Summary
Background/Objective
Chronic anal fissure is a painful condition that is associated with an increase in internal anal sphincter pressure. The main aim of this study is to evaluate the efficacy and adverse effects of topical isosorbide 5 mononitrate and topical diltiazem, when administered either as single agents or in combination, in the treatment of anal fissure.
Methods
Patients with chronic anal fissure were enrolled in the study. They were randomized into three groups: Group A (0.2% isosorbide 5 mononitrate users), Group B (2% diltiazem users), and Group C (2%diltiazem + 0.2% isosorbide 5 mononitrate users). Pain was evaluated using a visual analog scale (VAS). Level of strain during defecation was graded on a 4-point scale.
Results
A total of 55 patients were enrolled in the study. The average ages of patients in Groups A, B, and C were 37.94 ± 16.19, 42.83 ± 13.21, 40 ± 13.58 years, respectively. After treatment, pain completely abated in 55.6% of patients in Group A, 27.8% (n = 5) in Group B, and 42.1% (n = 8) in Group C. The decreases in average VAS values prior to and after treatment in Groups A, B, and C were statistically significant (p values 0.0001, 0.001, and 0.0001, respectively). Average strain scores prior to and after treatment were 2.11/0.72 for Group A, 2.17/0.94 for Group B, and 1.95/0.47 for Group C. Strain during defecation prior to and after treatment in Groups A, B, and C was statistically significant (p values 0.001, 0.001, and 0.003, respectively).
Conclusion
Topical diltiazem and a combination of nitrate and diltiazem can be used in the treatment of anal fissure. However, the agents are not significantly superior each other.
Keywords
anal fissure;diltiazem;isosorbide mononitrate
1. Introduction
Chronic anal fissure is a painful condition that is associated with an increase in internal anal sphincter pressure. The aim of fissure treatment is to increase mucosal blood flow by reducing or eliminating the spasm in the anal sphincter and improve the fissure symptoms.1 ; 2 Anal fissure can be healed by a wide range of treatments, including medical (topical or oral) and surgical treatments. These treatment methods increase local blood supply and help heal the fissure by reducing hypertony. In the treatment of fissure, surgical or chemical sphincterotomy is performed.3 ; 4 Many studies have proved the efficacy of various chemical agents in reducing anal sphincter pressure, and many topical and systemic agents have been used for this purpose.2; 3 ; 4 In many studies, nitrates and calcium channel blockers have been used in the treatment of anal fissure. Some studies have shown that increased nitrate concentrations result in increased improvement ratios. Some studies have shown that headache, which is the most important adverse effect of nitrates, increases with an increase in the dose. The success ratios of topical calcium blockers have been found to be equivalent to those of nitrates.5 The goal of this study is to evaluate the efficacy and adverse effects of topical isosorbide 5 mononitrate and topical diltiazem when administered as single agents or in combination.
2. Material and methods
Patients with chronic anal fissure presenting to the General Surgery Clinic of Keçiören Training and Research Hospital between December 2010 and April 2011 were enrolled in the study. Informed consent was obtained from all patients. Rectoscopic examination was performed on all patients to exclude other pathologies. The inclusion criteria for this study were as follows: (1) patients had been experiencing chronic anal fissure symptoms for more than 2 months; (2) the classic triad of hypertrophied anal papilla, sentinel skin tag, and exposed internal sphincter muscle fibers was present; (3) prior to the use of topical nitroglycerin (NTG) and diltiazem, all patients were treated with a conservative regimen of bulk agents and warm sitz baths for 6 weeks. Exclusion criteria for the study included complicated Grade III–IV hemorrhoidal disease, pregnancy, puerperal period, systemic diseases interfering with wound healing (chronic obstructive lung disease (COPD), diabetes mellitus (DM), congestive cardiac failure (CCF), collagen tissue disease, etc.), and inflammatory intestinal disease.
