Summary
Objective
To examine the expression of Mullerian inhibiting substance (MIS) in papillary thyroid cancer.
Materials and methods
The MIS expression was examined by studying the immunohistochemistry in deparafinized sections prepared from tissue blocks of patients who were diagnosed with papillary thyroid cancer, as given in the pathology archive records (n = 23).
Results
In all the cases studied, 50% (n = 10) showed strong staining and 50% showed moderate staining. The percentage of staining was found to be 94.2 ± 3.1% in strongly stained cases and 92.2 ± 2.1% in moderately stained cases. Normal thyroid tissues neighboring the tumor did not display any staining.
Conclusion
The MIS expression can be used as a significant tool in differential diagnosis of papillary thyroid cancer and also to shed light on its etiopathogenesis.
Keywords
immunohistochemistry;Mullerian inhibiting substance;papillary thyroid cancer
1. Introduction
The Mullerian inhibiting substance (MIS) is a member of the transforming growth factor-beta (TGF-β) protein family, and it is responsible for the regression of the Mullerian channel in the development of the male embryo.1 The regulation of the MIS gene expression demonstrates sexual dimorphism. This hormone, which is considerably high in neonatal and prepubertal periods in males and immeasurably low in females, reaches equal levels after puberty in both sexes and drops down to immeasurable levels once again after menopause in females.2
For many years, the MIS has been thought to have a limited function in the determination of sex in the intrauterine period, and only recently, it was found that the MIS plays significant roles in the testicular maturation in males and the regulation of follicular growth in females and that both MIS and its receptors were present in many types of cancer, most notably ovarian cancer.3 ; 4
The recombinant MIS was shown to cause a strong blockage of the epidermal growth factor receptor (EGFR) in complex interactions at the molecular level.5 In a recent study, it was demonstrated that the EGFR, in turn, contributed substantially to rearranged during transfection (RET) kinase activation, a hallmark in papillary thyroid cancer, as well as many others.6 Despite the established relationship between EGFR and thyroid cancer, it is not known how the levels of MIS, whose role is currently under research, are affected in thyroid cancer.
In this preliminary study, we examine how the MIS levels are affected in papillary thyroid cancer.
2. Materials and methods
The tissues used in this study were procured from the archives of the Pathology Department of Fırat University. Twenty samples from the cases diagnosed as papillary thyroid cancer in the archive records were randomly chosen, and their preparations stained with hematoxylin and eosin were re-examined to reconfirm the diagnosis. Additionally, sociodemographic characteristics of the cases were retrieved from the records in their files.
2.1. Tissue preparation and immunohistochemistry
The method developed by Meyts and colleagues was employed to determine MIS expression in papillary thyroid cancer using the immunohistochemical method.7 In short, cross-sections of 4 μm were taken from fixed tissues buried in paraffin with minor modifications and placed on poly-l-lysine coated slides using avidin-biotin-peroxidase complex (ABC) technique (Lab Vision Corporation, USA). All cross-sections were deparaffinized using routine techniques. Following deparaffinization, the sections were dehydrated by passing through three different absolute alcohols and three different 96% alcohol solutions within 20 minutes. Subsequently, the tissue sections were treated in the microwave oven at 1000 W and 400 W for 5 minutes with 5% urea buffer. The cross-sections were kept at room temperature for 15 minutes and then incubated in methanol with 2% H2O2 to eliminate endogenous peroxidase activity. All the sections were coated with diluted goat serum to avoid the binding of nonspecific antibodies. The incubation with a primary antibody was carried out overnight at 4°C.
The antibody was a monoclonal mouse antihuman AMH (Mab 10.6) from AbD Serotec, cat # MAC2246. The incubation with the second “link” antibody (biotinylated goat antimouse IgG, Zymed Laboratories, Inc., San Francisco, CA) and the color development (streptavidin–peroxidase complex, followed by acethylcarbazol and hydrogen peroxide (H2O2)) were performed at room temperature according to manufacturers instructions. The placental tissue was used as the negative control. Staining in the range between orange and light brown was accepted as a positive reaction.
The preparations obtained as such were examined under a light microscope by two experienced pathologists and scored according to the severity of staining. Accordingly: 0 = no staining, 1 = mild staining, 2 = moderate staining, and 3 = strong staining. Furthermore, the staining areas of all preparations were determined in percentages.
2.2. Statistical analysis
The statistical evaluation was based on the severity and percentage of staining. The data were expressed as mean ± standard deviation. One-way Analysis of Variance (ANOVA) was used to compare groups, and Tukeys tests were used for post-hoc analysis. Values of p < 0.05 were considered statistically significant.
