Summary
Riedels thyroiditis is a rare type of chronic thyroiditis, associated with fibroinflammatory process and invasion into surrounding tissues, leading to compressive symptoms. A 45-year-old man had a left thyroid mass, presenting with hypotension and bradycardia many times. He was diagnosed with vasovagal reflex caused by cervical vessel compression due to a thyroid lesion. We performed the emergency operation, and most of the left thyroid was removed to relieve the compression on cervical vessels. The result of pathology proved to be Riedels thyroiditis. The vasovagal reflex did not occur any more during the 28-month follow up, except on the 3rd day after the surgery. Six months after the thyroidectomy, the patient was found to have retroperitoneal fibrosis, diagnosed by biopsy during a laparotomy for biliary disease. Riedels thyroiditis can lead to a vasovagal episode and might not be a primary thyroid disease but rather a manifestation of the systemic disorder, multifocal fibrosclerosis.
Keywords
Riedels thyroiditis;vasovagal reflex;diagnosis
1. Introduction
Riedels thyroiditis (RT), also termed ligneous thyroiditis, chronic fibrous thyroiditis, or woody thyroiditis,1 ; 2 was first described by Bernhard Riedel in 1896.3 Riedels thyroiditis is a rare thyroid disease, which is found in 0.06% of all thyroidectomies.4 An autoimmune mechanism is considered to have a role in the pathogenesis of Riedels thyroiditis.5 Clinically, Riedels thyroiditis often leads to compressive symptoms, including dyspnea and dysphagia.6 We herein present a rare case of Riedels thyroiditis that caused repeated episodes of vasovagal reflex.
2. Case report
A 45-year-old male presented with a left cervical mass and tachycardia and was diagnosed with toxic nodular goiter associated with hyperthyroidism. After treatment with thiamazole for 1 month, the patient had an elevated thyroid stimulating hormone (TSH) level (24.62μ IU/ml [normal range: <5.5 μIU/ml]), and he was given thyroxine tablets. The TSH was restored to the normal level (4.75 μIU/ml). During this period, the patient presented twice with episodes of headache, chest distress, and tinnitus. These symptoms could be relieved if the patient bowed his head and bended from the waist for about 1 hour. He was admitted to hospital for his third episode at night. During these episodes, his consciousness was always normal and there was no syncope. He had no history of diabetes mellitus or epilepsy.
Physical examination showed that consciousness of the patient was clear. A mass about 6 cm × 5 cm was palpated in the left part of the neck. The mass was hard, nontender, and had no clear margin. The cardiac border was normal. Heart sounds were strong and regular without pathological murmurs. Blood glucose was normal. Cardiac troponin and D-dimer were negative. The echocardiogram showed that the structure of heart was normal. The serum levels of T3, T4, and TSH were normal. Both antithyroperoxidase (anti-TPOAb) and antithyroglobulin (anti-TgAb) were negative. The ultrasound scan of neck showed a 5-cm solid mass with cyst component in the left lobe of the thyroid. Left internal jugular vein and common carotid artery were deformed by compression. Computerized tomography (CT) scan suggested that a mass in the left lobe of the thyroid push the trachea to the right. The carotid artery was not clearly shown. There were no enlarged lymph nodes in the neck area (Fig. 1).
