Summary
Intussusception is rare in adults, representing only 1% of bowel obstruction and 5% of all intussusceptions. Previous reports have shown that > 90% of adults diagnosed with intussusception had an identifiable pathological leading point—a malignant tumor in 43–63% of the cases. Colonic lipomas are rare nonepithelial neoplasms, but represent the most common benign tumors in the large intestine. Most colonic lipomas present as submucosal, sessile polypoid masses with intact mucosa, and they rarely produce symptoms when < 2 cm in diameter. However, all the intussuscepted lipomas in the literature had a tumor size > 4 cm in diameter. As the clinical presentations of adult intussusception are not pathognomonic and the image study may not provide a typical presentation, a precise preoperative diagnosis of whether a benign or malignant tumor is causing the colon intussusception can be difficult. Here, we report the case of a 50-year-old man who presented with abdominal pain and lower gastrointestinal bleeding and was diagnosed postoperatively with ileocecal valve lipoma with cecal-transverse colon intussusception. This report emphasizes colonic lipomas > 4 cm in diameter should receive surgical resection before intussusception develops. However, if the nature of the tumor causing colon intussusception cannot be identified before the operation, en bloc resection is recommended as there is a high risk of malignancy spreading.
Keywords
Adult ; Benign tumor ; Bloody stool ; Colon intussusception ; Colonic lipoma
Introduction
Although intussusception is a relatively common etiology of bowel obstruction in children, it remains rare in adults: only 1% of bowel obstructions and 5% of all intussusceptions [1] . It usually occurs in predominantly male, middle-aged patients [2] . Previous reports have shown that > 90% of adult intussusceptions had an identifiable pathological leading point [2] ; [3] ; [4] ; [5] . Although the prevalence of colon intussusception is much lower than enteric intussusception (22% vs. 78%, respectively), the incidence of colon intussusception caused by malignancy is greater than enteric intussusception [5] . Colonic lipomas are rare nonepitheliral neoplasms in the large intestine and account for 0.035–4.4% of all polypoid lesions in the colon [6] . Most colonic lipomas are asymptomatic. Our case report presents abdominal pain and gastrointestinal bleeding.
Case Report
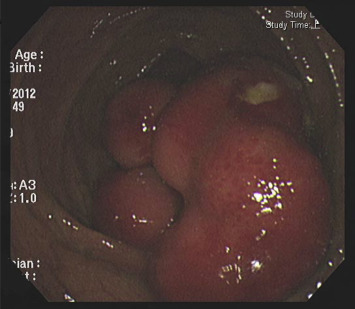
A 50-year-old man without a personal or family history of colorectal cancer presented with a 5-month history of loose yellow-colored stool passage and intermittent periumbilical pain. Recently, the stool consistency had become mucus-tinged and bloody, occurring approximately twice a day, and accompanied by upper abdominal pain. When he visited our clinic, we performed a colonoscopy and found a large, sessile, hard polypoid mass with congestive overlying mucosa and focal ulcerations involving the ileocecal valve and ascending colon (Figure 1 ). The colonoscope could not be inserted into the terminal ileum because the orifice of the ileocecal valve was almost completely obstructed by the tumor.
|
|
|
Figure 1. A large, sessile, hard polypoid tumor with a congestive overlying mucosa and focal ulcerations involving the ileocecal valve and ascending colon. |
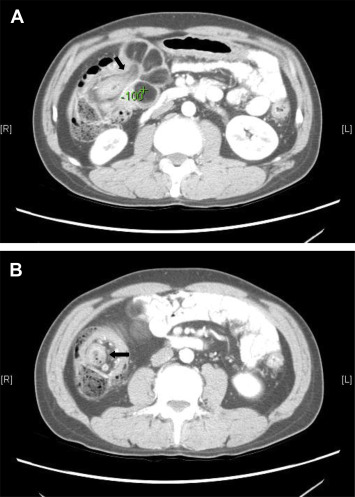
Endoscopic biopsy of the tumor showed normal colonic mucosa with focal necrosis and inflammation, but no evidence of malignancy. As a large amount of bloody stool passage developed after the colonoscope exam, we ordered a contrast-enhanced abdominal computed tomography (CT), which showed intussusception of the transverse colon by a giant polypoid tumor (Figures 2 A and 2B). Although the densiometry value of the tumor (−100 Hounsfield units, HU) was indicative of lipoma, liposarcoma could not be rule out because of its atypical presentation on the computed tomographic images (i.e., prominent septa and nodularity).
