Summary
Tuberculous peritonitis (TBP) is a continuing problem in populations with high prevalence of tuberculosis and is difficult to diagnose early. Here, we report a case of confirmed TBP that presented as intestinal ileus and pneumatosis intestinalis. The 79-year-old woman had a history of atrial fibrillation, chronic ischemic heart disease, and chronic renal failure (chronic kidney disease, stage V). She complained of abdominal fullness and pain for 1 week prior to hospitalization. A computed tomography (CT) scan revealed pneumatosis intestinalis. Laparoscopic surgery was performed, and multiple whitish nodules covering the peritoneum were discovered. Biopsy results were consistent with caseating granulomatous inflammation. A modified anti-tuberculosis regimen (isoniazid, 300 mg daily; rifampicin 600 mg daily; ethambutol 800 mg three times per week; and pyrazinamide 1200 mg three times per week) was initiated, stabilizing the condition of the patient. The total duration of anti-tuberculosis therapy was 12 months, with patient condition gradually improving to normal. The elderly, uremic patients recovered fully after the modified anti-tuberculosis regimen for 12 months. For clinical practice, we developed a decision-making algorithm for patients suspecting TBP.
Keywords
Intestinalis ; Obstructive ileus ; Pneumatosis ; Tuberculous peritonitis
Introduction
Tuberculous peritonitis (TBP) is a continuing problem in populations with a high prevalence of tuberculosis (TB). According to reports by the World Health Organization, one-third of the world population is at risk for TB. In the 1990s, more than 30 million people died of TB, particularly in Asia and Africa [1] . Abdominal TB is one of the most common forms of extrapulmonary TB [2] , with TBP usually diagnosed late due to lack of specific symptoms and laboratory findings. Intestinal obstruction and pneumatosis intestinalis are seldom reported as the major manifestations of TBP.
In 75% of patients, acute intestinal obstructions result from many conditions that must be differentiated, included adhesive bands secondary to previous abdominal surgery, adynamic intestinal obstruction, and primary intestinal pseudo-obstruction [3] . Some cases of mechanical intestinal obstruction require surgical intervention. Clinical presentation, laboratory reports, and radiographic studies are sometimes used to decide between surgery and non-surgical treatment [3] .
Here, we report a case of confirmed TBP presenting as intestinal obstruction and pneumatosis intestinalis.
Case Report
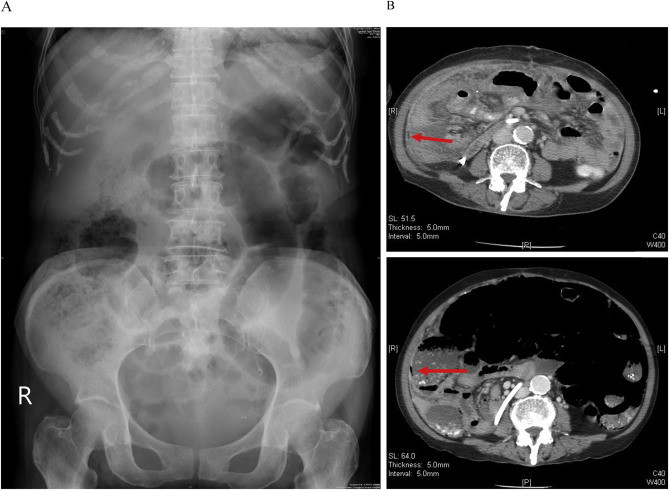
A 79-year-old woman with a history of atrial fibrillation, chronic ischemic heart disease, and chronic renal failure (chronic kidney disease, stage V) complained of abdominal fullness and pain for 1 week prior to hospitalization. The characteristics of her abdominal pain were as follows: located at the umbilical area, 1–2 hours in duration, an onset-to-maximal intensity interval of seconds, a frequency of 2–3 times/day, aggravated by feeding, and relieved by rest. The abdominal pain became more severe and frequent with additional nausea and vomiting, and fever developed 1 day before hospitalization. Subsequently, she was brought to the emergency department (ED) of our institute for help. At the ED, vital-sign measurements were: blood pressure, 100/90 mmHg; temperature, 37°C; pulse rate, 110 beats/min; and respiratory rate, 20 breaths/min. The patient appeared acutely ill, and the abdomen was distended and ovoid. There was radiation pain and tenderness to her back, and abdominal fullness over the right quadrant area (negative Murphys sign), but no rebounding pain. Initial laboratory data at the ED showed