|
|
|
Figure 1. A mass lesion in the left thyroid lobe invaded the carotid artery (black arrow), and slight tracheal compression (asterisk) was observed. |
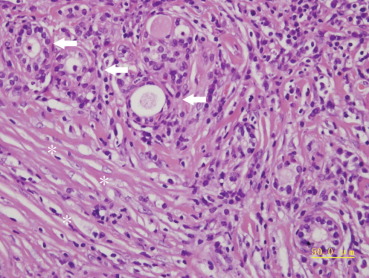
After admission, the patient had multiple episodes of the abovementioned symptoms. The electrocardiogram (ECG) demonstrated sinus bradycardia with a heart rate (HR) of 35-40/min and appearing escape rhythm of junction zone. The blood pressure (BP) dropped to about 60/40 mmHg. The symptoms were relieved 3–5 min after intravenous injection of atropine or dopamine. The HR and BP gradually restored to the normal level. A temporary heart pacemaker was installed and set 55-60/min as the pacing frequency. However, the patient still had recurrent attacks. Angiography showed no coronary artery stenosis or spasm, but the episode interval became shorter and shorter. After multidisciplinary discussion, the cause of the disease was considered to be the vasovagal reflex by compression of left thyroid mass. An emergency operation was performed on the 3rd day after admission. During the surgery, the right thyroid was found firm but with no definite nodule, and the isthmus and left side were enlarged and firm, which had no clear margin and was adhesive to infrahyoid musculature anteriorly and to recurrent laryngeal nerve interiorly. A hard mass of 6 cm × 4 cm × 4 cm was seen in the enlarged left thyroid, which entrapped the carotid vascular sheath upward to the bi-furcation of the carotid artery, making dissection very difficult. After isthmectomy was performed, the mass was cut open to carotid vascular sheath. Most of the mass and left thyroid were removed. Part of the mass behind the carotid vessels and surrounding recurrent laryngeal nerve was left owing to the difficulty of dissection. The pathology showed (Fig. 2) noticeable fibroplasias, with lymphocytes and plasmocytes infiltrating. Thyroid follicular epithelial cells were separated by the fibrous tissue. In the immunohistochemical study, some thyroid follicular cells showed CK19 (+), α-actin (+), and vimentin (+). The diagnosis was considered to be Riedels thyroiditis. On postoperative Day 4, the vasovagal reflex occurred again. However, the severity was considerably less, and the duration was very short (20 minutes). One week after the operation, an IgG test was done. The serum IgG value was 1950 mg/dL, (normal range: 751–1560 mg/dL) and higher than normal value. However, the IgA and IgM levels remained normal. The patient was discharged after a 12-day hospitalization and continued to use levothyroxine 50 μg/d.
|
|
|
Figure 2. Thyroid residual follicles (arrows) were disorganized by fibro-inflammatory process (asterisks) (hematoxylin & eosin stain, original magnification 40×). |
Six months later, the patient was admitted to hospital again because of acute cholecystitis and gallbladder stones. During laparoscopic cholecystectomy, we found a hard mass located in the duodenohepatic ligament. The mass entrapped the hepatic artery, portal vein, and common bile duct, and therefore it was difficult to excise. Excised gallbladder and small tissue from the mass were taken for frozen and paraffin section diagnoses, and diffuse fibrosis and lymphocytes and plasmocytes infiltration were observed. Biliary tract exploration and cholangiography were performed, but no abnormality was found. Therefore, the T-tube was placed to drain the biliary tract. Postoperative recovery of the patient was smooth. There was no episode of vasovagal reflex during the subsequent follow-up of 28 months. On the 2-year follow-up CT scan, the smaller size of the thyroid lesion and no compression were noted (Fig. 3).
|
|
|
Figure 3. The lesion in the left thyroid lobe became smaller (black arrow) 2 years after surgery. |
3. Discussion
Riedels thyroiditis is a rare form of chronic thyroiditis.4 The incidence has been reported to be 1.06 in for every 10,000 people. The average age of onset is 46.8 years, with the ratio of male to female being 1:5.6 Pathophysiology of the disease is still in controversy.7 It is suggested that Riedels thyroiditis originate from the fibrosis by autoimmune reaction. Fibrosis can extend beyond the capsule of thyroid and characteristically invades and encloses the adjacent structures in the neck extending beyond the capsule of thyroid. Riedels thyroiditis is also associated with other fibrous inflammatory processes, including retroperitoneal, parotid and mediastinal fibrosis, orbital pseudotumour, sclerosing cholangitis, and fibrosis in other organ systems.4; 5 ; 6 Approximately, one-third of Riedels thyroiditis cases are associated with clinical findings of multifocal fibrosclerosis at the time of diagnosis.2 This is a case of fibrosis of thyroid gland associated with retroperitoneal tissue fibrosis. The surgeon was not familiar with the disease process, and therefore, exploration of the common bile duct was performed. It has also been suggested that Riedels thyroiditis may not be a primary thyroid disease but rather a manifestation of the systemic disorder, multifocal fibrosclerosis.2 Most cases of multifocal fibrosclerosis have been proved to belong to IgG4-related sclerosis disease (IgG-RSD). Therefore, Riedels thyroiditis is considered as part of the IgG4-related sclerosis spectrum.8 ; 9 IgG-RSD is characterized by mass-forming lesions in various organs because of severe IgG4 positive lymphoplasmcytic infiltration and stromal fibrosis, and an increased serum IgG4 level can be found in IgG-RSD patients.9 The patient had Riedels thyroiditis and duodenohepatic ligament mass with increasing serum IgG. Pathologically, these lesions were similar: fibrotic change with lymphoplasmcytic infiltration. We considered the case as a possible IgG4-RSD, although IgG4 staining on plasma cell and the serum IgG4 test were not done.
