Highlights
- Rasch analysis of the Portuguese version of the Substance Problem Scale performed
- This scale has performance similar to Canadian and American versions.
- None of the scale items distort the measurement.
- Further differential item functioning analysis with larger sample needed
Abstract
Introduction
This study used the Rasch model to evaluate the psychometric properties of the Portuguese version of the Substance Problem Scale (SPS) of the “Global Appraisal of Individual Needs - Initial” for use in Brazil. The SPS measures alcohol and drug problem severity within a DSM-IV-TR framework. The goal of the Rasch analysis was to assess scale dimensionality, item severity, and differential item functioning (DIF).
Methods
Data was collected from 40 inpatients and 70 outpatients in São Paulo, Brazil. The Rasch model fit and DIF by gender and level of care were examined.
Results
The SPS fit the Rasch model, with no items distorting the measure. Only three of the sixteen items performed differently between men and women and three performed differently by level of care.
Conclusions
The results were compatible with those from Rasch analyses of the American English and Canadian English versions of the scale. The Portuguese version of the SPS is, thus, valid for use in Brazil, both with men and women in inpatient and outpatient programs.
Keywords
Validation studies;Alcohol-related disorders;Substance-related disorders
1. Introduction
Intervening during the early stages of a substance use disorder greatly improves the prognosis, thus making the development of early intervention assessment strategies a priority. Studies have documented the need for rapid, accurate evaluation of symptoms and comorbidities related to substance use. Assessment tools must be valid, reliable and cost-effective (Formigoni, M. and Castel, S., 1999 ; Henrique, I., et al., 2004).
Currently, in Brazil, assessment tools such as the Alcohol, Smoking and Substance Involvement Screening test — ASSIST (Henrique et al., 2004) and Alcohol Use Disorders Identification Test — AUDIT (Moretti-Pires & Corradi-Webster, 2011) are validated and being used both in clinical practice and research. However, there is still a need to develop a full-length, comprehensive psychosocial assessment that includes not just items on substance use, but also those on substance use-related needs of the client (e.g., legal, mental health, physical health, environment, vocational, risk behaviors and other areas of interest) (Claro, Oliveira, Almeida, Vargas, & Paglione, 2011).
The GAIN — Global Appraisal of Individual Needs, or, in Portuguese, AGNI — “Avaliação Global das Necessidades Individuais”, is a family of evidence-based assessment tools. These instruments include a screening instrument – the GAIN-SS Short Screener (AGNI-RR in Portuguese — Rastreio Rápido) – which takes 10 to 15 min to administer; the GAIN-Quick version 3 (GAIN-Q3), a targeted assessment that takes about 30–45 min to administer; and the GAIN-Initial (GAIN-I), a full biopsychosocial evaluation which takes 90 to 120 min to administer (Dennis, White, Titus, & Unsicker, 2003).
Linguistic and cultural adaptation of the GAIN-I included two independent forward translations, a synthesis of the forward translations analyzed by an expert committee, a back translation into English, and reconciliation of the back translated English version with the original English by the instrument developers (Claro et al., 2012). The final revised versions of the Portuguese AGNI-I and AGNI-RR (composed of a subset of items from the AGNI-I) were then validated with inpatients and outpatients in the city of São Paulo, Brazil (Claro, 2015).
Chestnut Health Systems (CHS), a not-for-profit private behavioral health organization with a state-of-the-science research institute, developed the GAIN instruments and related materials. The GAIN Assessment Building System (ABS) is the software system that houses all the GAIN instruments and allows for computer-assisted administration and the production of several kinds of clinical reports of the results. CHS has also developed GAIN trainings and offers data analysis services for agencies using GAIN instruments. The GAIN was developed with support from U.S. federal agencies such as the Substance Abuse and Mental Health Services Administration (SAMHSA), National Institute on Drug Abuse (NIDA), and the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The GAIN family of assessments has been used by more than 1700 agencies and projects in 49 U.S. states and in countries such as Canada (Kenaszchuk, Wild, Rush, & Urbanoski, 2013). Translations of the shortest GAIN instrument, the GAIN-SS, have been completed, allowing for use of the GAIN-SS in Japan, Russia, the Philippines, Vietnam, Indian states and Asian regions (Hmong dialect), among others (Dennis, 2010). Data from all GAIN instruments support research reports and scientific publications (Dennis, M., et al., 2008; Gotham, H., et al., 2008; Titus, J., et al., 2008 ; Titus, J. C., et al., 2012).