a white blood cell count of 2900/μL, with 68.1% neutrophils, 8.7 g/dL hemoglobin level, 97,000/μL platelet count, 19.8 s prothrombin time with an international normalized ratio of 1.84, 140 mm/h erythrocyte sedimentation rate (ESR), 7.1 mg/dL C-reactive protein level, 73 U/L serum amylase level, 2.56 mg/dL total bilirubin level, 156 U/L glutamic-pyruvic transaminase level, 94 μg/dL ammonia level, 55 mg/dL urea nitrogen level, and 6.13 mg/dL serum creatinine level. A kidney, ureter, and bladder (KUB) X-ray showed excessive bowel gas retention and no free air (Figure 1 A). Abdominal ultrasound (US) revealed small ascites, a minute liver cyst, and small calcification spots in S8. Her initial chest film revealed no definite active lung lesion. The patient was admitted under a tentative diagnosis of intestinal obstruction. Nulla per os and fluid hydration were administered immediately, and the acuity and progress of the intestinal obstruction were monitored. Acute-on-chronic renal failure and lung edema developed after fluid hydration, and the patient was transferred to the intensive care unit (ICU) due to respiratory failure. Ceftriaxone (2000 mg/day) plus azithromycin and furosemide for 3 days was prescribed for possible pneumonia and pulmonary edema during this period. Coma and tremor due to uremic encephalopathy were noted, and hemodialysis was performed due to possible uremic encephalopathy. Serial follow-up KUB showed excessive bowel gas retention without significant dilatation of the bowel loops, and colonoscopy (up to the cecum) revealed internal hemorrhoids and redundant colon. Laxatives, neostigmine (0.25 mg intramuscular injection once daily) and oral erythromycin (250 mg four times daily) were prescribed. Fever, tachypnea, and hypoxemia developed, and follow-up CT showed air collection in the bowel wall from the jejunum to the ascending colon without obstructive level ( Figure 1 B). Laparoscopic surgery was performed, and the findings revealed multiple whitish nodules covering the peritoneum. Pathological analysis of the peritoneal nodules revealed caseating granulomatous inflammation. TBP was suspected, and an anti-tuberculosis regimen, including Rifinah 300/150 (Peili, Taichung, Taiwan; 300 mg/day rifampicin plus 150 mg/day isoniazid), ethambutol (Peili, Taichung, Taiwan; 800 mg three times per week), and pyrazinamide (Peili; 1200 mg three times per week), and a modified HERZ regimen (rifampicin + isoniazid + ethambutol + pyrazinamide) were empirically initiated according to guidelines for TB treatment [4] . The condition of the patient stabilized and she was transferred to a ward after a 2-week ICU stay. The modified HERZ regimen was continued after ascitic fluid and tissue cultures were positive for Mycobacterium tuberculosis 1 month later. The total duration of the modified HERZ regimen was 12 months, and the patient recovered fully.
|
|
|
Figure 1. Images of the patient consistent with tuberculous peritonitis. (A) Kidney, ureter, and bladder X-ray showing increased bowel gas. (B) Computed tomography indicating thickened peritoneum with mild ascites and air collection (arrow) in the bowel wall from the jejunum to the ascending colon and suspected pneumatosis intestinalis. |
Discussion
To our knowledge, this is the first case report of TBP presenting as intestinal obstruction and pneumatosis intestinalis in central Taiwan. Invasive techniques following peritoneal biopsy are usually needed to confirm TBP [7] . Sotoudehmanesh et al [8] reported diagnosing 50 (74%) patients with laparotomy and laparoscopy [8] . Laparoscopic examination is the most important method of diagnosis, and our experience is the same as that reported by Bhargava et al [5] .