Riedels thyroiditis is characteristic of the progressive fibrous replacement of the thyroid gland.7 Finally, the thyroid will become wood hard and less functional than normal. The lesion can invade and compress the cervical vessels, recurrent laryngeal nerve, trachea, and esophagus to give rise to hoarseness, dyspnea, and dysphagia,10 imposing difficulty on clinical differentiation from malignancy. However, vasovagal reflex caused by Riedels thyroiditis compressing the cervical vessel has never been reported. Vasovagal reflex is characterized by blood pressure decrease, with or without bradycardia and autonomic nerves excitation, leading to hypoperfusion of cerebral blood vessels and then vasovagal syncope.11 ; 12 According to features of its hemodynamics, vasovagal syncope can be divided into three types: Type I, mixed; Type II, cardioinhibitory; and Type III, vasodepressive.13 ; 14 Syncope caused by vasovagal reflex is rarely life-threatening, but frequent episodes of vasovagal reflex can affect life quality and even lead to severe accidents. This patient is in the prime of his life, and had paroxysmal bradycardia and hypotension. The consciousness of the patient was always clear without syncope episode. His symptoms can be relieved by administering atropine and dopamine but not by using pacemaker. After each episode, all abnormalities will restore to normal. The typical manifestations of vasovagal reflex are as mentioned above. Many causes can induce vasovagal reflex, including affection change, orthostatic stress, dysautonomia, and carotid sinus hypersensitivity.15 ; 16 In this case, cardiovascular system examination excluded the coronary heart disease, while a hard mass of left thyroid lobe without clear margins, showed notable compression of cervical vessels. Therefore, the episode of vasovagal reflex was considered to be related to a left thyroid lesion. Intraoperative frozen pathology showed a considerable number of infiltrating fibrous tissues in the thyroid gland. Hence, the thyroid mass was largely excised to relieve the compression of cervical vessels. The vasovagal reflex did not occur in the 28-month follow up. Glucocorticoids or tamoxifen can be used to treat Riedels thyroiditis. High-dose glucocorticoids can be considered as a primary treatment method for reducing the tissue edema and fibroplasias and relieving the compressive symptoms. However, long-term use is not recommended.2 Tamoxifen has also been proven to be effective for some patients resistant to glucocorticoids or prohibited to use them; the mechanism of action may be inhibiting fibroblastic proliferation to relieve symptoms.17 ; 18 Moreover, levothyroxine can also be considered to maintain function of thyroid when it is necessary.19 This patient recovered well and only required levothyroxine therapy.
Acknowledgments
This work was supported by the founding of Beijing municipal health system academic leaders of high-level health personnel program, No. 2011-2-28.