3. Results
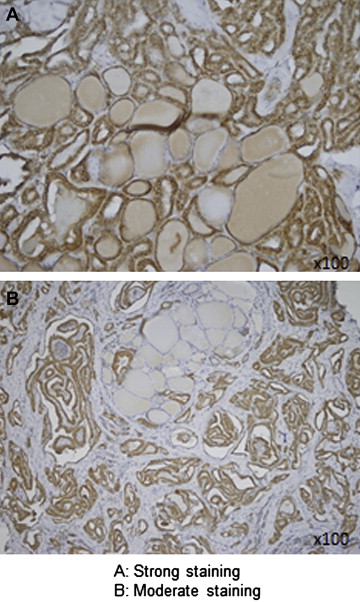
In this study, 35% of the cases were male and 65% were female. The mean age was 53 ± 2 years for males and 45 ± 3 years for females. Of all the cases, 50% (n = 10) showed strong staining and 50% (n = 10) showed moderate staining ( Fig. 1). The mean staining surface was found to be 94.2 ± 3.1% in strongly stained cases and 92.2 ± 2.1% in moderately stained cases. No significant difference was established between the staining percentages (p > 0.05). There was no staining in normal thyroid tissues neighboring the tumor. One metastatic lymph node preparation showed mild staining, while the other showed no staining. Placental tissues that were used as controls did not display staining either. There was no significant difference between males and females in terms of staining severity and percentage. The staining levels and percentages of the preparations are presented in Table 1.
|
|
|
Figure 1. Severity scores of Mullerian inhibiting substance staining under a light microscope in papillary thyroid carcinomas. |
| Biopsy no. | Severity of staining (0: no staining, 1: mild staining, 2: moderate staining, 3: strong staining) | Percentage of staining |
|---|---|---|
| 1 | 3 | 80% |
| 2 | 2 | 90% |
| 3 | 2 | 100% |
| 4 | 2 | 90% |
| 5 | 2 | 80% |
| 6 | 3 | 80% |
| 7 | 3 | 100% |
| 8 | 3 | 90% |
| 9 | 2 | 80% |
| 10 | 3 | 90% |
| 11 | 3 | 100% |
| 12 | 2 | 100% |
| 13 | 3 | 90% |
| 14 | 3 | 80% |
| 15 | 3 | 90% |
| 16 | 2 | 80% |
| 17 | 2 | 70% |
| 18 | 2 | 80% |
| 19 | 3 | 100% |
| 20 | 2 | 80% |
| 21 – Lymph node metastasis | 1 | 30% |
| 22 – Lymph node metastasis | 0 | 0% |
| 23 – Placenta | 0 | 0% |
MIS = Mullerian inhibiting substance.
4. Discussion
In our study, the MIS expression in papillary thyroid cancer was found to be at a high rate and strong most of the time. To the best of our knowledge, no study on the presence of MIS in either normal thyroid tissue or thyroid cancers has been mentioned in the literature. The MIS expression in papillary thyroid cancer has been shown for the first time in this study.
Our literature review has revealed that just as MIS inhibits Mullerian structures in the embryonic period, it continues to exert this inhibiting effect in the postnatal period. This effect was shown in cervical and endometrial cancers, and most notably in the ovarian cancer, through different mechanisms.8; 9; 10 ; 11
The MIS binds to Type I and II receptors in the cell membrane. The bioactive MIS forms a heteromeric complex with transmembrane serine/threonine kinases. The extracellular cysteine-rich domain of the Type II receptor ligand ensures specificity. FKBP-12-bound Type I receptors strengthen Type II and maintain signal transmission.2 The purified recombinant human MIS was shown to inhibit growth in ovarian cells via a receptor-mediated mechanism both in vivo and in vitro. Similarly, the MIS was demonstrated to inhibit growth in endometrial, cervical, and breast cancers, where the MIS receptors are found through receptor-mediated mechanisms. 8; 9; 10; 11; 12; 13; 14; 15; 16 ; 17 On the basis of these data, it can be speculated that MIS is expressed in response to the proliferative effect of the EGFR, which is known to have a strong proliferative effect in thyroid cancer. However, thus far, there is no clarity regarding those growth factors inhibited by MIS in papillary thyroid cancers.
Although the oncogenic potential of rearranged in transformation/papillary thyroid carcinomas (RET/PTC), the most commonly established genetic modification in papillary thyroid cancer, is in a close relationship with intrinsic tyrosine kinase activity, the substrates of this enzyme are not clear. Kim et al. reported in their study that serine/threonine kinases were also used as targets of RET/PTC in growth-factor signaling pathways and that the concerned pathway might be among the mechanisms in thyroid carcinogenesis.18 An overall evaluation of this information suggests that the elevated expression of MIS in papillary thyroid cancer may be through the serine/threonine kinases pathway.
However, when the fact that a high number of studies are needed to clarify the mechanism of MIS expression is set aside, our finding in the immunohistochemical differentiation of papillary thyroid cancer is a new marker. There was little or no immunohistochemical staining outside the normal thyroid cancer sites in our study, which suggests that it can be used as a new marker in differential diagnosis.
We have presented an excellent finding for the diagnosis of papillary cancer. We demonstrated MIS expression in papillary cancer tissues only by employing the immunohistochemical method that was developed by Meyts and colleagues.7 We did not use Western blotting or enzyme-linked immunosorbent assay (ELISA), but we believe that further prospective studies need to be conducted on MIS. We had conducted our retrospective study only on the pathological blocks of tissues from patients diagnosed with papillary cancer. We had also observed that there was no MIS expression in the sections of normal thyroid tissue. Therefore, we did not include a control group in our study.