Patients with TBP may present with fever, abdominal pain, abdominal distension, and weight loss. Sanai et al [9] reported the cumulative data of clinical features, various diagnostic tests, and image findings from 39 TBP studies, finding that the laparoscopic method was the most sensitive for diagnosing TBP (Table 1 ) [9] . The most common complication of TBP is intestinal obstruction, as in the present case. Early diagnosis and treatment are expected to decrease TBP-related mortality and morbidity.
| Item | Frequencya (%) | Cumulative number of cases |
|---|---|---|
| Clinical feature | ||
| Ascites | 73 | 1405 |
| Abdominal pain | 64.5 | 1284 |
| Weight loss | 61 | 774 |
| Fever | 59 | 1393 |
| Positive tuberculin skin test | 53.2 | 380 |
| Abdominal tenderness | 47.7 | 329 |
| Hepatomegaly | 28.2 | 319 |
| Diarrhea | 21.4 | 630 |
| Splenomegaly | 14.3 | 189 |
| Constipation | 11 | 319 |
| Image | ||
| Abnormal chest film | 38 | 1002 |
| Laboratory examinations for ascitic fluid tests | ||
| LDH | 77 | 87 |
| ADA | 94 | 1305 |
| Predominant lymph | 68.3 | 477 |
| Culture | 34.8 | 446 |
| Smear | 2.93 | 615 |
| Laparoscopic method | ||
| Histologic diagnosis | 93 | 402 |
| Visual diagnosis | 92.7 | 397 |
ADA = adenosine deaminase; LDH = lactate dehydrogenase.
a. The estimated sensitivity of a clinical test refers to the ability of the test to correctly identify patients with tuberculous peritonitis [9] .
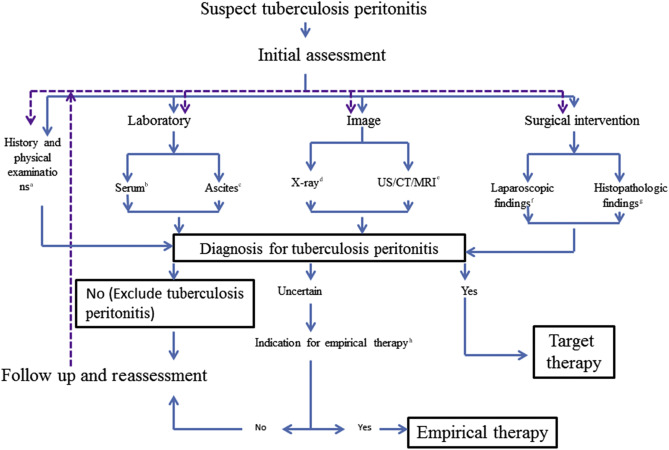
An algorithm for diagnosing and treating TBP was developed after reviewing the literature and our own experience [2] ; [4] ; [5] ; [6] ; [9] ; [10] (Figure 2 , Table 1 ). Accurate diagnosis and adequate treatment of TBP can improve outcomes. Patients selected for conservative treatment without surgery should be monitored closely with serial clinical examinations, ESR tests, and US, magnetic resonance imaging, or CT. Optimal care involves early diagnosis with imaging, the administration of appropriate anti-tuberculosis regimens, and risk assessments of concurrent conditions. Surgical intervention may still be considered in some cases.
|
|
|
Figure 2. Algorithm for the evaluation of patients with suspected tuberculous peritonitis. a Indicators of possible tuberculous peritonitis include abdominal pain, fever, weight loss, diarrhea, constipation, ascites, hepatomegaly, splenomegaly, and history of exposure to tuberculosis. b Serological indicators of tuberculous peritonitis include IGRA. Two kinds of IGRA are approved by the U.S. Food and Drug Administration and available in Taiwan. They are the QuantiFERON–TB Gold In-Tube test and the T-SPOT TB test. Additionally, the tuberculin skin test (Mantoux tuberculin skin test) is available in Taiwan. c Ascites examination results suggesting tuberculous peritonitis include lymphocyte-predominant white cell count, low serum ascites albumin gradient, high adenosine deaminase level, positive smear (acid-fast stain and Ziehl–Neelsen stain), mycobacterial culture, and polymerase chain reaction. d X-ray results suggesting tuberculous peritonitis include abnormal chest films with possible pulmonary tuberculosis. e US/CT/MRI results suggesting tuberculous peritonitis include hypervascular peritoneum, loop matting, omental masses, and thickened mesentery (>15 mm) with mesenteric lymph nodes [4] . f Laparoscopic findings suggesting tuberculous peritonitis include: (1) thickened and hyperemic peritoneum with ascites and whitish miliary nodules scattered over the parietal peritoneum, omentum, and bowel loops; (2) thickened and hyperemic peritoneum with ascites and adhesions; and (3) markedly thickened parietal peritoneum with possibly yellowish nodules and cheesy material and multiple thickened adhesions [5] . g Histopathological findings suggesting tuberculous peritonitis include granuloma with epithelioid macrophages and Langhans giant cells, as well as lymphocytes and plasma cells. h Indications for empirical therapy include high risk for transmission (for example, a combination of a lung lesion with possible tuberculosis) and high risk for fatality (such as a possible tuberculosis diagnosis combined with a critical condition) [6] . Abbreviation: IGRA = interferon-gamma release assay; US/CT/MRI = ultrasound/computed tomography/magnetic resonance therapy; TB = tuberculosis. |
The elderly, uremic patients recovered fully after the modified anti-tuberculosis regimen for 12 months. For clinical practice, we developed a decision-making algorithm for patients suspecting TBP.
