications occurred. Three patients experienced late complications, one experienced chronic wound pain after 6 months after the operation and the other two experienced erectile dysfunction up to 6 months of follow up, which was improved by oral phosphodiesterase Type 5 inhibitors (Table 2). The learning curve also impacted patients' convalescence significantly. The time required for resumption of oral intake revealed a significant improvement after the learning period (0.3 ± 0.3 days vs. 0.1 ± 0.1 days; p < 0.0001; Figure 2) Improvement in convalescence was also noted in the time to return normal activity with a mean of 6.3 ± 6.4 days during learning period and a mean of 2.2 ± 1.2 days after learning (p < 0.0001; Figure 3). The majority of the patients (88%) were satisfied or extremely satisfied with the surgical results (Table 2).
|
|
|
Figure 2. Scatter plot (dash line) and cumulative curve (solid line) of time to oral intake after LESS adrenalectomy. LESS = laparo-endoscopic single-site. |
|
|
|
Figure 3. Scatter plot (dash line) and cumulative curve (solid line) of time to return to normal activity after LESS adrenalectomy. LESS = laparo-endoscopic single-site. |
Postoperative cure of hypertension (29/46 patients; normotensive without antihypertensive medication) or significant improvement of hypertension (10/46 patients; normotensive with less antihypertensive medication when compared with preoperative status) was confirmed in 39/46 (84.8%) patients (Table 3). Hypokalemia was resolved in all patients and no patient required potassium supplements after surgery. Biochemical sign (ARR > 35) of PA was found in four (8.9%) patients at a follow up of 6 months. The laterality of all these four patients had been confirmed by NP-59 SPECT/CT scan of AVS preoperatively. One of them was confirmed to have idiopathic hyper-aldosteronism according to the postoperative histological study.
| No. of patients (%) | |
|---|---|
| Mean aldosterone:rennin ratio (SD) ng/dL per ng/mL/h (SD) | |
| Preoperative | 169.66 (361.40) |
| Postoperative | 18.48 (26.28) |
| Blood pressure control after operation (%) | |
| Normotensive without medication (cure) | 29 (63) |
| Normotensive with medication | 10 (21.4) |
| Hypertensive | 7 (15.6) |
| No. of hypokalemic patients (%) | |
| Before operation | 30 (61.2) |
| After operation (without supplementation) | 0 (0) |
Data expressed as mean (SD) or absolute no. (%) of patients.
LESS = laparo-endoscopic single-site; SD = standard deviation.
4. Discussion
LESS adrenalectomy is one of the most promising LESS procedures, because neither time consuming reconstruction nor further enlargement of the surgical incision is required with a single small 2–3 cm incision for LESS. Several preliminary and comparative studies revealed its safety and feasibility in removing benign functional/nonfunctional adrenal tumors.11; 16; 17; 18; 19 ; 20 Among these early series, APA and unilateral hyperplasia is the most common indication for LESS adrenalectomy. However, most of these early reports focus on perioperative outcomes and procedure related complications. Only two comparative studies mentioned their functional outcome of PA, and their follow-up periods were either extremely short or unknown.18 ; 20 Therefore, reports regarding functional outcomes in PA patients who underwent LESS adrenalectomy were either scarce or inadequate. Although it is one of the most common indications of LESS adrenalectomy, its functional effectiveness in PA is still underdeveloped.
To the best of our knowledge, this is the first study reporting the long-term functional outcomes of LESS adrenalectomy in PA patients. In our series, cure of hypertension was defined if blood pressure decreased to ≤140/90 mmHg after adrenalectomy and patients were free from antihypertensive medication within the 1st year of treatment. The cure rate was as high as 63% in our long-term follow up. This result is compatible with those open and laparoscopic counterparts who have an overall cure rate of 60% with a compatible definition of “cure”.21 In addition, our results revealed that blood pressure could be normalized with antihypertensive medications in another 21% of our PA patients (Table 3). Overall, 84% of our PA patients had clinical improvement in blood pressure control after their LESS adrenalectomy. In addition, preoperative hypokalemia patients were all resolved in the early postoperative phase. Therefore, the long-term effectiveness of LESS adrenalectomy could be confirmed based on the current study.