The GAIN instruments are designed to guide clinical decision making about diagnosis, treatment planning and placement, and monitoring of results. The GAIN can also be integrated into electronic health records and information systems. A great deal of research using pooled GAIN data from a collection of treatment and research programs across the U.S. and Canada has been done (Dennis, M., et al., 2006; Dennis, M., et al., 2004; Dennis, M., et al., 2003 ; Kenaszchuk, C., et al., 2013).
The Substance Problem Scale (SPS) as appears on the GAIN-I is a 16-item scale composed of lifetime symptoms of substance abuse, dependence, and substance-induced health and psychological disorders based on the DSM-IV. Higher scores on the SPS represent greater severity of alcohol and other drug problems. The scale includes physiological, psychological and social criteria. A total score of 0 symptoms endorsed suggests no reported drug problems, 1 or more suggests abuse, and 4 or more suggests dependence (Dennis, M., et al., 2004; Dennis, M., et al., 2003 ; Kenaszchuk, C., et al., 2013). The information collected supports diagnosis and treatment, and previous studies have shown its value for use in clinical practice (Kenaszchuk et al., 2013). Studies on the validity and reliability of the scale support its use with both adolescents and adults (Conrad, K. J., et al., 2011 ; Lennox, R., et al., 2006).
The Rasch model was originally developed for use in the education field for the assessment of student learning. When measuring a trait, the Rasch model considers the difficulty of an item and the subjects ability to respond to it. Rasch measurement is based on the probability that a person will answer each item correctly. In psychological measurement, there are no “correct” answers (in contrast to educational measurement). Rather than being based on “correctness”, the Rasch model in psychological measurement is based on responding positively to an item in accordance with an increased amount of the characteristic or trait being measured. In the SPS, which measures severity of problems related to the use of alcohol and other drugs, the “correct” answer for each item is a positive response (that is, the interviewee endorses the problem measured by an item). More severe clients should have more positive responses than a less severe one. Thus, the Rasch model analyzes if the scale is in fact able to detect greater severity in the most severe clients (Boone, W. J., et al., 2014 ; Chachamovich, E., 2007).
Rasch is a prescriptive method that permits checking whether the tested scale meets the necessary and sufficient conditions for the fundamental measurement model. The goal is to achieve a good fit of the data to the model. Scales that meet the Rasch model requirements are deemed to measure the trait of interest (the latent variable).
2. Methods
2.1. Sample and procedure
Prior to data collection, a description of the research project and instrument was presented to the 70 inpatients of the residential agency; 40 agreed to participate and were interviewed. The outpatient agency was one of the Centers for Psychosocial Attention for Alcohol and Drugs (CAPSad) in São Paulo. There, 304 individuals eligible for the study began treatment between March and December, 2014. However, only 117 returned to complete the instrument(s); of those, an additional 47 clients were excluded from the sample. Exclusions were due to cognitive impairment (16), time unavailability (6), the need for urgent health attention due to severe withdrawal symptoms, or clients overly emotive (crying, upset; 9) and were thus referred to their case managers for further evaluation and interventions, and clients who started the interview but did not come back to finish it (14). The final sample from CAPSad was composed of 70 complete interviews. The total sample for the study was composed of 110 individuals. The study was approved by the Ethics Committee of the School of Nursing at the University of São Paulo, the Municipal Health Secretary of São Paulo (CAE 15450713.8.0000.5392), and by the Internal Review Board of Chestnut Health Systems (IRB Study No. 1076–0912).
Among these 110 respondents, there was a predominance of males (70%); the mean age was 33.35 years and the mean age of first use was 15.82 years (with a range of 7 to 42 years). The most prevalent race/color/ethnicity was white (41.8%), 67.3% of the clients were never homeless, 38.2% were smokers at the time of data collection, and 91.8% were sexually active in the preceding year. Data showed that 73.6% reported never having been involved in criminal activity and 30.9% reported having suffered mentally or psychologically in the two days prior to the interview. For 44.5% of the sample, this was the first episode of treatment; 80.9% felt drunk or high during at least one day of the 90 days prior to data collection.
2.2. Treatment
The data from this study was collected in an inpatient unit for alcohol and other drug (AOD) users in the state capital and a Center for Psychosocial Care for AOD - CAPSad, also in São Paulo. In both places, the treatment included individual and group counseling. Each individual was assigned to a case manager, who works with the client to set treatment goals. In both settings, the treatment was free of charge since the treatment agencies belong to the psychosocial network of care within the Universal Health System of Brazil.