Patients were randomized into three groups: Group A (n = 18; 0.2% isosorbide 5 mononitrate users), Group B (n = 18; 2% diltiazem users), and Group C (n = 19; 2% diltiazem + 0.1% isosorbide 5 mononitrate users). Ages, genders, physical examination and rectoscopy results, symptoms prior to and after treatment (pain, straining during defecation), whether or not fissure improved after treatment, and complications caused by treatment were recorded. Patients in Group A were asked to apply 0.2% isosorbide 5 mononitrate (a pea- or chickpea-sized amount; approximately 1 g) twice daily to the anodermal area for a period of 8 weeks. Patients in Group B were asked to apply a 2% diltiazem pomade and those in Group C to apply a pomade containing 2% diltiazem and 0.1% isosorbide 5 mononitrate to the anus, twice daily for 8 weeks in both cases. Patients in each group were advised to consume fiber-rich and high-water-content diet. No other medicines were given to the patients. All patients were contacted 1 week after the initiation of treatment for assessment of complications (headache, perianal irritation, hypotension, incontinence, pain, bleeding, etc.). At the end of the 8-week treatment, patients were evaluated with respect to physical examination results, symptoms, and complications. Pain was evaluated using a visual analog scale (VAS). Patients were asked to score the pain prior to and after 8 weeks of treatment. In a VAS a 10-cm-long straight line, called a visual evaluation scale, is used for ranking pain intensity. On this straight line, “0” represents absence of pain and “10” represents unbearable pain. Changes in pain intensities in the patients of three groups during the period between prior to and after treatment were recorded on a VAS and compared. Level of strain during defecation was graded on a four-point scale: serious strain was scored as 3, moderate strain as 2, mild strain as 1, and defecation without strain as 0. Patients of all the groups were asked to specify their level of strain during defecation prior to and after treatment.
Statistical evaluation was performed by Biostatistics Department using SPSS 18 for Windows software. Unidirectional analysis of variance (ANOVA) and chi-square (χ2) test were used for evaluating the age and gender distributions, respectively. As the number of study participants was less, the Fisher exact chi-square test was used for the evaluation of improvement in fissure and its complications. To evaluate the difference in patients pain and strain scores prior to and after treatment between the groups, nonparametric Kruskal–Wallis variance analysis was used. Wilcoxon test was used for the evaluation of the differences in pain and strain scores prior to and after treatment within each group. A p value of <0.05 was considered statistically significant.
3. Results
At the beginning of the study, 60 patients with chronic anal fissure were enrolled. However, during the study one patient discontinued treatment and four patients failed to turn up for checkups, and they were excluded from the study. The study continued with a total of 55 patients (18 patients each in Groups A and B, and 19 patients in Group C). The average ages of patients in Groups A, B, and C were 37.94 ± 16.19, 42.83 ± 13.21, and 40 ± 13.58 years, respectively. There were no statistically significant differences between the groups with respect to age and gender (p = 0.865 and p = 0.858, respectively) ( Table 1).
| Group | No. patients | Mean age (y) | ATD | AKD | AHD |
|---|---|---|---|---|---|
| A | 18 | 37.94 ± 16.19 | 55.6% (10) | 22.2% (4) | 22.2% (4) |
| B | 18 | 42.83 ± 13.21 | 27.8% (5) | 44.4% (8) | 27.8% (5) |
| C | 19 | 40 ± 13.58 | 42.1% (8) | 36.8% (7) | 21.1% (4) |
| p | 0.865 | 0.0858 |
AHD = less than 50% reduction in pain or no difference; AKD = More than 50% reduction in pain; ATD = disappearance of pain.
Pain abated completely in 55.6% of patients (n = 10) in Group A, 27.8% (n = 5) in Group B, and 42.1% (n = 8) in Group C; greater than 50% reduction in pain was observed in 22.2% of patients (n = 4) in Group A, 44.4% (n = 8) in Group B, and 36.8% (n = 7) in Group C; and no change or less than 50% reduction in pain was observed in 22.2% of patients (n = 4) in Group A, 27.8% (n = 5) in Group B, and 21.1% (n = 4) in Group C after treatment ( Table 1). The average pain scores prior to/after treatment were found to be 6.5/1.67 in Group A, 8.11/3.22 in Group B, and 7/1.89 in Group C. Accordingly, the reduction of the VAS average value within each group in the period between prior to and after treatment was found to be statistically significant. The p values in Groups A, B, and C were found to be 0.0001, 0.001, and 0.0001, respectively. When the change in the VAS values prior to and after treatment for the three groups were compared, no statistically significant differences were found between them (p = 0.957) ( Table 2 ; Table 3).
| Group | BT VAS | AT VAS | p | BT DSS | AT DSS | p |
|---|---|---|---|---|---|---|
| A | 6.5 | 1.67 | 0.0001 | 2.11 | 0.72 | 0.001 |
| B | 8.11 | 3.22 | 0.001 | 2.17 | 0.94 | 0.001 |
| C | 7 | 1.89 | 0.0001 | 1.95 | 0.47 | 0.003 |
AT = after treatment; BT = before treatment; DSS = defecation strain score; VAS = visual analog scale.
| Group | VAS BATD | DSS BATD |
|---|---|---|
| A | 4.83 ± 2.95 | 1.38 ± 1.14 |
| B | 4.88 ± 3.19 | 1.22 ± 0.94 |
| C | 5.10 ± 3.03 | 1.22 ± 1.11 |
| p | 0.957 | 0.888 |
BATD = difference between prior to and after treatment, DSS = defecation strain score; VAS = visual analog scale.