Several risk factors have been associated with potential failure in blood pressure improvement following adrenalectomy, including having one or more first-degree relatives with hypertension, advanced age, duration of disease, and lack of response to spironolactone.21; 22 ; 23 Additional factors associated with persistence of hypertension were multiple adenomas or nodular hyperplasia.24 In our series, we had one case of unilateral hyperplasia who suffered aggravated hypertension after adrenalectomy. The effectiveness of adrenalectomy on PA patients due to unilateral hyperplasia is still controversial.23 ; 24 Walz et al24 found very late occurrences (5–14 years) of contralateral hyperplasia lesions after unilateral adrenalectomy for unilateral hyperplasia. A further cause of persistent or recurrent hypertension may be the presence of preoperatively undetected bilateral hyperplasia which could not be detected using the current technology.22 Thus, for PA patients with functional lateralized unilateral hyperplasia lesions, long-term or life-time follow up is mandatory.
There are only two meta-analyses that compared LESS and conventional laparoscopic adrenalectomy to date.14 ; 15 These studies revealed compatible incidence of procedure-related adverse events (complication, conversion, and transfusion rate) between the two techniques. The present cohort, which focused on PA patients undergoing LESS adrenalectomy, also revealed a compatible short postoperative convalescence, minimal perioperative complication, and low conversion rate (1 in 49 patients) when compared with other LESS or conventional laparoscopic series. As we demonstrated in Figure 1, LESS adrenalectomy was associated with a short learning period in experienced hands. What is interesting is that the transition from one minimally invasive technique to the other also demonstrated a short learning period with the patients' convalescences rapidly and significantly shortening after the learning period. In our logarithmic regression model generated cumulative curve regarding patients convalescence, the regression curves revealed a progressive reduction of time to convalescence during all the progressive cases. (Figure 2 ; Figure 3) Although LESS is commonly associated with a long, steep learning curve, in experienced hands, LESS adrenalectomy for PA is actually associated with a short learning curve and also a short transition period of longer patient convalescence.
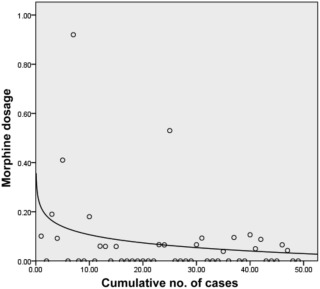
LESS adrenalectomy is a recent novel approach; the operative technique in LESS actually following the standard protocol in conventional laparoscopic adrenalectomy. A longer operative time was observed during the learning period due to adaptation to a new approach. However, the improvement in clinical outcome regarding hypertension was not observed according to our data. In addition, during LESS or conventional laparoscopic surgery, the lever pivot point of the instrument is located at the trocar incision of abdominal wall. The differences between LESS and laparoscopy is, in our single-port design, the surgical incision was only covered by a thin-layer soft transparent wound protector and not a rigid plastic tube that we commonly use in laparoscopy. Therefore, the blunt trauma associated with the forces applied by instruments shaft was clearly increased when the operative time was prolonged during the learning curve. This phenomenon could be explained by the increased postoperative analgesic usage during the learning curve (Figure 4) Furthermore, analgesics (such as morphine, demeral) usage after operation is one of the main causes of delayed bowel movement and also the main reason for delayed oral intake during the learning period.