References
- 1 B. McIver, M.M. Fatourechi, I.D. Hay, V. Fatourechi; Graves' disease after unilateral Riedels thyroiditis; J Clin Endocrinol Metab, 95 (2010), pp. 2525–2526
- 2 K. Kakudo, Y. Li, M. Hirokawa, T. Ozaki; Diagnosis of Hashimotos thyroiditis and IgG4-related sclerosing disease; Pathol Int, 61 (2011), pp. 175–183
- 3 I. Pirola, M.L. Morassi, M. Braga, E. De Martino, E. Gandossi, C. Cappelli; A case of concurrent Riedels, Hashimotos and acute suppurative thyroiditis; Case Report Med, 2009 (2009), pp. 1–4
- 4 N. Shahi, M.F. Abdelhamid, M. Jindall, R.W. Awad; Riedels thyroiditis masquerading as anaplastic thyroid carcinoma: a case report; J Med Case Reports, 4 (2010), p. 15
- 5 R. Slman, H. Monpeyssen, S. Desarnaud, et al.; Ultrasound, elastography, and fluorodeoxyglucose positron emission tomography/computed tomography imaging in Riedels thyroiditis: report of two cases; Thyroid, 21 (2011), pp. 799–804
- 6 L. Lu, F. Gu, W.X. Dai, et al.; Clinical and pathological features of Riedels thyroiditis; Chin Med Sci J, 25 (2010), pp. 129–134
- 7 S. Fontaine, F. Gaches, L. Lamant, M. Uzan, A. Bennet, P. Caron; An unusual form of Riedels thyroiditis: a case report and review of the literature; Thyroid, 15 (2005), pp. 85–88
- 8 M. Dahlgren, A. Khosroshahi, G.P. Nielsen, V. Deshpande, J.H. Stone; Riedels thyroiditis and multifocal fibrosclerosis are part of the IgG4-related systemic disease spectrum; Arthritis Care Res (Hoboken), 62 (2010), pp. 1312–1318
- 9 L. Zhang, T.C. Smyrk; Autoimmune pancreatitis and IgG4-related systemic diseases; Int J Clin Exp Pathol, 3 (2010), pp. 491–504
- 10 P. Lee, A. Vonk-Noordegraaf, M.A. Paul, T.G. Sutedja; Unusual manifestation of Riedels thyroiditis; Ann Thorac Surg, 84 (2007), p. 300
- 11 M.A. Aydin, T.V. Salukhe, I. Wilke, S. Willems; Management and therapy of vasovagal syncope: a review; World J Cardiol, 2 (2010), pp. 308–315
- 12 P. Alboni; Therapy of vasovagal syncope: to prevent the vasovagal reflex or to treat the impending reflex?; Europace, 12 (2010), pp. 776–778
- 13 J. Gajek, D. Zysko, W. Mazurek; Efficacy of tilt training in patients with vasovagal syncope; Kardiol Pol, 64 (2006), pp. 602–608
- 14 D. Zysko, J. Gajek, E. Kozluk, A.K. Agrawal, J. Smereka, I. Checinski; Clinical relevance of syncope and presyncope induced by tilt testing; Acta Cardiol, 64 (2009), pp. 461–465
- 15 W. Wieling, R.D. Thijs, N. van Dijk, A.A. Wilde, D.G. Benditt, J.G. van Dijk; Symptoms and signs of syncope: a review of the link between physiology and clinical clues; Brain, 132 (Pt 10) (2009), pp. 2630–2642
- 16 P. Mitro, P. Kirsch, G. Valocik, P. Murin; A prospective study of the standardized diagnostic evaluation of syncope; Europace, 13 (2011), pp. 566–571
- 17 Y.J. Jung, C.R. Schaub, R. Rhodes, F.A. Rich, S.J. Muehlenbein; A case of Riedels thyroiditis treated with tamoxifen: another successful outcome; Endocr Pract, 10 (2004), pp. 483–486
- 18 K. Pritchyk, K. Newkirk, P. Garlich, Z. Deeb; Tamoxifen therapy for Riedels thyroiditis; Laryngoscope, 114 (2004), pp. 1758–1760
- 19 N. Dabelic, T. Jukic, Z. Labar, S.A. Novosel, N. Matesa, Z. Kusic; Riedels thyroiditis treated with tamoxifen; Croat Med J, 44 (2003), pp. 239–241
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?