Average strain scores prior to and after treatment were evaluated to be 2.11/0.72 for Group A, 2.17/0.94 for Group B, and 1.95/0.47 for Group C. For each group, the reduction in strain score during defecation in the period between prior to and after treatment was found to be statistically significant. The p values for Groups A, B, and C were 0.001, 0.001, and 0.003, respectively. The differences in strain scores during defecation prior to and after treatment for the groups, were not statistically significant (p = 0.888) ( Table 2 ; Table 3).
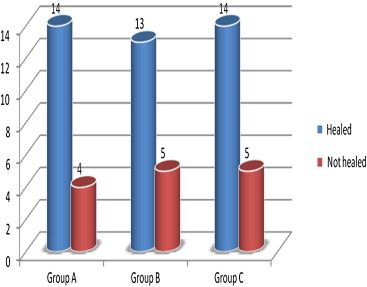
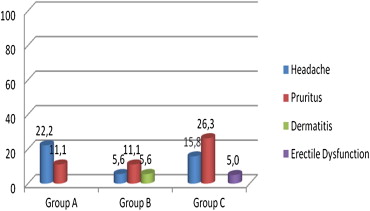
No significant difference was found between the groups with respect to the improvement in physical examination results (p = 0.990). The improvement ratios for all three groups were found to be similar. In 77.8% of the patients (n = 14) in Group A, 72.2% (n = 13) in Group B, and 73.7% (n = 14) in Group C, fissure was observed to have improved ( Fig. 1). The most common complications encountered in all three groups were headache and itchiness (Fig. 2); headache was observed in eight patients (4 in Group A, 1 in Group B, and 3 in Group C) and itchiness in nine patients (2 in Group A, 2 in Group B, and 5 in Group). For headache and itchiness, there were no statistically significant differences between the groups (p = 0.359 and p = 0.350, respectively). Perianal dermatitis was observed in one patient in Group B and erectile dysfunction in one patient in Group C. Gas or stool incontinence was not seen in any of the patients ( Table 2).
|
|
|
Figure 1. Improvement ratios between groups. |
|
|
|
Figure 2. Distribution of complication ratios between groups (%). |
4. Discussion
In this study, we determined that topical nitrate and topical diltiazem separately, and their combination all are efficacious in the treatment of chronic anal fissure. Additionally, when we compared the three groups that used these three treatments, none of them were found to be superior to others with respect to VAS score, strain during defecation score, and improvement of fissure. We observed that the most common adverse events in each of the three groups were headache and itchiness.
Anal fissure develops in approximately 10–15% of the patients presenting with proctologic discomfort. The most common symptoms are pain and rectal bleeding.2 It is known that anal sphincter spasm and the ischemia developing after spasm lead to chronic anal spasm. The aim of chronic anal fissure treatment is to remove ischemia by reducing spasm. Various surgical and medical treatments have been tried for healing anal fissure.1; 4 ; 5 Chemical sphincterotomy have been suggested as an alternative to surgery to avoid possible complications of surgical treatment. Among these, nitrates, calcium channel blockers, and botulinum toxin are the most studied and used agents.2; 3 ; 5
Nitroglycerin contributes to anodermal blood flow by reducing anal sphincter pressure. Transdermal absorption of nitrates is through passive diffusion, and varies depending on people and the site of administration. Hence, it is difficult to standardize the administration of this medicine.3 In a prospective study by Lund et al6 where it was compared with placebo, improvement ratios were found to be 68% for glycerol trinitrate (GTN) and 8% for placebo. Similar improvement ratios have been reported in other studies.2 ; 3 Despite initial efficacy, its long-term results and effect on disease recurrence are still under discussion.7 Other organic nitrates that are used in the treatment of anal fissure include isosorbide dinitrate and isosorbide mononitrate. Their efficacies have been observed to be similar to that of GTN.8; 9 ; 10 We also used isosorbide 5 mononitrate in our study. In 14 (77.8%) of the 18 patients with chronic anal fissure who used the pomade prepared with 0.2% isosorbide mononitrate, improvement of anal fissure and significant reduction in pain (no pain in 55.6% and more than 50% reduction in 22.2%) were observed. While this finding was similar to the findings of other publications in the literature, it was a little above average. This might be due to a lack of long-term follow-up of patients and the small size of the sample.
