Summary
Systemic sclerosis is a multisystem autoimmune rheumatic disorder characterized by fibrosis in the skin and internal organs but rarely with hepatic or brain involvement. Reversible posterior leukoencephalopathy syndrome is characterized by a unique pattern of brain vasogenic edema in the setting of neurotoxicity predominantly in the parietal and occipital regions. We report a case of systemic sclerosis associated with probable autoimmune hepatitis that progressed rapidly to reversible posterior leukoencephalopathy syndrome with loss of vision, seizures, and coagulopathy. Brain computed tomography showed faint low density in the bilateral occipital lobes and posterior parietal lobes with edematous change. Fortunately, the patients clinical condition considerably improved 2 days following the initiation of 100 mg intravenous hydrocortisone infusion.
Keywords
ERCP ; Jaundice ; PRES ; Steroid
Introduction
Systemic sclerosis (SS) is a systemic disorder characterized by inflammation, fibrosis and degeneration of the skin, blood vessels, and internal organs [1] . Nearly all patients with SS have peripheral vascular involvement with Raynaud syndrome, and >80% experience gastrointestinal function change such as dysphagia. SS rarely has hepatic involvement especially autoimmune hepatitis. Rodrigues et al [2] reported a patient with diffuse SS who was diagnosed with autoimmune hepatitis and who had an excellent response to immunosuppressive drugs.
Reversible posterior leukoencephalopathy syndrome (RPLS), or posterior reversible encephalopathy syndrome, is characterized by a unique pattern of brain vasogenic edema in the setting of neurotoxicity predominantly in the parietal and occipital regions [3] . It may develop in patients with immunosuppressed conditions and various rheumatologic diseases. Fugate et al [4] noticed that a substantial proportion of patients with RPLS had underlying autoimmune disorders. They described focal regions of symmetric hemispheric edema on computed tomography (CT) or magnetic resonance images [5] . However, the etiology of presentation was unknown; underlying vasculitis, cerebral autoregulation disorder, and hypertensive encephalopathy were considered [6] . RPLS is reversible and is characterized by headaches, decreased alertness, altered mental status, seizures, and visual loss.
We present a patient with underlying SS who developed acute liver injury, seizure, and visual loss, and whose condition considerably improved following hydrocortisone intravenous infusion.
Case report
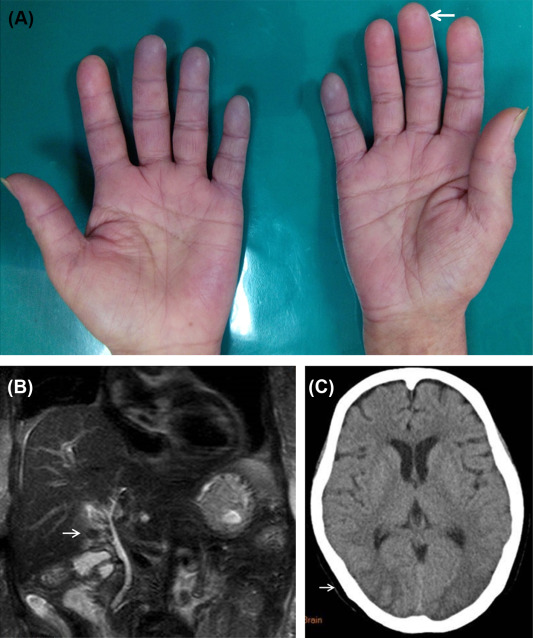
A 71-year-old woman experienced nausea, vomiting, and intermittent epigastric pain for 10 days accompanied by general malaise, poor appetite, and tea-colored urine. She was previously diagnosed with early progressive SS and hypertension at outpatient clinics and was maintained with 4 mg methylprednisolone and 8 mg candesartan daily. She had not taken any new drugs or herbal medicine or consumed alcohol prior to presentation. The patient was afebrile when she visited the emergency department. Her initial vital signs were a body temperature of 36.3°C, pulse rate of 63 beats/min, and respiratory rate of 18 breaths/min. She had icteric sclera and yellowish skin. She presented with Raynaud phenomenon affecting the fingers, with a digital pitting scar (Figure 1 A) and sclerodactyly. The initial biochemistry evaluation revealed the following: total/direct bilirubin, 9.9/6.9 mg/dL (normal range 0.3–1.2/0.1–0.5 mg/dL); aspartate/alanine transaminase, 412/282 IU/L (normal range 15–41/14–41 IU/L); alkaline phosphatase, 854 IU/L (normal range 38–126 IU/L); gamma-glutamyl transpeptidase, 649 IU/L (normal range 7–50 IU/L); blood urea nitrogen, 43 mg/dL (normal range 8–20 mg/dL); creatinine, 3.7 mg/dL (normal range 0.4–1.2 mg/dL); amylase, 285 mg/dL (normal range 28–100 mg/dL); lipase, 82 mg/dL (normal range 22–51 mg/dL); white blood cells, 10,000/μL (normal range 4000–10,000/μL); platelets, 237,000/μL (normal range 140,000–450,000/μL); lactate dehydrogenase, 283 IU/L (normal range 93–192 IU/L); and antinuclear factor 640X+ (normal range < 40+). The following serology tests were negative: viral hepatitis A, B, and C, herpes simplex virus 1, cytomegalovirus, Epstein–Barr virus, rheumatic factor, immunoglobulin G, C3, C4, anti-ds-DNA, antimitochondrial antibody, and antismooth muscle antibody. Abdominal ultrasonography showed chronic liver parenchymal disease and gallbladder stones, but normal diameter of the common bile duct. Further magnetic resonance cholangiopancreatography showed a normal common bile duct (Figure 1 B).
|
|
|
Figure 1. (A) The patient had Raynaud’s phenomenon and digital pitting scar (white arrow). (B) The magnetic resonance cholangiopancreatography image shows gallstones (white arrow) with intact biliary duct. (C) The brain computed tomography images show a hypodense area in the occipital lobe, which is a characteristic of posterior reversible encephalopathy syndrome (white arrow). |
After 4 days of supportive care, the patient’s jaundice worsened (total bilirubin, 13.2 mg/dL) with coagulopathy (prothrombin time, 13.9 seconds). At this time, the patient experienced sudden altered mental status with seizure, vision loss, and elevated blood pressure (180/77 mmHg). She was diagnosed with acute liver failure and hypertensive crisis. Brain CT showed faint low density in the bilateral occipital lobes and posterior parietal lobes with edematous change that was diagnosed as RPLS (Figure 1 C).
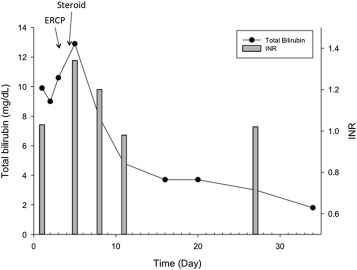
An aggressive control of blood pressure was attempted with nifedipine plus 5 mg amlodipine/80 mg valsartan QD. Liver biopsy was not possible because of coagulopathy; however, a 100-mg intravenous hydrocortisone injection was administered every 12 hours because of concern of impending autoimmune acute liver failure. Fortunately, her clinical condition, including consciousness level, vision loss, and kidney and liver function, considerably improved after 2 days (Figure 2 ). Following 2 weeks of 100 mg intravenous hydrocortisone therapy, we tapered the steroid dose to 10 mg oral prednisolone twice daily. The patient became asymptomatic with normal liver function, and her status was maintained with 4 mg/d methylprednisolone. After follow-up for 9 months, her liver function test results were within the normal range.
|
|
|
Figure 2. Level of total bilirubin (mg/dL) and international normalized ratio over the course of treatment with endoscopic retrograde cholangiopancreatography and steroid intervention. |
Discussion
Reports describe an association between autoimmune hepatitis and SS; therefore, elevation of liver enzyme levels should be monitored [2] . Our patient had acute hepatitis with severe jaundice, coagulopathy, and acute conscious change due to RPLS, a condition that mimicked sudden onset acute liver failure, but not hepatic encephalopathy because she had no preexisting liver disease, and the abdominal CT scan showed no liver cirrhosis. The most frequent symptoms of RPLS include headache, seizures, and visual changes.