In conclusion, due to the fact that MIS has been started to be studied only recently, there is insufficient information on the interaction of this hormone with other systems, the tissues in which it has receptors, and its relation with cancers, except for a limited number of gynecologic cancers. Further studies on MIS are needed to interpret the findings obtained in our study.
References
- 1 J. Teixeira, S. Maheswaran, P.K. Donahoe; Mullerian inhibiting substance: an instructive developmental hormone with diagnostic and possible therapeutic applications; Endocr Rev, 22 (2001), pp. 657–674
- 2 J. Teixeira, P.K. Donahoe; Molecular biology of MIS and its receptors; J Androl, 17 (1996), pp. 336–341
- 3 A.L. Durlinger, M.J. Gruijters, P. Kramer, et al.; Anti-Müllerian hormone attenuates the effects of FSH on follicle development in the mouse ovary; Endocrinology, 142 (2001), pp. 4891–4899
- 4 Y. Ikeda, A. Nagai, M.A. Ikeda, et al.; Increased expression of Müllerian-inhibiting substance correlates with inhibition of follicular growth in the developing ovary of rats treated with E2 benzoate; Endocrinology, 143 (2002), pp. 304–312
- 5 M.A. Maggard, E.A. Catlin, P.L. Hudson, et al.; Reduction of epidermal growth factor receptor phosphorylation by activated Mullerian inhibiting substance is vanadate-sensitive; Metabolism, 45 (1996), pp. 190–195
- 6 M. Croyle, N. Akeno, J.A. Knauf, et al.; RET/PTC-induced cell growth is mediated in part by epidermal growth factor receptor (EGFR) activation: evidence for molecular and functional interactions between RET and EGFR; Cancer Res, 68 (2008), pp. 4183–4191
- 7 E. Rajpert-De Meyts, N. Jørgensen, N. Graem, et al.; Expression of anti-Müllerian hormone during normal and pathological gonadal development: association with differentiation of Sertoli and granulosa cells; J Clin Endocrinol Metab, 84 (1999), pp. 3836–3844
- 8 A.E. Stephen, L.A. Pearsall, B.P. Christian, et al.; Highly purified Müllerian inhibiting substance inhibits human ovarian cancer in vivo; Clin Cancer Res, 8 (2002), pp. 2640–2646
- 9 P.T. Masiakos, D.T. MacLaughlin, S. Maheswaran, et al.; Human ovarian cancer, cell lines, and primary ascites cells express the human Mullerian inhibiting substance (MIS) type II receptor, bind, and are responsive to MIS; Clin Cancer Res, 5 (1999), pp. 3488–3499
- 10 T.U. Ha, D.L. Segev, D. Barbie, et al.; Mullerian inhibiting substance inhibits ovarian cell growth through an Rb-independent mechanism; J Biol Chem, 275 (2000), pp. 37101–37109
- 11 T.U. Barbie, D.A. Barbie, D.T. MacLaughlin, et al.; Mullerian inhibiting substance inhibits cervical cancer cell growth via a pathway involving p130 and p107; Proc Natl Acad Sci USA, 100 (2003), pp. 15601–15606
- 12 J.W. Wallen, R.L. Cate, D.M. Kiefer, et al.; Minimal antiproliferative effect of recombinant Müllerian inhibiting substance on gynecological tumor cell lines and tumor explants; Cancer Res, 49 (1989), pp. 2005–2011
- 13 D.T. MacLaughlin, P.L. Hudson, A.L. Graciano, et al.; Mullerian duct regression and antiproliferative bioactivities of mullerian inhibiting substance reside in its carboxy-terminal domain; Endocrinology, 131 (1992), pp. 291–296
- 14 T. Chin, R.L. Parry, P.K. Donahoe; Human Mullerian inhibiting substance inhibits tumor growth in vitro and in vivo; Cancer Res, 51 (1991), pp. 2101–2106
- 15 D.L. Segev, T.U. Ha, T.T. Tran, et al.; Mullerian inhibiting substance inhibits breast cancer cell growth through an NFkappa B-mediated pathway; J Biol Chem, 275 (2000), pp. 28371–28379
- 16 E.J. Renaud, D.T. MacLaughlin, E. Oliva, et al.; Endometrial cancer is a receptor-mediated target for Mullerian inhibiting substance; Proc Natl Acad Sci USA, 102 (2005), pp. 111–116
- 17 L. Gouedard, Y.G. Chen, L. Thevenet, et al.; Engagement of bone morphogenetic protein type IB receptor and Smad1 signaling by anti-Mullerian hormone and its type II receptor; J Biol Chem, 275 (2000), pp. 27973–27978
- 18 D.W. Kim, J.H. Hwang, J.M. Suh, et al.; RET/PTC (rearranged in transformation/papillary thyroid carcinomas) tyrosine kinase phosphorylates and activates phosphoinositide-dependent kinase 1 (PDK1): an alternative phosphatidylinositol 3-kinase-independent pathway to activate PDK1; Mol Endocrinol, 17 (2003), pp. 1382–1394
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?