Summary
Objective
We evaluated the efficacy and outcome of laser photoselective vaporization of prostate (PVP) in patients with voiding difficulty due to prostatic obstruction induced by advanced prostate cancer (PC).
Methods
We retrospectively studied the records of 13 patients with advanced PC and prostatic obstruction with a mean prostate volume of 65.0 ml. All of the 13 patients received PVP between 2006 and 2010 due to the symptoms of voiding difficulty or acute urinary retention (AUR; N = 10) refractory to medical treatment. Perioperative safety and functional results were evaluated.
Results
Lasering time ranged from 24 to 20 minutes (mean 67 ± 26), during which 66–423 KJ (mean 172 ± 95) of laser energy was delivered. All patients could resume voiding function with a mean catheterization time of 3.0 days.
Conclusions
Our preliminary results suggest that PVP is a safe and effective procedure for relieving prostatic obstruction without intraoperative blood transfusion, water intoxication, or other complications in patients with advanced prostate cancer.
Keywords
acute urinary retention;cancer;laser;men’s health;photoselective vaporization;prostate;prostate cancer
1. Introduction
Prostate cancer (PC) is a relatively common cancer in older men. Radical prostatectomy and definitive therapy is usually applied to younger patients with localized disease. However, in patients with metastatic disease, androgen-suppressing strategies and active surveillance remains the mainstay of managements.1 Bothersome lower urinary tract symptoms (LUTS), especially aberrant growth of prostatic cancer induced bladder outlet obstruction, have been increasing in men with advanced diseases, significantly impacting their quality of life.
Transurethral resection of the prostate (TURP) has been the standard therapy for relieving bladder outlet obstruction (BOO) due to benign prostatic hyperplasia (BPH) or PC for more than 7 decades.1; 2; 3 ; 4 Safety considerations for TURP in men with PC still remain a major concern, both in surgical and oncological risks.2; 3; 4; 5 ; 6 In the past decade, the use of laser photovaporization of prostate (PVP) has emerged as a well accepted alternative to TURP for relieving BOO caused by BPH.7 ; 8 PVP is considered as efficacious as TURP, offering safety, low morbidity, rapid recovery, immediate and sustained improvement, and long-term durability.7 ; 8 To our knowledge, there have been few published studies regarding to the use of PVP for relieving BOO for advanced PC patients. The purpose of this study was to evaluate the safety and efficacy of PVP in management of advanced PC patients with prostatic obstruction.
2. Materials and methods
We retrospectively reviewed the medical records of 343 patients with voiding difficulty who were refractory to conventional medical treatment and treated with the 120-W GreenLight high performance system (HPS; American Medical Systems, Minnetonka, Minnesota, USA) for the palliation of BOO in our department between March 2006 and January 2010. The standard procedures of PVP were similar to that published previously by Gomez.9 According to the sixth edition of the TNM staging system of the American Joint Committee on Cancer (2002), advanced PC is defined as either stage III or stage IV disease.10 Patients who previously received transurethral surgery such as TURP or urethrotomy were excluded.
Thirteen patients with advanced PC and with refractory voiding difficulty were treated with 120-W GreenLight HPS for the palliation of BOO and were included in this study. A thorough chart review including inpatient and outpatient records was done. The primary diagnosis of PC was made by transrectal ultrosonography (TRUS) guided biopsy in all patients, and tumors were graded using the Gleason score. Serum prostate specific antigen (PSA) was obtained from the time of diagnosis to the end of the follow-up. Advanced PC was diagnosed by bone scan, and/or computed tomography, or magnetic resonance imaging. This study was approved by our institutional review board. Given the retrospective design, informed consent to enter this study was not required.