|
|
|
Figure 2. Contrast-enhanced abdominal computed tomography showing (A) intussusception of the transverse colon by a giant polypoid tumor; (B) with a bowel-within-bowel appearance (black arrow). |
Surgical intervention was suggested for tumor intussusception, but the patient refused at that time. However, a few days later, he was admitted to our hospital because of severe upper abdominal pain with bloody stool progression. Physical examination showed a systolic and diastolic pressure of 120/76 mmHg, a heart rate of 106 beats/min, and a palpable mass with tenderness over the epigastric area. Laboratory studies disclosed the following values: hemoglobin level, 15.6 g/dL (normal range, 13.5–17.5 g/dL); white blood cell count, 6.7 × 103 /uL (normal range, 3.9–10.6 × 103 /μL); platelet count, 305 × 103 /uL (normal range, 150–400 × 103 /μL); international normalized ratio (INR), 1.0 (normal range, < 1.2); albumin level, 3.9 g/dL (normal range, 3.5–5.5 g/dL); and carcinoembryonic antigen (CEA), 0.67 ng/mL (normal range, < 0.5 ng/mL).
During the operation, we found an 8.5 cm × 5.0 cm × 4.0 cm polypoid tumor involving the ileocecal valve and resulting in cecal-transverse colon intussusception; we then performed a right hemicolectomy. Histopathological examination of the resected tumor showed mature adipose tissue, with delicate septa in the submucosa compatible with submucosal lipoma. The postoperative course of the patient was uneventful, and he was still well 1 year after the operation.
Discussion
Lipomas are the most common benign mesenchymal tumors of the gastrointestinal tract, appearing most frequently in the colon. However, colonic lipomas are still rare, with a reported incidence of 0.3–0.5% in autopsy cases [7] , and usually involve the ascending colon, transverse colon, and cecum. Colonic lipomas typically arise from the submucosa and present as a sessile polypoid mass with intact mucosa, but they may also form a pedunculated tumor with an ulcerative surface.
Most colonic lipomas are asymptomatic, with only 25% causing symptoms, especially when their size exceeds 2 cm in diameter. Size has an important impact on the development of symptoms, because 75% of lipomas > 4 cm in diameter are symptomatic [8] . The most common symptom of a colonic lipoma before the occurrence of intussusception is abdominal pain. Other clinical presentations may be related to intestinal obstruction, such as nausea, vomiting, constipation, and diarrhea. Lower gastrointestinal bleeding is also common and presents in 22% of patients. However, a preoperative diagnosis is difficult to establish because these clinical presentations are often not pathognomonic of colonic lipomas.
Colonoscopic findings may provide direct inspection of submucosal lipoma with endoscopic features, including the “tenting sign”, “cushion sign”, and “naked fat sign”. In our patient, however, the large size of the polypoid lipoma precluded evaluation of the “tenting sign” and “cushion sign”.
Abdominal ultrasonographic findings indicative of intussusception include the “crescent-in-doughnut sign” and “pseudokidney sign” [9] . An abdominal CT is another noninvasive diagnostic tool. Findings characteristic of lipoma on abdominal CT include the presence of smooth, demarcated margins with thin fibrous septa, and homogenous fatty densiometry values ranging from −40 HU and −120 HU [10] . Duration between the diagnosis of lipoma and intussusception has been reported to range from 1 day to 7 years [8] . Our patient developed intussusception 10 days after the colonoscopy.
Endoscopic resection is suggested for pedunculated lipomas or lipomas measuring < 2 cm in diameter. However, if a lipoma is sessile or has a diameter greater than 2 cm, surgery is preferred because the risk of perforation is high during endoscopic resection [10] .
