Summary
We report a 27-year-old female with chronic iron deficiency anemia and unexplained fecal occult blood. Abdominal ultrasonography and computed tomography disclosed a possible endoluminal lesion in the small intestine. Single-balloon enteroscopy detected the target lesion in the proximal ileum. The lesion was a 2.5-cm submucosal tumor that was purple-red, soft, had a narrow base, and exhibited superficial telangiectasia. After endoscopic marking, the tumor was resected with minimally invasive laparoscopy. It was histologically confirmed as a cavernous hemangioma. In this report, we discuss the endoscopic characteristics, surgical and pathological assessment, and management strategy of hemangiomas in the small intestine.
Keywords
Endoscopy ; Hemangioma ; Obscure gastrointestinal bleeding ; Small intestine
Introduction
Hemangioma is rare among primary small intestinal tumors and can present as an infrequent cause of obscure gastrointestinal bleeding [1] ; [2] . A preoperative diagnosis has seldom been possible owing to the tumors deep location that is often beyond the reach of regular endoscopy [2] . Thus, most cases reported in the literature were diagnosed with surgical exploration. With the recent advent of newer techniques such as balloon-assisted enteroscopy [3] , endoscopic diagnosis or even resection of small intestinal hemangiomas is becoming feasible. However, the proposed diagnostic features vary between experienced endoscopists, and the evolution of nonsurgical treatment options has led to new controversy [4] ; [5] . We report a case of a presurgically diagnosed ileal hemangioma as a source of chronic gastrointestinal blood loss, demonstrate its endoscopic features, and discuss the risk of endoscopic tumor resection from a pathological prospective.
Case report
A 27-year-old female was referred to our gastroenterology department for obscure gastrointestinal bleeding. Prior to referral, she had been continuously treated in the hematology clinic for unexplained chronic iron deficiency anemia since she was a teenager. Over the years, her treatment consisted of oral iron therapy and occasional transfusions. She experienced significant anemic symptoms episodically, which somewhat interfered with her social life. She had denied abdominal symptoms, melena, hematochezia, bowel habit changes, and body weight loss. She was on no medications, other than iron preparations. On presentation, physical examination was only remarkable for generalized pallor. Laboratory studies showed a hemoglobin level of 4.6 g/dL, a mean corpuscular volume of 60.5 fL, and decreased iron stores [iron level, 9 μg/dL (normal range, 50–212 μg/dL); total iron-binding capacity, 392 μg/dL (275–332 μg/dL); transferrin saturation, 2.29%; ferritin level, 1.99 ng/mL (3–151 ng/mL)]. Hemoglobin electrophoresis results were normal. In the previous 5 months, her transfusion requirements had increased. During this time, four separate fecal occult blood tests were positive. However, esophagogastroduodenoscopy and colonoscopy did not identify any potential source of blood loss. Therefore, a bleeding source in the small intestine was suspected.
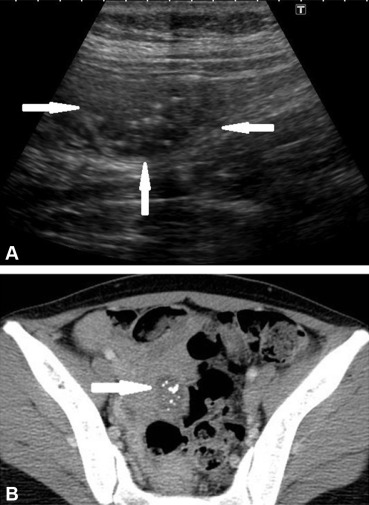
We first performed intestine-targeted transabdominal ultrasonography, which disclosed a questionable 2-cm hypoechoic, compressible, endoluminal tumor superficially located 5 cm below the umbilicus (Fig. 1 A). Subsequent computed tomography (CT) further characterized the lesion as a 2.5 cm contrast-enhancing, small intestine-bound tumor with internal calcifications in the lower peritoneal cavity (Fig. 1 B). There were no other findings or additional calcifications along the intestines.