3. Results
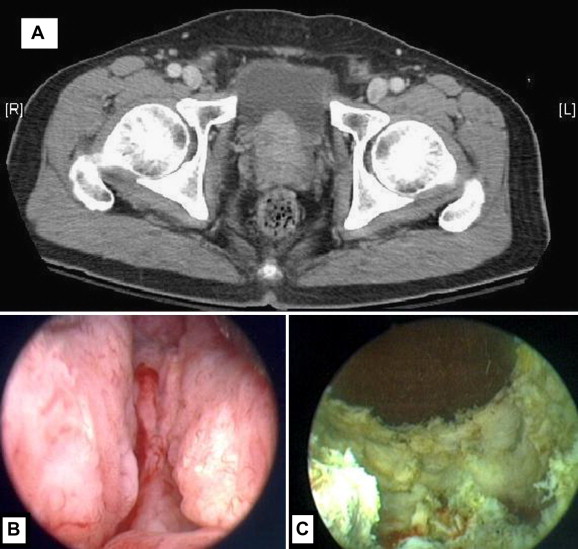
Table 1 shows the demographic details of these patients. Between March 2006 and January 2010, 13 patients with a mean age of 76.5 ± 8.3 years (60–91 years of age) underwent palliative PVP for relieving prostatic obstruction due to advanced PC. Ten out of the 13 patients had a history of urinary retention and needed urethral catheterization. At cancer diagnosis the mean PSA was 1740 ± 3502 (range: 38–12498) ng/ml. PVP was performed under spinal or general anesthesia. Efficient debulking and hemostatic effects was achieved during operation (Fig. 1). There were no intraoperative complications or mortality. Laser time ranged from 24 to 120 (mean 67 ± 26) minutes. Mean 172 ± 95 KJ of laser energy was delivered. The mean follow-up time was 23.4 ± 14.1 months.
| Variable | |
|---|---|
| Patient number | 13 |
| Age at PVP (years) | 76.5 ± 8.3 |
| Preoperative TRUS prostate volume (ml), n = 13 | 65.0 ± 39.2 |
| PSA at diagnosis (ng/ml) | 1740 ± 3502 (13∼12498) |
| Stage at surgery (III/IV) | 4/9 |
| Mean Pre-PVP flow rate (ml/s), n = 6 | 5.0 (3–8) |
| Mean post-PVP flow rate (ml/s), n = 12 | 9.8 (6–17) |
| Mean laser times (minutes) | 67 ± 26 (24–120) |
| Mean laser energy delivered (kJ) | 172 ± 95 (66–423) |
| Perioperative complications | N = 8 |
| Urinary tract infection | 1 |
| Hematuria need to irrigate | 1 |
| Failed initial TWOC | 8 |
| Failed second TWOC | 3 |
| Postoperative outcome | |
| Successful TWOC in 1 mo | 13 |
| Time to successful TWOC (d) | 3.0 ± 1.4 (2–9) |
| Residual urine (ml) | 85 ± 144 (3–434) |
TWOC = trial without catheter.
|
|
|
Figure 1. (A) Preoperative computed tomography showed advanced prostate cancer with extracapsualr invasion; (B) preoperative cystoscopy showed bladder outlet obstruction induced by advanced prostate cancer; (C) postoperative cystoscopy showed relief of bladder outlet obstruction after PVP. |
According to the grading system of complications published by Dindo et al11 only two patients experienced grade II complications, one had urinary tract infection, and the other encountered blood clots needing irrigation. In addition to these two patients, there were another six patients failing initial trial without catheter (TWOC) 1 or 2 days after operation, which could be considered as a grade I complication. Unlike most BPH patients who received PVP who could void 1 day after surgery, our patients took a longer time to accomplish TWOC (mean 3 days). However, all of our patients could void within 1 month of the operation. In addition, 3 of 13 (23.1%) patients received repeated surgical reintervention (TURP or re-PVP, dependent on the availability of PVP) at 2, 15, 29, and 36 months after initial PVP due to tumor bleeding or regrowth. At the time of the latest analysis one patient died from castration-resistant prostate cancer (CRPC) 38 months after PVP and 43 months after the diagnosis of CRPC.
4. Discussion
Bothersome LUTS have been increasing in men with advanced PC and significantly impacted their quality of life. TURP has been the undisputed gold standard therapy for relieving BOO caused by BPH or PC for more than 7 decades. In terms of surgical therapies for relieving BOO due to BPH, PVP had proved to have the same efficacy as TURP, while offering an established safety, low morbidity, rapid recovery, and long-term durability.7 ; 12 Our preliminary results in treating patients with PC and PVP were promising, with excellent safety outcomes and good efficacy. The perioperative complications were relatively mild with PVP. In our series, significant hematuria was negligible except for one patient who needed saline irrigation. Another grade II complication was urinary tract infection, which was solved easily with antibiotics. No patient needed blood transfusion nor did water intoxication happen during PVP.
TURP might cause cancer cells dissemination on locally advanced PC.13 ; 14 Although debates on the potential negative effect remain, TURP has also shown its association with an increase in metastasis and death in patients with advanced PC.4; 13; 14 ; 15 The condition may be related to the procedures of TURP or may be secondary to an unidentified adverse prognostic factor associated with BOO in this subset of patients. The 532-nm GreenLight of HPS is absorbed by the hemoglobin and coagulated arterial and venous bleeders with significant efficiency. This high absorption coefficient accounted for adequate tissue vaporization and coagulation effect on prostate tissue.7; 16 ; 17 The HPS vaporization provided an option for men with prostatic obstruction due to BPH or PC.12 ; 16 In a canine study, no irrigant absorption was detected after PVP.17 This technique brought in not only adequate tissue coagulation on hemostatic effect, but it also brought the possibility to prevent tumor cell dissemination through cutting veins as with TURP.