Primary colon adenocarcinoma is the main cause of malignant colon intussusception, followed by lymphoma and metastasis [2] ; [5] . Benign colonic lesions, including lipomas, benign stromal tumors, and adenomatous polyps, account for ∼30% of colon intussusceptions [11] . Lipoma is the most common benign cause of colon intussusception. In a review of 37 cases, by Paškauskas et al [8] found that the greatest diameter of lipomas causing intussusception ranged from 4 cm to 16.0 cm and that none of the patients with intussusception due to colonic lipoma had a lipoma measuring < 4 cm in size. Abdominal pain is the most common clinical symptom in patients with intussusception. The other clinical presentations include nausea, vomiting, hematochezia, body weight loss, and a palpable abdominal mass. Compared with enteric intussusception, the clinical presentation of colonic intussusception generally has a more subacute onset with prolonged abdominal pain or constipation. Unless acute presentation occurs, emergency surgery is not necessary.
Preoperative diagnosis of colonic intussusception is difficult to establish because the clinical presentations are not typically pathognomonic. Previous studies have shown that CT is the most useful and accurate diagnostic tool for intussusception, with 85% of the cases being correctly diagnosed [3] . In our patient, the CT appearance of bowel-within-bowel, which is described as “sausage sign” on longitudinal section and “target sign” on transverse section, is a typical presentation of intussusception. A polypoid tumor as the leading point was also identified. The densiometry value indicated lipoma. However, due to the atypical CT presentation with prominent septa and nodularity, we could not exclude the possibility of liposarcoma. A surgical approach with en bloc resection without reduction is recommended for colonic intussusception because of the high malignancy rate of the leading point and the possibility that the reduction procedure may cause the malignant tumor to spread.
In conclusion, most of the colonic lipomas of > 4 cm in greatest diameter are symptomatic and should receive surgical resection before intussusception develops. However, if the nature of the tumor causing colon intussusception cannot be identified before the operation, en bloc resection is recommended as there is a high risk of malignancy in colon intussusception.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- [1] Y.H. Kim, M.A. Blake, M.G. Harisinghani, K. Archer-Arroyo, P.F. Hahn, M.B. Pitman, et al.; Adult intestinal intussusception: CT appearances and identification of a causative lead point; Radiographics, 26 (2006), pp. 733–744
- [2] T. Azar, D.L. Berger; Adult intussusception; Ann Surg, 226 (1997), pp. 134–138
- [3] W.S. Huang, C.S. Changchien, S.N. Lu; Adult intussusception: a 12-year experience, with emphasis on etiology and analysis of risk factors; Chang Gung Med J, 23 (2000), pp. 284–290
- [4] E.M. Haas, E.L. Etter, S. Ellis, T.V. Taylor; Adult intussusception; Am J Surg, 186 (2003), pp. 75–76
- [5] J.M. Chiang, Y.S. Lin; Tumor spectrum of adult intussusception; J Surg Oncol, 98 (2008), pp. 444–447
- [6] M.A. Murray, V. Kwan, S.J. Williams, M.J. Bourke; Detachable nylon loop assisted removal of large clinically significant colonic lipomas; Gastrointest Endosc, 61 (2005), pp. 756–759
- [7] B. Marra; Intestinal occlusion due to a colonic lipoma. Apropos 2 cases; Minerva Chir, 48 (1993), pp. 1035–1039
- [8] S. Paškauskas, T. Latkauskas, G. Valeikaite, A. Parseliunas, S. Svagzdys, Z. Saladzinskas, et al.; Colonic intussusception caused by colonic lipoma: a case report; Medicina (Kaunas), 46 (2010), pp. 477–481
- [9] C.S. Chung, M.Y. Wang, H.P. Wang; A “crescent-in-doughnut” lesion at right lower quadrant abdomen; Gastroenterology, 137 (2009), pp. e3–e4
- [10] S. Atmatzidis, G. Chatzimavroudis, A. Patsas, B. Papaziogas, S. Kapoulas, S. Kalaitzis, et al.; Pedunculated cecal lipoma causing colo-colonic intussusception: a rare case report; Case Rep Surg, 2012 (2012), p. 279213
- [11] M.J. Gollub; Colonic intussusception: clinical and radiographic features; AJR Am J Roentgenol, 196 (2011), pp. W580–W585
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?