The etiology of RPLS is thought to be failure of cerebral autoregulation in severe hypertension along with possible additive injury secondary to uremia, cytotoxic drug use, and microthrombi formation [7] . It may be associated with certain autoimmune disorders, including autoimmune hepatitis and rheumatic diseases under immunosuppressant treatment, and with chemotherapy treatment [6] . However, the mechanism by which immunosuppressive therapy might cause RPLS is unclear. Hypertensive encephalopathy is a feature in the majority of RPLS patients; treatments for hypertension are thought to resolve RPLS [3] ; [8] .
It is difficult initially to identify the causes of acute liver injury. We excluded viral hepatitis, alcohol- or drug-related hepatitis, and congestive heart failure-related hepatitis by initial evaluation. Using the revised Original Scoring System of the International Autoimmune Hepatitis Group, the patients posttreatment aggregate score was 17, which strongly suggested autoimmune hepatitis [9] . Steroid treatment is controversial in acute liver failure. However, this patient had a good response to steroid treatment. Although connective tissue-related autoimmune hepatitis has rarely been described, it was thought to be a liver manifestation associated with SS [10] .
In conclusion, we suggest that the cause of RPLS might be the use of immunosuppressants because of SS and autoimmune hepatitis. The reversible nature of RPLS makes the diagnosis important. Adequate treatment of hypertension and autoimmune hepatitis is necessary. Further studies are required establish treatment guidelines. It is worthwhile for young residents to keep this in mind when doing emergent treatment.
Conflict of interest
All authors declare no conflicts of interest.
References
- [1] A. Gabrielli, E.V. Avvedimento, T. Krieg; Scleroderma; N Engl J Med, 360 (2009), pp. 1989–2003
- [2] C.E. Rodrigues, C.L. Borges, J.F. de Carvalho; Diffuse systemic sclerosis and autoimmune hepatitis: a unique association; Clin Rheumatol, 29 (2010), pp. 799–801
- [3] J. Hinchey, C. Chaves, B. Appignani, J. Breen, L. Pao, A. Wang, et al.; A reversible posterior leukoencephalopathy syndrome; N Engl J Med, 334 (1996), pp. 494–500
- [4] J.E. Fugate, D.O. Claassen, H.J. Cloft, D.F. Kallmes, O.S. Kozak, A.A. Rabinstein; Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings; Mayo Clin Proc, 85 (2010), pp. 427–432
- [5] W.S. Bartynski; Posterior reversible encephalopathy syndrome: Part 1. Fundamental imaging and clinical features; AJNR Am J Neuroradiol, 29 (2008), pp. 1036–1042
- [6] A. Dhillon, C. Velazquez, C. Siva; Rheumatologic diseases and posterior reversible encephalopathy syndrome: two case reports and review of the literature; Rheumatol Int, 32 (2012), pp. 3707–3713
- [7] W.S. Bartynski; Posterior reversible encephalopathy syndrome: Part 2. Controversies surrounding pathophysiology of vasogenic edema; AJNR Am J Neuroradiol, 29 (2008), pp. 1043–1049
- [8] P.F. Yong, S.M. Hamour, A. Burns; Reversible posterior leukoencephalopathy in a patient with systemic sclerosis/systemic lupus erythematosus overlap syndrome; Nephrol Dial Transplant, 18 (2003), pp. 2660–2662
- [9] M.P. Manns, A.J. Czaja, J.D. Gorham, E.L. Krawitt, G. Mieli-Vergani, D. Vergani, et al.; Diagnosis and management of autoimmune hepatitis; Hepatology, 51 (2010), pp. 2193–2213
- [10] I. Marie, H. Levesque, J.L. Tranvouez, A. Francois, G. Riachi, N. Cailleux, et al.; Autoimmune hepatitis and systemic sclerosis: a new overlap syndrome?; Rheumatology (Oxford), 40 (2001), pp. 102–106