The functional results in our series were acceptable. The rate of failed TWOC that needs recatheterization was high (61.5%) when we routinely removed the catheter at postoperative Day 1 or 2. In our series, the time to successful catheter removal was 3.0 ± 1.4 (2–9) days. It was longer than 1.7∼1.8 ± 1.5 days in patients with BPH who received PVP in other series,17 ; 18 but was similar to Chang’s5 report (2.69 ± 1.01 days) in palliative TURP for patients with PC. However, it is not a major issue in palliative surgery for advanced PC. What we learned was to remove the catheter 1–2 days later in patients with PC than in patients with BPH, thus all of our patients could accomplish successful TWOC within 1 month after the operation. Compared with a series of palliative TURP in patients with PC, Crain2 reported that 42% failed initial TWOC, there was 8.3% recatheterization, and there was 21% chronic drainage in 19 patients. Our results are promising because all patients achieved successful TWOC within 1 month postoperatively, although high residual urine over 100 ml was noted in three patients. The conditions of two patients experiencing high residual urine (>250 ml) improved after medical treatment with Urecholine and an alpha blocker.
In the palliative TURP series, up to 29% of patients experienced surgical reintervention for bleeding or obstruction,2 and up to 26% of patients needed long-term catheterization.3 A high percentage of failed initial TWOC, a high rate of chronic catheterization, and a high residual urine are found in patients who receive TURP,2; 3; 4 ; 5 and the same results were found in our series of PVP. The comparative data of PVP and another four series of palliative TURP in advanced PC are shown in Table 2.2; 3; 4 ; 5 Risk factors of failed initial TWOC had been postulated as a incomplete channel creation, impaired wound healing, and general health deterioration to patients with advanced PC. Another possibility is the detrusor dysfunction, which is induced by delayed surgical intervention. The immediate functional results of PVP versus TURP (failed initial TWOC: 61.5% in PVP vs. 16.7 to 43.5% in TURP; Table 2) recommend against PVP. However, the current PVP group took advantage of safety and showed no need for blood transfusion and no perioperative mortality. Our results were in line with a randomized clinical trial of 120 patients with BPH that demonstrated no major intraoperative complications; none of the patients in that study required blood transfusion in the PVP group.19 However, among TURP patients, 12 (20%) required transfusion, 3 (5%) developed TUR syndrome, and capsule perforation was observed in 10 patients.19
| PVP | Crain2∗ | Gnanapragasam3 | Marszalek4 | Chang5 | |
|---|---|---|---|---|---|
| Patients (N) | 13 | 19 | 46 | 81 | 14 |
| Mean age at operation | 76.5 | 74 | 72 | 75.9 | 75.8 |
| Pre-op AUR (%) | 76.9 | 13.0 | 34.8 | 30.0 | 100 |
| Post-op RU (ml) | 85 ± 144 | N | N | N | N |
| Post-op UF rate ml/s | 9.8 | 7.38 | 8.8 | N | N |
| Failed TWOC (%) | 61.5 | 42 | 43.5 | N | 16.7 |
| LTC within 1 y | — | 21 | 26.1 | N | N |
| Reoperation | 23.1 | 29 | 10.9 | N | 28.6 |
| Blood transfusion needed (%) | 0 | 10.5 | N | 9.9 | N |
| Peri-op mortality (<30 d), % | 0 | 5.3∗ | N | 2.2 | 0 |
LTC = long-term urinary catheterization; N = not shown; peri-op = perioperative; pre-op = preoperative; post-op = postoperative; RU = residual urine.
∗. One patient committed suicide 5 days after surgery.
There has been a report on the possibility of TURP in promoting the metastasis of PC, and the result of distant metastasis was alarmingly poor, with 38% in TURP versus 13% in needle biopsy after 5 years and 56% versus 22% after 10 years.14 With the characteristics of immediate and efficient photoablation as well as photocoagulation in PVP, the possibility of distant metastasis might be reduced with long-term follow-up.
There are some limitations in this retrospective study. Even in advanced PC, there still are a wide variety of diseases that may prejudice prognosis of treatment, e.g., hormone sensitiveness and the general performance of the patient. It is hard to determine a functional difference without a comprehensive urodynamic study before and after surgical intervention. The number of cases is too small to make a good comprehensive logistic analysis. However, PVP did achieve excellent immediate efficacy and low perioperative morbidity in patients of this disease entity.