2.3. Measurements
Clients were interviewed with the Brazilian Portuguese version of the Global Appraisal of Individual Needs — GAIN Initial (GAIN-I), and the data were entered into the Global Appraisal of Individual Needs — GAIN — Assessment Building System (GAIN ABS), an online application for interactive on-site data collection (Dennis et al., 2003). A clinical report is generated from the data entered into ABS, and the report was made available to the treatment staff. The data analyzed here are from the SPS scale of the instrument. The 16 items on the SPS are composed of symptoms of a substance use disorder and are shown in Table 1 Each item was answered along a 4-point scale indicating the last time the client ever had this problem or symptom: 0 for “never”, 1 for “more than 12 months ago”, 2 for “2–12 months ago”, and 3 for “during the past month”.
| Number of the item | Item “When was the last time” |
|---|---|
| S9c | You tried to hide that you were using alcohol or other drugs? |
| S9d | Your parents, family, partner, co-workers, classmates or friends complained about your alcohol or other drug use? |
| S9e | You used alcohol or other drugs weekly or more often? |
| S9f | Your alcohol or other drug use caused you to feel depressed, nervous, suspicious, uninterested in things, reduced your sexual desire or caused other psychological problems |
| S9g | Your alcohol or other drug use caused you to have numbness, tingling, shakes, blackouts, hepatitis, TB, sexually transmitted disease, or any other health problems? |
| S9h | You kept using alcohol or other drugs even though you knew it was keeping you from meeting your responsibilities at work, school, or home? |
| S9j | You repeatedly used alcohol or other drugs when it made the situation unsafe or dangerous for you, such as when you were driving a car, using a machine, or when you might have been forced into sex or hurt? |
| S9k | Your alcohol or other drug use caused you to have repeated problems with the law? |
| S9m | You kept using alcohol or other drugs even though it was causing social problems, leading to fights, or getting you into trouble with other people? |
| S9n | You needed more alcohol or other drugs to get the same high or found that the same amount did not get you as high as it used to |
| S9p | You had withdrawal problems from alcohol or other drugs like shaky hands, throwing up, having trouble sitting still or sleeping, or you used any alcohol or other drugs to stop being sick or avoid withdrawal problems? |
| S9q | You used alcohol or other drugs in larger amounts, more often or for a longer time than you meant to? |
| S9r | You were unable to cut down on or stop using alcohol or other drugs? |
| S9s | You spent a lot of time either getting alcohol or other drugs, using alcohol or other drugs, or feeling the effects of alcohol or other drugs (high, sick)? |
| S9t | Your use of alcohol or other drugs caused you to give up, reduce or have problems at important activities at work, school, home or social events? |
| S9u | You kept using alcohol or other drugs even after you knew it was causing or adding to medical, psychological or emotional problems you were having? |
2.4. Analysis
Item values were recoded into binary form, differentiating clients who experienced the respective problem during the past month (1) or not (0). This re-categorization was also used in a previous study on the SPS Canadian English version, where the authors stated that the study focused on binary indicators of symptoms during the past month. (Kenaszchuk et al., 2013). The Rasch model analyses were performed using R Studio and Stata for Windows®.
In the Rasch model, independent variables represent the trait measured (in this case, the severity of substance use-related problems) (Ф) and the “difficulty” of the parameter item (δ). Notice that the word “difficulty” reflects the educational research background of the Rasch model. In psychological research, a better word to describe this parameter would be “rarity”, since the most rarely occurring items are endorsed by the most severe clients, similar to how in a learning assessment, the most difficult questions are answered correctly by the most intelligent individuals who have more of the trait being measured (Chachamovich, 2007).
In the model, the independent variables (the set of items) are combined additively and the scale score is considered sufficient to describe both the individual and the difficulty of each item. The latter is subtracted from the mean subjects ability response. The probability of success (that is, of endorsing the item) – the dependent variable – is computed as the logarithm of the ratio between the probability of success (Pis) and failure (1 – Pis), where i indicates the individual, s the item, Ф the individuals i ability and δ the difficulty of item s ( Chachamovich, 2007):
|
|
If the magnitude of Ф (ability) is equal to δ (difficulty), the probability of success and failure are identical (P = 0.5/0.5). The relationship between Ф and δ defines how the skill can be inferred from an item with known difficulty (Chachamovich, 2007).