|
|
|
Figure 1. (A) Transabdominal ultrasonography shows a 2-cm hypoechoic lesion (arrows) within the ileal lumen, which contains internal calcifications (that appear as bright dots). (B) Computed tomography reveals that the lesion is 2.5 cm with soft tissue density and scattered internal calcifications arising from the small intestine (arrow). |
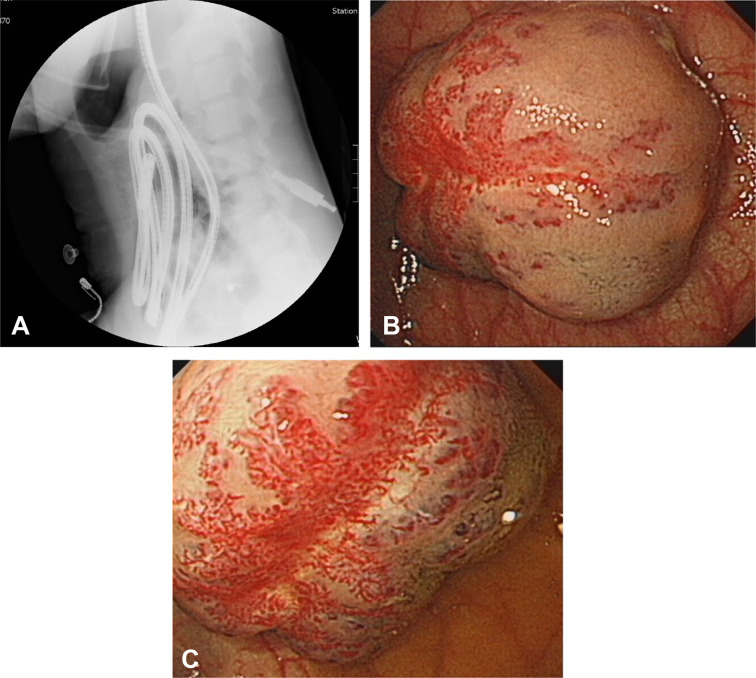
Enteroscopy was performed for presurgical marking, and possible histological evaluation. Using a SIF-Q260 enteroscope with ST-SB1 splinting tube (Olympus Co., Tokyo, Japan) via an antegrade approach, the target lesion was successfully accessed near the insertion limit of the endoscope. This location was judged as the proximal ileum (approximately 300 cm beyond ligament of Treitz) under fluoroscopic guidance (Fig. 2 A). The lesion was a purple-red, soft, depressible, semipedunculated tumor that exhibited superficial telangiectasia (Fig. 2 B and C). Biopsy was thought unnecessary.
|
|
|
Figure 2. (A) Fluoroscopy of the endoscope at the end of insertion suggests a target lesion in the proximal ileum. (B, C) Single-balloon enteroscopy shows a purple-red, soft, depressible, pedunculated mass with superficially dilated capillaries and varicosities in the proximal ileum. |
Endoscopic tattoos with India ink were applied adjacent to the lesion. Additional marking with hemoclipping was applied to allow intraoperative fluoroscopy guidance whenever necessary.
Surgical resection of the tumor was performed on the day after enteroscopy, using the minimally invasive single-port laparoscopy technique [6] . The lesion was easily visualized at surgery, and appeared as a well-defined reddish bulge on the antimesenteric ileal serosa (Fig. 3 A). There was no additional finding during surgical exploration. Ileal segmental resection was performed. The main bulk of the tumor was endoluminal (Fig. 3 B).
|
|
|
Figure 3. (A) On laparoscopic exploration, the lesion is identified as a vascular bulge at the antimesenteric side of the ileal serosa. The surrounding black areas are endoscopic markings by carbon ink. (B) The luminal side of the lesion. Three endoscopy-applied hemoclips are visible close to the tumor. |
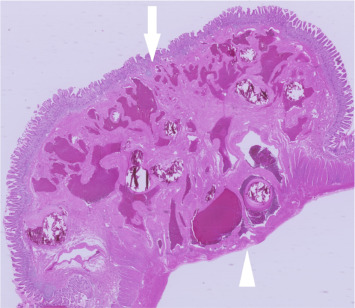
Histological examination confirmed a cavernous hemangioma (Fig. 4 ). At the 4-month follow up, the patient exhibited a spontaneously rising hemoglobin level, which indicated successful cessation of blood loss.
|
|
|
Figure 4. Histological examination shows that the tumor is composed of variably congested and tortuous vascular spaces lined by endothelial cells, which indicates a cavernous hemangioma. The arrow shows the subepithelial boundary and the arrow head shows the subserosal boundary of the tumor. |
Discussion
Hemangioma of the small intestine accounts for 7–10% of all small intestinal benign neoplasms [1] ; [2] ; [7] . It is histologically classified as “cavernous”, “capillary”, or “mixed-type”, based on the size of the affected vessels [2] . Occult chronic gastrointestinal bleeding and iron deficiency anemia are the more common presentations, whereas intussusception and intestinal obstruction are less common presentations [2] . Technical advances have allowed entrance into previously unexplored areas of the deep intestines; therefore, the diagnostic skills to recognize hemangiomas are becoming more attainable for endoscopists. Similar to our patient, previous endoscopy reports of intestinal hemangiomas have described them as typically submucosal [1] ; [2] ; [4] ; [5] ; [8] , purple to red [4] ; [5] ; [9] , soft [5] ; [9] , and pedunculated [4] ; [9] or sessile [8] . It is remarkable that superficial capillary networks and fine varicosities in our patient strongly suggested the vascular nature of the lesion. Characteristic endoscopic signs have often led to a straightforward diagnosis by experienced endoscopists [10] , which can bypass the need for a biopsy and risk of bleeding complications, avoid further image studies, and allow an immediate decision for an ultimate treatment.