Conflicts of interest
All authors declare no conflicts of interest.
Acknowledgments
The authors thank Dr. Chen-Te Chou at the Department of Medical Image of Changhua Christian Hospital for the interpretation of medical images. The authors wish to express their gratitude to the staff of the Division of Infectious Diseases, Division of Critical Care Medicine, and Division of Gastroenterology of Changhua Christian Hospital who were abundantly helpful and offered patient care, invaluable assistance, and support.
References
- [1] WHO; Tuberculosis control and research strategies for the 1990s. Memorandum from a WHO meeting; Bull WHO, 70 (1992), pp. 17–21
- [2] A.C. Tanrikulu, M. Aldemir, F. Gurkan, A. Suner, C.E. Dagli, A. Ece; Clinical review of tuberculous peritonitis in 39 patients in Diyarbakir, Turkey; J Gastroenterol Hepatol, 20 (2005), pp. 906–909
- [3] W. Silen; Acute intestinal obstruction; D.L. Longo, A.S. Fauci, D.L. Kasper, S.L. Hauser, J. Jameson, J. Loscalzo (Eds.), Harrisons principles of internal medicine (18th ed.), McGraw-Hill, New York, NY (2012) Available at: http://accessmedicine.mhmedical.com/content.aspx?bookid=331&Sectionid=40727093 [accessed 17.06.15]
- [4] F.B. Demirkazik, O. Akhan, M.N. Ozmen, D. Akata; US and CT findings in the diagnosis of tuberculous peritonitis; Acta Radiol, 37 (1996), pp. 517–520
- [5] D.K. Bhargava, S. Shriniwas, P. Chopra, S. Nijhawan, S. Dasarathy, A.K. Kushwaha; Peritoneal tuberculosis: laparoscopic patterns and its diagnostic accuracy; Am J Gastroenterol, 87 (1992), pp. 109–112
- [6] C.D.C. Taiwan; Taiwan guideline on TB diagnosis and treatment; (5th ed.)Taiwan Centers for Disease Control, Taipei (2013)
- [7] O.U. Bayramicli, G. Dabak, R. Dabak; A clinical dilemma: abdominal tuberculosis; World J Gastroenterol, 9 (2003), pp. 1098–1101
- [8] R. Sotoudehmanesh, N. Shirazian, A.A. Asgari, R. Malekzadeh; Tuberculous peritonitis in an endemic area; Dig Liver Dis, 35 (2003), pp. 37–40
- [9] F.M. Sanai, K.I. Bzeizi; Systematic review: tuberculous peritonitis-presenting features, diagnostic strategies, and treatment; Aliment Pharmacol Ther, 22 (2005), pp. 685–700
- [10] M.C. Raviglione; Tuberculosis; D. Kasper, A. Fauci, S. Hauser, D. Longo, J. Jameson, J. Loscalzo (Eds.), Harrisons principles of internal medicine (19th ed.), McGraw-Hill, New York, NY (2015) Available at: http://accessmedicine.mhmedical.com/content.aspx?bookid=1130&Sectionid=79737003 [accessed June 18, 2015]
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?