Before and after the Rasch analysis, a Principal Components Analysis (PCA) was performed to verify whether the assumption of one-dimensionality was met. One-dimensionality means the measure is a single latent dimension defined by a set of items. Prior to the Rasch analysis, a PCA of the raw scores of the scales is performed to verify the existence of a latent variable. Following the Rasch analysis, a PCA is performed on the residuals of the Rasch model to check if there are any secondary variables after removing the variance of the latent factor.
Finally, a differential item functioning (DIF) analysis was performed in order to diagnose possible differences in the measurement of the latent trait for certain characteristics of the sample. The variables used in this analysis were gender and level of care (inpatient versus outpatient). Previous research on the SPS also performed a DIF analysis (Kenaszchuk et al., 2013).
Lastly, it is important to note that the Rasch model analysis presented here did not include cases in which individuals answered in an extreme way, that is, responded positively or negatively to all items. These cases are eliminated because analysis of them introduces infinite error given it is not possible to measure the exact degree of severity of these individuals.
An individual who responds negatively to all items may have a degree of severity close to the difficulty of the easiest (least severe) item, or even much less severe than that. On the other hand, an individual who responds positively to all items may have a degree of severity slightly larger than the hardest (most severe) item or even much more severe. Thus, the items used do not allow the separation of these cases, restricting an estimate of the severity of those individuals.
3. Results
To initiate the analysis of the SPS scale via the Rasch model, an item characteristic curve (ICC) analysis was performed for each of the 16 items of the scale. The curves show the probability of endorsement for each response category (0 — Never, 1 — More than 12 months ago, 2 — 2–12 months ago or 3 — Past month) by the severity of the individual, estimated by a Rating Scale Rasch Model.
The ICC analysis showed that the intermediate response categories (1 and 2) did not differentiate individuals according to their severity. Less severe individuals were more likely to respond 0, while the most severe individuals are more likely to respond 3. Therefore, for better implementation of the Rasch model, it was necessary to re-categorize response variables. Responses were re-computed as 0 = 0, 1 and 2 and 3 = 1, thus collapsing responses into those categories indicating occurring during the past month (1) or not during the past month (0). This re-categorization was also implemented in a previous study with the Canadian version of the Scale (Kenaszchuk et al., 2013).
Following re-categorization, an exploratory factor analysis was performed using principal component analysis with Varimax rotation, which indicates a one factor solution. The first three eigenvalues were 8.33, 1.44 and 1.01.
Items S9e, S9j, S9m, and S9u have loadings greater than 0.6 on the first factor. Items S9c, and S9d had factor loadings greater than 0.6 on factor 2. Item S9k loaded on factor 3, which may indicate the existence of another, but much less relevant, dimension on the scale. The first factor accounts for 52.06% of the variation in the data, the second factor only 9%, and the third factor only 6.3%.
The adequacy of the data to the Rasch model was verified. As shown in Table 2, the difficulty (in psychological measurement, the “severity”) of the items varied between the values of − 1.81 (item S9e) and 4.08 (item S9k). The values corresponding to the severity of individuals range from − 3.12 to 3.59, with an average severity of 0.29 (SD = 1.72) Table 2 also presents the models infit and outfit values.