Individual case reports have been published that demonstrate the feasibility and safety of endoscopic snare polypectomy or endoscopic mucosal resection in the treatment of intestinal hemangiomas [2] ; [3] ; [4] ; [9] , and stress the advantages of a nonsurgical approach. However, there have been no studies to estimate the true complication rates of these techniques. The highly vascular nature of hemangiomas inevitably raises the concern of bleeding complications. Furthermore, our case and some cases previously reported [6] have shown an alarmingly unpredictable depth of intestinal wall involvement, even if the tumor morphology is suitable for snaring. Based on our surgical and histological findings, which showed subserosal involvement, we believe that significant bleeding or perforation would have occurred if the tumor had been resected endoscopically. We therefore recommend a careful selection of tumors with an unequivocal stalk or sessile tumors with clear image evidence to exclude deep mural involvement prior to endoscopic resection [3] .
In conclusion, we have presented a case of a solitary ileal cavernous hemangioma as the source of obscure gastrointestinal bleeding. By using balloon-assisted enteroscopy, the lesion was promptly located, diagnosed, and marked prior to surgical resection. Endoscopic signs that are diagnostic of a small intestinal hemangioma is a tumor that is submucosal, appears purple-red, is soft, and is covered with superficial telangiectasia. Endoscopic resection may be performed after carefully ruling out transmural extension.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] P.J. Garvin, V. Herrmann, D.L. Kaminski, V.L. Willman; Benign and malignant tumors of the small intestine; Curr Probl Cancer, 3 (1979), pp. 1–46
- [2] P.S. Ramanujam, K.S. Venkatesh, L. Bettinger, J.T. Hayashi, M.C. Rothman, M.J. Fietz; Hemangioma of the small intestine: case report and literature review; Am J Gastroenterol, 90 (1995), pp. 2063–2064
- [3] A. May, L. Nachbar, J. Pohl, C. Ell; Endoscopic interventions in the small bowel using double balloon enteroscopy: feasibility and limitations; Am J Gastroenterol, 102 (2007), pp. 527–535
- [4] T. Shibuya, T. Osada, H. Mitomi, T. Takeda, O. Nomura, H. Nakayama, et al.; Jejunal capillary hemangioma treated by using double-balloon endoscopy (with video); Gastrointest Endosc, 72 (2010), pp. 660–661
- [5] J.J. Easler, G.I. Papachristou; A case of obscure gastrointestinal bleeding; Gastroenterology, 142 (2012), p. 700 1044
- [6] M. Pera, L. Márquez, J.M. Dedeu, J. Sánchez, M. Garcia, J.M. Ramón, et al.; Solitary cavernous hemangioma of the small intestine as the cause of long-standing iron deficiency anemia; J Gastrointest Surg, 16 (2012), pp. 2288–2290
- [7] T. Akamatsu, Y. Matsuda, E. Tsugane, K. Matsuzawa, O. Hasebe, S. Furuta, et al.; A case of multiple cavernous hemangioma of the small intestine and clinical review of the Japanese literature; Gastroenterol Jpn, 25 (1990), pp. 494–498
- [8] N. Nishiyama, H. Mori, H. Kobara, S. Fujihara, T. Nomura, M. Kobayashi, et al.; Bleeding duodenal hemangioma: morphological changes and endoscopic mucosal resection; World J Gastroenterol, 18 (2012), pp. 2872–2876
- [9] M.H. Lee, H.H. Yen, Y.Y. Chen, C.J. Chen, M.S. Soon; Combined capillary hemangioma and angiodysplasia of the ileum: an unusual cause of obscure gastrointestinal bleeding with preoperative localization by double-balloon endoscopy; Am J Surg, 200 (2010), pp. e30–e32
- [10] S. Kimura, S. Tanaka, H. Kusunoki, Y. Kitadai, M. Sumii, S. Tazuma, et al.; Cavernous hemangioma in the ascending colon treated by endoscopic mucosal resection; J Gastroenterol Hepatol, 22 (2007), pp. 280–281
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?