5. Conclusions
Our preliminary results suggested that palliative PVP can be performed safely and efficiently for relieving bladder outlet obstruction in patients with advanced PC, and this treatment offers significant improvement in a patient’s voiding function.
References
- 1 A. Heidenreich, G. Aus, M. Bolla, et al.; EAU guidelines on prostate cancer; Eur Urol, 53 (2008), pp. 68–80
- 2 D.S. Crain, C.L. Amling, C.J. Kane; Palliative transurethral prostate resection for bladder outlet obstruction in patients with locally advanced prostate cancer; J Urol, 171 (2004), pp. 668–671
- 3 V.J. Gnanapragasam, V. Kumar, D. Langton, R.S. Pickard, H.Y. Leung; Outcome of transurethral prostatectomy for the palliative management of lower urinary tract symptoms in men with prostate cancer; Int J Urol, 13 (2006), pp. 711–715
- 4 M. Marszalek, A. Ponholzer, M. Rauchenwald, S. Madersbacher; Palliative transurethral resection of the prostate: functional outcome and impact on survival; BJU Int, 99 (2007), pp. 56–59
- 5 C.C. Chang, J.Y. Kuo, K.K. Chen, et al.; Transurethral prostatic resection for acute urinary retention in patients with prostate cancer; J Chin Med Assoc, 69 (2006), pp. 21–25
- 6 P.F. Engelhardt, C.R. Riedl; Re: palliative transurethral prostate resection for bladder outlet obstruction in patients with locally advanced prostate cancer; J Urol, 173 (2005), pp. 324–325
- 7 R.S. Malek, R.S. Kuntzman, D.M. Barrett; Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes; J Urol, 174 (2005), pp. 1344–1348
- 8 C.H. Chen, P.H. Chiang, Y.C. Chuang, W.C. Lee, Y.T. Chen, W.C. Lee; Preliminary results of prostate vaporization in the treatment of benign prostatic hyperplasia by using a 200-W high-intensity diode laser; Urology, 75 (2010), pp. 658–663
- 9 F. Gómez Sancha, A. Bachmann, B.B. Choi, S. Tabatabaei, G.H. Muir; Photoselective vaporization of the prostate GreenLight PV: lessons learnt after 3500 procedures; Prostate Cancer Prostatic Dis, 10 (2007), pp. 316–322
- 10 F.L. Greene, D.L. Page, I.D. Fleming, et al.; Prostate American Joint Committee on Cancer: AJCC Cancer Staging Manual (6th ed), Springer, New York, NY (2002), pp. 309–316
- 11 D. Dindo, N. Demartines, P.A. Clavien; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey; Ann Surg, 240 (2004), pp. 205–213
- 12 P.H. Chiang, C.H. Chen, C.H. Kang, Y.C. Chuang; GreenLight HPS laser 120-w versus diode laser 200-w vaporization of the prostate: comparative clinical experience; Lasers Surg Med, 42 (2010), pp. 624–629
- 13 G.E. Hanks, S. Leibel, S. Kramer; The dissemination of cancer by transurethral resection of locally advanced prostate cancer; J Urol, 129 (1983), pp. 309–311
- 14 H.M. Sandler, G.E. Hanks; Analysis of the possibility that transurethral resection promotes metastasis in prostate cancer; Cancer, 62 (1988), pp. 2622–2627
- 15 D.G. McGowan; The adverse influence of prior transurethral resection on prognosis in carcinoma of prostate treated by radiation therapy; Int J Radiat Oncol Biol Phys, 6 (1980), pp. 1121–1126
- 16 R. Ruszat, M. Seitz, S.F. Wyler, et al.; GreenLight laser vaporization of the prostate: single-center experience and long-term results after 500 procedures; Eur Urol, 544 (2008), pp. 893–901
- 17 R.S. Kuntzman, R.S. Malek, D.M. Barrett, D.G. Bostwick; Potassium-titanyl-phosphate laser vaporization of the prostate: A comparative functional and pathologic study in canines; Urology, 484 (1996), pp. 575–583
- 18 R. Ruszat, S. Wyler, H.H. Seifert, et al.; Photoselective vaporization of the prostate: subgroup analysis of men with refractory urinary retention; Eur Urol, 505 (2006), pp. 1040–1049
- 19 A. Al-Ansari, N. Younes, V.P. Sampige, et al.; GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up; Eur Urol, 58 (2010), pp. 349–355
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?