| Item | Statistics | Mean Square | ZSTD | ||||||
|---|---|---|---|---|---|---|---|---|---|
| % | Severity | X2 | Df | p-value | Outfit | Infit | Outfit | Infit | |
| s9k | 3.70 | 4.079 | 148.105 | 80 | 0.000 | 1.828 | 0.885 | 0.95 | − 0.17 |
| s9c | 40.74 | 0.917 | 131.573 | 80 | 0.000 | 1.624 | 1.498 | 1.79 | 3.49 |
| s9j | 48.15 | 0.503 | 59.859 | 80 | 0.955 | 0.739 | 0.877 | − 0.98 | − 0.95 |
| s9r | 48.15 | 0.503 | 58.149 | 80 | 0.969 | 0.718 | 0.869 | − 1.08 | − 1.02 |
| s9m | 51.85 | 0.291 | 57.53 | 80 | 0.973 | 0.71 | 0.8 | − 1.18 | − 1.59 |
| s9n | 54.32 | 0.147 | 54.675 | 80 | 0.986 | 0.675 | 0.802 | − 1.38 | − 1.55 |
| s9g | 55.56 | 0.074 | 76.377 | 80 | 0.594 | 0.943 | 0.999 | − 0.15 | 0.04 |
| s9t | 58.02 | − 0.074 | 56.607 | 80 | 0.978 | 0.699 | 0.86 | − 1.26 | − 1.01 |
| s9p | 61.73 | − 0.305 | 118.359 | 80 | 0.003 | 1.461 | 1.143 | 1.64 | 0.99 |
| s9h | 62.96 | − 0.384 | 41.752 | 80 | 1.000 | 0.515 | 0.724 | − 2.14 | − 2.02 |
| s9f | 66.25 | − 0.552 | 72.258 | 79 | 0.691 | 0.903 | 1.022 | − 0.26 | 0.19 |
| s9s | 67.90 | − 0.715 | 49.858 | 80 | 0.997 | 0.616 | 0.797 | − 1.4 | − 1.31 |
| s9u | 69.14 | − 0.802 | 58.525 | 80 | 0.966 | 0.723 | 0.851 | − 0.89 | − 0.9 |
| s9q | 70.37 | − 0.891 | 50.305 | 80 | 0.996 | 0.621 | 0.767 | − 1.26 | − 1.44 |
| s9d | 71.60 | − 0.983 | 148.324 | 80 | 0.000 | 1.831 | 1.61 | 2.1 | 3.03 |
| s9e | 81.48 | − 1.808 | 127.791 | 80 | 0.001 | 1.578 | 1.035 | 1.13 | 0.23 |
Source: Data collection, 2011 and 2014.
The mean square values of infit and outfit indicate that all items fit the Rasch model, though some are unproductive to measurement. None of the SPS scale items have mean square infit or outfit values above 2.
The infit and outfit analyses for individuals shows that no individual has superior infit (a value of 2 or greater), but five individuals possess superior outfit. Of these five, two have Z-score standardized fit statistics (ZSTD) value greater than 2, meaning their result is not random and their answers are not in accordance with the Rasch model. One possibility is that they are severe individuals on the SPS score but have not responded positively to the most severe items; or, they are low severity but responded positively to the most severe items. The number of people in this condition is very low, so it does not generate concern for analysis.
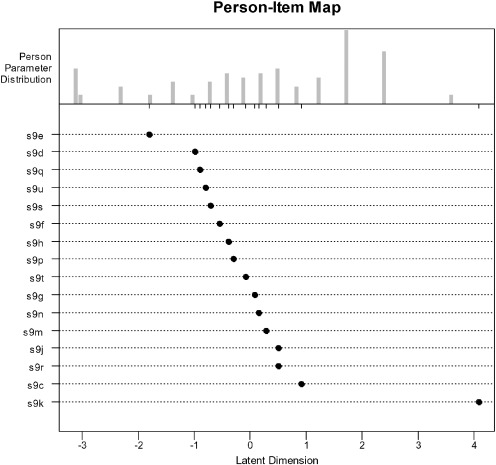
As observed in the person-items map in Fig. 1, the items are not evenly distributed along the latent scale of severity. This could mean that most of the items are of the same severity level, suggestive of redundancy in the scale.
|
|
|
Fig. 1. Person-Items Map, São Paulo, SP, Brasil, 2015. |
An analysis was conducted to check for the presence of differential item functioning (DIF) by gender and level of care (inpatient vs outpatient). Previous studies on the SPS scale also conducted this analysis (Kenaszchuk et al., 2013). Table 3 shows the results of the DIF analysis.