In this study, where calcium antagonists were administered for the first time, sublingual niphedipine was observed to reduce anal channel rest pressure in healthy individuals and patients with anal fissure.11 In studies with topical diltiazem providing improvement in 50% of the GTN treatment resistance cases is available.4; 12; 13 ; 14 This could be due to its tolerance being higher than and mechanism of action being different from those of nitrates.10 ; 11 In our study, we used 2% diltiazem. Consistent with the findings of topical diltiazem studies in literature, we observed an improvement in the fissure and a significant reduction in pain in 13 (72.2%) of the 18 patients (no pain in 27.8% and more than 50% reduction in 44.4%).
In a study conducted on internal anal sphincter isolated from a sheep, the administration of a combination of GTN and diltiazem was observed to be more efficacious than the administration of other pharmacological agents as single agents.15 In our study, we used a mixture consisting of 2% diltiazem and 0.1% isosorbide 5 mononitrate in Group C; however, the efficacy of this combination was seen to be similar to the single agents used in other two groups. In 14 (73.7%) of the 19 patients, improvement in the fissure and a significant reduction in pain were observed compared to other two groups (no pain in 42.1% and more than 50% reduction in 36.8%).
Strain during defecation was also evaluated as an indicator of the patients quality of life and time spent in bathroom. This scoring had only been used in the study by Takoot and Salaam, where the patients were categorized into three groups. The first group used GTN, the second group lidocaine, and the third group a healer cream (mixture of isosorbide dinitrate, lidocaine, and rutoside). In all three groups, a reduction in straining after the treatment was observed.16 Our study results were found to be consistent with those of other studies in the literature. In all three groups, a significant reduction in straining and discomfort was observed after treatment compared to those prior to treatment.
Headache is one of the most important adverse events of nitrate treatment, and it has been reported to occur in up to 50% of patients. Headache frequently responds to simple analgesics. Usually, it is mild and in less than 10% of patients it necessitates discontinuation of treatment.1; 2; 3; 4; 8 ; 17 There are publications reporting a positive correlation between nitrate dose and headache.1; 3 ; 18 In this study, headache ratios for Groups A, B, and C were 22.2%, 5.6%, and 15.8%, respectively. While it was not statistically significant, there were fewer occurrences of headache in the patient group using diltiazem. A literature search reveals that nitrates causes significantly fewer or no headaches compared to diltiazem.2; 4 ; 19 The reason why it was statistically not significant might be the low number of study participants. We aimed to reduce the adverse events associated with nitrate by combining it with diltiazem and providing synergistic efficacies similar or superior to those of a single agent. When patients in Group C were compared with those in Group A we did not find a statistically meaningful difference with respect to adverse events and treatment efficacy. However, in another center, we had a patient using the pomade consisting of 2% diltiazem and 0.1% isosorbide 5 mononitrate, who was prescribed a commercially available form containing 0.4% GTN and discontinued treatment on the 3rd day due to headache. Studies with bigger study groups will clearly reveal whether there is a difference between these agents in terms of adverse events and treatment efficacy.
In our study, itchiness, however, was recorded as another important symptom noticed in the 1st week of treatment. Itchiness ratio observed in Groups A, B, C were 11.1%, 11.1%, and 26.3%, respectively. There were no statistically significant differences between the three groups; however, in Group C the itchiness ratio was higher. In general, these ratios were higher compared to those reported in literature.20 ; 21 Dermatitis was seen in one Group B patient. Treatment was halted for 3–4 days. The patient was applying a dose higher than the dose in anamnesis and was spreading the medicine to the surrounding tissue. The correct method of use was explained to the patient and the treatment was continued. Dermatitis was not seen again. Erectile dysfunction was seen in one Group C patient. The patient wanted to discontinue treatment and hence was withdrawn from the study. In literature, there is no information on erectile dysfunction as an adverse effect.
A limiting factor of our study could be the lack of a control group. However, since all patients who were enrolled in the study had previously been treated unsuccessfully for anal fissure with various treatments, we found the use of a control group unnecessary.