|
|
|
Figure 4. Scatter plot and learning curve of morphine dosage. |
What really amazed us is the two cases in our cohort who suffered from persistent (longer than 6 months) erectile dysfunction after their adrenalectomies, a phenomenon never before reported in humans. Penile erection has been mainly believed to be an androgen-associated process in both rats and humans. Although blockage of nontesticular origin androgen with antiandrogen has been shown to have a negative impact on erection in castrated rats, the androgen of adrenal origin plays a minor role in maintaining erectile function in noncastrated mammals.25 In addition, as penile erection is a nitric oxide dependent process in intracellular mechanism, another possible explanation for erectile dysfunction after adrenalectomy is that the adrenalectomy might have a negative impact on nitric oxide synthase (NOS) activity thus impairing the erectile function. To date, only one study showed the adrenal gland contributes to the maintenance of the erectile mechanism and may affect neuronal NOS content in the penis in the rat model.26 However, the evidence still remains scarce in humans and the possibility that postadrenalectomy induced hypotension also plays a role in erection could not be totally ruled out. In short, erectile dysfunction is a possible morbidity of adrenalectomy in PA patients, which deserves further investigation in a large scale-study to confirm our speculations.
In conclusion, this is the first and largest series of PA patients treated with LESS adrenalectomy. Our experience revealed that LESS adrenalectomy is a safe and effective approach which is associated with comparable long-term cure and improvement of hypertension compared with conventional laparoscopic series in treating PA. In addition, LESS adrenalectomy for PA is not only associated with a short learning curve, but also a short transition period of patient convalescence impairment in experienced hands. Therefore, LESS adrenalectomy for PA is a suitable alternative for surgeons experienced in conventional laparoscopic adrenalectomy.
References
- 1 J.W. Funder, R.M. Carey, C. Fardella, et al.; Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline; J Clin Endocrinol Metab, 93 (2008), pp. 3266–3281
- 2 T. Nishikawa, M. Omura; Clinical characteristics of primary aldosteronism: its prevalence and comparative studies on various causes of primary aldosteronism in Yokohama Rosai Hospital; Biomed Pharmacother, 54 (2000), pp. 83s–85s
- 3 M. Omura, J. Saito, K. Yamaguchi, Y. Kakuta, T. Nishikawa; Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan; Hypertens Res, 27 (2004), pp. 193–202
- 4 M. Zacharias, A. Haese, A. Jurczok, J.U. Stolzenburg, P. Fornara; Transperitoneal laparoscopic adrenalectomy: outline of the preoperative management, surgical approach, and outcome; Eur Urol, 49 (2006), pp. 448–459
- 5 A. Assalia, M. Gagner; Laparoscopic adrenalectomy; Br J Surg, 91 (2004), pp. 1259–1274
- 6 C.H. Ho, P.W. Liao, V.C. Lin, et al.; Laparoendoscopic single-site (LESS) retroperitoneal partial adrenalectomy using a custom-made single-access platform and standard laparoscopic instruments: technical considerations and surgical outcomes; Asian J Surg, 38 (2015), pp. 6–12
- 7 S.D. Chung, C.Y. Huang, S.M. Wang, et al.; Laparoendoscopic single-site totally extraperitoneal adult inguinal hernia repair: initial 100 patients; Surg Endosc, 25 (2011), pp. 3579–3583
- 8 T.C. Li, S.D. Chung, P.A. Tai, et al.; Laparoendoscopic single-site retroperitoneal lumbar sympathectomy: initial report; Neurosurgery, 68 (2011), pp. 291–293