| Item | Gender | Level of Care | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Outpatient | Inpatient | |||||||
| % | Sev | % | Sev | DIF | % | Sev | % | Seve | DIF | |
| s9e | 65% | − 2.36 | 52% | − 0.33 | − 2⁎ | 81% | − 2.55 | 25% | 0.52 | − 3.1⁎ |
| s9d | 57% | − 1.46 | 45% | 0.26 | − 1.7⁎ | 67% | − 1.03 | 30% | − 0.7 | − 0.3 |
| s9q | 49% | − 0.71 | 61% | − 1.6 | 0.9 | 66% | − 0.92 | 30% | − 0.7 | − 0.2 |
| s9u | 49% | − 0.71 | 58% | − 1.1 | 0.4 | 64% | − 0.81 | 30% | − 0.7 | − 0.1 |
| s9s | 48% | − 0.6 | 58% | − 1.1 | 0.5 | 64% | − 0.81 | 28% | − 0.04 | − 0.8 |
| s9f | 47% | − 0.49 | 55% | − 0.68 | 0.2 | 60% | − 0.5 | 30% | − 0.74 | 0.2 |
| s9h | 43% | − 0.16 | 58% | − 1.1 | 0.9 | 56% | − 0.22 | 33% | − 1.46 | 1.2 |
| s9p | 43% | − 0.16 | 55% | − 0.68 | 0.5 | 50% | 0.15 | 40% | − 3.09 | 3.2⁎ |
| s9g | 39% | 0.15 | 48% | − 0.02 | 0.2 | 53% | − 0.03 | 23% | 0.99 | − 1 |
| s9t | 39% | 0.15 | 55% | − 0.68 | 0.8 | 51% | 0.06 | 30% | − 0.7 | 0.8 |
| s9n | 38% | 0.25 | 48% | − 0.02 | 0.3 | 51% | 0.06 | 23% | 0.99 | − 0.9 |
| s9c | 36% | 0.35 | 18% | 2.25 | − 1.9⁎ | 46% | 0.41 | 5% | 3.48 | − 3.1⁎ |
| s9m | 36% | 0.35 | 45% | 0.26 | 0.1 | 44% | 0.5 | 30% | − 0.7 | 1.2 |
| s9j | 32% | 0.65 | 45% | 0.26 | 0.4 | 40% | 0.75 | 30% | − 0.7 | 1.5 |
| s9r | 31% | 0.75 | 48% | − 0.02 | 0.8 | 40% | 0.75 | 30% | − 0.7 | 1.5 |
| s9k | 4% | 4.03 | 3% | 4.31 | − 0.3 | 4% | 4.2 | 3% | 4.24 | 0 |
Notes: n = 81 [by gender – 58 males (out of 77) and 23 females (out of 33)].
n = 81 [by level of care - 62 outpatient (out of 70) and 19 inpatient (out of 40)].
⁎. indicates DIF numbers equal to or greater than 1 that are statistically significant.
In both analyses, only three items have a DIF value higher than 1 and are statistically significant. For level of care, an additional four items have DIF values greater than 1, but without statistically significant difference. For gender, none of other the items have a DIF value greater than 1.
A positive DIF value indicates that an item indicates greater severity for men than women or greater severity for outpatient than inpatient clients.
As observed in Table 3, 13 of the 16 items do not have a DIF value that is statistically significant for level of care. The exceptions are items S9p, S9e, and S9c. This result indicates that the items perform the same for both types of programs, with the exception of the 3 items mentioned. As for gender, items that have a statistically significant DIF are S9c, S9d, and S9e. It is important to point out that the confidence intervals are much higher for females and clients from the inpatient service, since the sample has few non-extreme cases in these categories - there are only 23 women and 19 inpatients. This result indicates that the items perform the same for both genders, with the exception of the 3 items mentioned.
The final principal components analysis of the residuals of the Rasch model presents evidence of a second dimension, as the residuals from the first factor account for 2.3 units of variance, exceeding the first threshold value of 1.9 suggested by the literature (Humphreys & Montanelli, 1975). Items S9c and S9d have loadings greater than 0.6, indicating the multidimensional scale.
4. Discussion
The current application of the Rasch model to the SPS scale replicates the analysis performed with the Canadian English version of the scale. Given the analysis was performed using a binary re-categorization of responses, the results are also limited to two responses (Kenaszchuk et al., 2013). One predominant dimension was identified in the scale, a result which is consistent with previous findings from studies in the USA and Canada using the same scale (Conrad, K. J., et al., 2011 ; Kenaszchuk, C., et al., 2013). However, these previous studies did not acknowledge the presence of a second dimension, which was detected in the present study through an analysis of the residuals. Since the sample sizes of previous studies were much larger than the current studys sample, future research with more cases should be performed.
A reanalysis of the SPS scale without items S9c, S9d, and S9k was completed, but the overall performance of the scale decreased. Item S9d is frequently endorsed by individuals, while Item S9k is endorsed more rarely. This could mean the scale needs both easier (less severe) items and more difficult items in order to better evaluate the severity of individuals.