In conclusion, topical nitrate, topical diltiazem, and their mixture can be used in the treatment of anal fissure. With respect to treatment success, none of these is statistically significantly superior to others.
References
- 1 S. Dhawan, S. Chopra; Nonsurgical approaches for the treatment of anal fissures; Am J Gastroenterol, 102 (2007), pp. 1312–1321
- 2 E.E. Collins, J.N. Lund; A review of chronic anal fissure management; Tech Coloproctol, 11 (2007), pp. 209–223
- 3 A.G. Acheson, J.H. Scholefield; Anal fissure: the changing management of a surgical condition; Langenbecks Arch Surg, 390 (2005), pp. 1–7
- 4 R. Nelson; Non surgical therapy for anal fissure; Cochrane Database Syst Rev, 4 (2006) CD003431
- 5 A. Poh, K.Y. Tan, F. Seow-Choen; Innovations in chronic anal fissure treatment: a systematic review; World J Gastrointest Surg, 2 (2010), pp. 231–241
- 6 J.N. Lund, P.O. Nystrom, G. Coremans, et al.; An evidence-based treatment algorithm for anal fissure; Tech Coloproctol, 10 (2006), pp. 177–180
- 7 A. Graziano, L. Svidler Lopez, S. Lencinas, et al.; Long-term results of topical nitroglycerin in the treatment of chronic anal fissures are disappointing; Tech Coloproctol, 5 (2001), pp. 143–147
- 8 R. Nelson; A systematic review of medical therapy for anal fissure; Dis Colon Rectum, 47 (2004), pp. 422–431
- 9 L. Tankova, K. Yoncheva, D. Kovatchki, et al.; Topical anal fissure treatment: placebo-controlled study of mononitrate and trinitrate therapies; Int J Colorectal Dis, 24 (2009), pp. 461–464
- 10 L. Tankova, K. Yoncheva, M. Muhtarov, et al.; Topical mononitrate treatment in patients with anal fissure; Aliment Pharmacol Ther, 16 (2002), pp. 101–103
- 11 E. Chrysos, E. Xynos, G. Tzovaras, et al.; Effect of nifedipine on rectoanal motility; Dis Colon Rectum, 39 (1996), pp. 212–216
- 12 K. McCallion, K.R. Gardiner; Progress in the understanding and treatment of chronic anal fissure; Postgrad Med J, 77 (2001), pp. 753–758
- 13 D.F. Altomare, G.A. Binda, S. Canuti, et al.; The management of patients with primary chronic anal fissure: a position paper; Tech Coloproctol, 15 (2011), pp. 135–141
- 14 U.K. Shrivastava, B.K. Jain, P. Kumar, et al.; A comparison of the effects of diltiazem and glyceryl trinitrate ointment in the treatment of chronic anal fissure: a randomized clinical trial; Surg Today, 37 (2007), pp. 482–485
- 15 M. Jonas-Obichere, J.H. Scholefield, A. Acheson, et al.; Comparison of the effects of nitric oxide donors and calcium channel blockers on the intrinsic myogenic tone of sheep isolated internal anal sphincter; Br J Surg, 92 (2005), pp. 1263–1269
- 16 M. Yakoot, M. Abdel Salaam; Study of efficacy and safety of a new local cream ('healer') in the treatment of chronic anal fissure: a prospective, randomized, single-blind, comparative study; Arq Gastroenterol, 46 (2009), pp. 179–182
- 17 A.A. Yantunde, S.A. Debrah; Current concepts in anal fissures; World J Surg, 30 (2006), pp. 2246–2260
- 18 H.R. Bailey, D.E. Beck, R.P. Billingham, et al.; A study to determine the nitroglycerin ointment dose and dosing interval that best promote the healing of chronic anal fissures; Dis Colon Rectum, 45 (2002), pp. 1192–1199
- 19 J.J. Puche, M.J. Garcia-Coret, F.L. Villalba, et al.; Local treatment of a chronic anal fissure with diltiazem vs. nitroglycerin. A comparative study; Cir Esp, 87 (2010), pp. 224–230
- 20 H.M. Kocher, M. Steward, A.J. Leather, et al.; Randomized clinical trial assessing the side-effects of glyceryl trinitrate and diltiazem hydrochloride in the treatment of chronic anal fissure; Br J Surg, 89 (2002), pp. 413–417
- 21 C. Placer, J.L. Elosegui, I. Irureta, et al.; Initial response to topical diltiazem can predict outcome of chronic anal fissure; Cir Esp, 82 (2007), pp. 16–20
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?