- 9 H.C. Tai, C.H. Ho, Y.C. Tsai; Laparoendoscopic single-site surgery: adult hernia mesh repair with homemade single port; Surg Laparosc Endosc Percutan Tech, 21 (2011), pp. 42–45
- 10 S.D. Chung, C.Y. Huang, S.M. Wang, et al.; Laparoendoscopic single-site (LESS) nephroureterectomy and en bloc resection of bladder cuff with a novel extravesical endoloop technique; Surg Innov, 17 (2010), pp. 361–365
- 11 S.D. Chung, C.Y. Huang, S.M. Wang, H.C. Tai, Y.C. Tsai, S.C. Chueh; Laparoendoscopic single-site (LESS) retroperitoneal adrenalectomy using a homemade single-access platform and standard laparoscopic instruments; Surg Endosc, 25 (2011), pp. 1251–1256
- 12 Y.C. Tsai, C.H. Ho, H.C. Tai; Laparoendoscopic single-site (LESS) retroperitoneal nephropexy with standard laparoscopic instruments; J Laparoendosc Adv Surg Tech A, 20 (2010), pp. 257–260
- 13 H.C. Tai, C.D. Lin, C.C. Wu, Y.C. Tsai, S.S. Yang; Homemade transumbilical port: an alternative access for laparoendoscopic single-site surgery (LESS); Surg Endosc, 24 (2010), pp. 705–708
- 14 L. Wang, Z. Wu, M. Li, et al.; Laparoendoscopic single-site adrenalectomy versus conventional laparoscopic surgery: a systematic review and meta-analysis of observational studies; J Endourol, 27 (2013), pp. 743–750
- 15 Q. Hu, Y. Gou, C. Sun, K. Xu, G. Xia, Q. Ding; A systematic review and meta-analysis of current evidence comparing laparoendoscopic single-site adrenalectomy and conventional laparoscopic adrenalectomy; J Endourol, 27 (2013), pp. 676–683
- 16 Y. Hirasawa, A. Miyajima, S. Hattori, et al.; Laparoendoscopic single-site adrenalectomy versus conventional laparoscopic adrenalectomy: a comparison of surgical outcomes and an analysis of a single surgeons learning curve; Surg Endosc, 28 (2014), pp. 2911–2919
- 17 V.C. Lin, Y.C. Tsai, S.D. Chung, et al.; A comparative study of multiport versus laparoendoscopic single-site adrenalectomy for benign adrenal tumors; Surg Endosc, 26 (2012), pp. 1135–1139
- 18 T.P. Shi, X. Zhang, X. Ma, et al.; Laparoendoscopic single-site retroperitoneoscopic adrenalectomy: a matched-pair comparison with the gold standard; Surg Endosc, 25 (2011), pp. 2117–2124
- 19 A. Rane, L. Cindolo, L. Schips, M. De Sio, R. Autorino; Laparoendoscopic single site (LESS) adrenalectomy: technique and outcomes; World J Urol, 30 (2012), pp. 597–604
- 20 M.K. Walz, H. Groeben, P.F. Alesina; Single-access retroperitoneoscopic adrenalectomy (SARA) versus conventional retroperitoneoscopic adrenalectomy (CORA): a case-control study; World J Surg, 34 (2010), pp. 1386–1390
- 21 F. Lumachi, M. Ermani, S.M. Basso, D. Armanini, M. Iacobone, G. Favia; Long-term results of adrenalectomy in patients with aldosterone-producing adenomas: multivariate analysis of factors affecting unresolved hypertension and review of the literature; Am Surg, 71 (2005), pp. 864–869
- 22 I. Gockel, A. Heintz, M. Polta, T. Junginger; Long-term results of endoscopic adrenalectomy for Conns syndrome; Am Surg, 73 (2007), pp. 174–180
- 23 M. Sywak, J.L. Pasieka; Long-term follow-up and cost benefit of adrenalectomy in patients with primary hyperaldosteronism; Br J Surg, 89 (2002), pp. 1587–1593
- 24 M.K. Walz, R. Gwosdz, S.L. Levin, et al.; Retroperitoneoscopic adrenalectomy in Conns syndrome caused by adrenal adenomas or nodular hyperplasia; World J Surg, 32 (2008), pp. 847–853
- 25 D.F. Penson, C. Ng, L. Cai, J. Rajfer, N.F. Gonzalez-Cadavid; Androgen and pituitary control of penile nitric oxide synthase and erectile function in the rat; Biol Reprod, 55 (1996), pp. 567–574
- 26 D.F. Penson, C. Ng, J. Rajfer, N.F. Gonzalez-Cadavid; Adrenal control of erectile function and nitric oxide synthase in the rat penis; Endocrinology, 138 (1997), pp. 3925–3932
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?