Item S9c, despite being endorsed frequently by clients, is not identified by the Rasch model as an easy (less severe) item; in fact, it is the second most difficult. This result is understandable, since almost all individuals indicated they tried at some point to hide their use from friends and family. However, when they seek treatment, it is clear that they are no longer hiding this use, since the use-related problems have become very difficult to bear. It is often stated that it is not possible to hide something that causes so much suffering at the time of treatment admission. This could explain why the item is frequently endorsed, but not in the month preceding the start of treatment.
Present results also indicate a redundancy in the items – primarily of medium severity - which could explain the possible lack of low and high severity items. This result was also found in previous studies of the scale done in the USA and Canada (Conrad, K. J., et al., 2011 ; Kenaszchuk, C., et al., 2013). Future studies should investigate replacing some of the redundant items with those of lower and higher severities.
The DIF analysis indicated there was no performance difference on the scale for both gender and level of care in 13 of the 16 items. In the Canadian and American studies, a gender difference was noted, although it was not statistically significant and therefore does not justify administering items differently between genders (Conrad, K. J., et al., 2011 ; Kenaszchuk, C., et al., 2013). In this study, only three items showed differences, and this may be due to the small sample. The present results are consistent with the Canadian results and do not justify applying the scale differently by gender or level of care.
It is important to highlight once more that the number of individuals interviewed using the AGNI-I was 110 - far fewer than in other studies of the scale (Conrad, K. J., et al., 2011; Kenaszchuk, C., et al., 2013 ; Riley, B. B., et al., 2007). Even so, the overall results were consistent with those in other studies. In addition, in the present study, the number of males is a lot higher than the number of female clients. These few differences should be revisited in further studies.
Thus, the analysis of the SPS via the Rasch model yielded similar results to those found in Canada and the USA. Although 3 of the 16 items have infit and outfit values suggesting they are not productive for the measurement, the analysis does not justify any changes in the scale.
Study limitations.
The most relevant limitation of this study refers to the number of cases. Future studies should be carried out with samples greater than 200 subjects, as indicated by the Rasch literature (Linacre, 1994).
In addition, data collection took place in only two treatment programs in the city of São Paulo, thus disallowing generalization. Finally, most clients in the present study were adults. Future studies should also include the elderly and adolescent populations, as well as the use of this instrument in other cities.
5. Conclusions
The outcomes of this study support the validity of using the Brazilian Portuguese version of the SPS scale. The SPS scale seems to have some redundant items and requires including both more severe and less severe items in order to better classify individuals. A difference between men and women on two items of the SPS scales was detected, but it is possible it was due to the low number of women in the sample. In general, the Brazilian Portuguese version of the SPS scale performs similarly to the US and Canadian English versions.
Acknowledgments
We thank Fundação de Amparo à Pesquisa do Estado de São Paulo for the funding of research projects related to this article, grant numbers: 2012/23873-7, 2011/00226-3 and 2010/20741-7.
We also thank Chestnut Health Systems for their help and support throughout this research.
References
- Boone, W. J., et al., 2014 W.J. Boone, J.R. Staver, M.S. Yale; Rasch analysis in the human sciences; (2014)
- Chachamovich, E., 2007 E. Chachamovich; Teoria de Resposta ao Item: Aplicação do modelo Rasch em desenvolvimento e validação de instrumentos em saúde mental; Universidade Federal do Rio Grande do Sul, Porto Alegre (2007)
- Claro, H. G., 2015 H.G. Claro; Validação dos Instrumentos “Avaliação Global das Necessidades Individuais – Inicial e Rastreio Rápido”; Universidade de São Paulo, Escola de Enfermagem da Universidade de São Paulo (2015)
- Claro, H. G., et al., 2012 H.G. Claro, M.A.F. de Oliveira, H.B. Paglione, P.H. Pinho, M.O. Pereira, D. de Vargas; Tradução e adaptação cultural do global appraisal of individual needs-initial; Revista da Escola de Enfermagem da USP, 46 (2012), pp. 1148–1155
- Claro, H. G., et al., 2011 H.G. Claro, M.A.F.d. Oliveira, M.M.d. Almeida, D.d. Vargas, H.B. Paglione; Adaptação cultural de instrumentos de coleta de dados para mensuração em álcool e drogas; SMAD. Revista eletrônica saúde mental álcool e drogas, 7 (2011), pp. 71–77
- Conrad, K. J., et al., 2011 K.J. Conrad, K.M. Conrad, M.L. Dennis, B.B. Riley, R. Funk; Conrad et al 2011 Validation of the substance problem scale to the rasch measurement model; (2011) In
- Dennis, M., 2010 M. Dennis; Global appraisal of individual needs (GAIN): a standardized biopsychosocial assessment tool; 16th Annual Drug Court Training Conference of the National Association of Drug Court Professionals (2010) Boston, MA
- Dennis, M., et al., 2006 M. Dennis, Y. Chan, R. Funk; Development and validation of the GAIN short screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults; The American Journal on Addictions, 15 (Suppl. 1) (2006), pp. 80–91
- Dennis, M., et al., 2008 M. Dennis, T. Feeney, L. Stevens, L. Bedoya; C.H. Systems (Ed.), Global Appraisal of Individual Needs — Short Screener (GAIN-SS): Administration and Scoring Manual, Chestnut Health Systems, Normal - Illinois (2008)
- Dennis, M., et al., 2004 M. Dennis, R. Funk, S. Godley, M. Godley, H. Waldron; Cross-validation of the alcohol and cannabis use measures in the global appraisal of individual needs (GAIN) and timeline followback (TLFB; form 90) among adolescents in substance abuse treatment; Addiction, 99 (Suppl. 2) (2004), pp. 120–128
- Dennis, M., et al., 2003 M. Dennis, M. White, J. Titus, J. Unsicker; Global appraisal of individual needs: administration guide for the GAIN and related measures.; (2003) Bloomington
- Formigoni, M. and Castel, S., 1999 M. Formigoni, S. Castel; Escalas de avaliação de dependência de drogas: aspectos gerais; Revista Brasileira de Psiquiatria, 26 (1999), p. 26
- Gotham, H., et al., 2008 H. Gotham, M. White, H. Bergethon, T. Feeney, D. Cho, B. Keehn; An implementation story: moving the GAIN from pilot project to statewide use; Journal of Psychoactive Drugs, 40 (2008), pp. 97–107
- Henrique, I., et al., 2004 I. Henrique, D. De Micheli, R. Lacerda, L. Lacerda, M. Formigoni; Validation of the Brazilian version of alcohol, smoking and substance involvement screening test (ASSIST); Revista da Associação Médica Brasileira, 50 (2004), pp. 199–206
- Humphreys, L. G. and Montanelli, R. G., 1975 L.G. Humphreys, R.G. Montanelli Jr.; An investigation of the parallel analysis criterion for determining the number of common factors; Multivariate Behavioral Research, 10 (1975), pp. 193–205
- Kenaszchuk, C., et al., 2013 C. Kenaszchuk, T.C. Wild, B.R. Rush, K. Urbanoski; Rasch model of the GAIN substance problem scale among canadian adults seeking residential and outpatient addiction treatment; Addictive Behaviors, 38 (2013), pp. 2279–2287
- Lennox, R., et al., 2006 R. Lennox, M. Dennis, M. Ives, M. White; The construct and predictive validity of different approaches to combining urine and self-reported drug use measures among older adolescents after substance use treatment; The American Journal on Addictions, 15 (2006), pp. 92–101
- Linacre, J. M., 1994 J.M. Linacre; Sample size and item calibration stability; Rasch Measurements Transactions, 7 (1994)
- Moretti-Pires, R. O. and Corradi-Webster, C. M., 2011 R.O. Moretti-Pires, C.M. Corradi-Webster; Adaptação e validação do alcohol use disorder identification test (AUDIT) para população ribeirinha do interior da amazônia, brasil; Cadernos de Saúde Pública, 27 (2011), pp. 497–509
- Riley, B. B., et al., 2007 B.B. Riley, K.J. Conrad, N. Bezruczko, M.L. Dennis; Relative precision, efficiency and construct validity of different starting and stopping rules for a computerized adaptive test: the GAIN substance problem scale; Journal of Applied Measurement, 8 (2007), p. 48
- Titus, J. C., et al., 2012 J.C. Titus, T. Feeney, D.C. Smith, T.L. Rivers, L.L. Kelly, M.L. Dennis, G.C. Center; GAIN-Q3: administration, clinical interpretation, and brief intervention; (2012)
- Titus, J., et al., 2008 J. Titus, M. Dennis, R. Lennox, C. Scott; Development and validation of short versions of the internal mental distress and behavior complexity scales in the global appraisal of individual needs (GAIN); The Journal of Behavioral Health Services & Research, 35 (2008), pp. 195–214
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?