Keywords
Acute coronary syndrome;STEMI;PCI;Abciximab;Ticagrelor;Acute and spontaneous occlusion of LAD
Dear Editor,
The most frequent physiopathological substrate of ST-segment elevation myocardial infarction (STEMI) is total occlusion of an epicardial coronary artery due to an occlusive thrombus underlying an atherosclerotic plaque [1]. Rapid and complete coronary blood flow restoration is the mechanism underlying the benefit of reperfusion therapy in patients with STEMI. Percutaneous coronary intervention (PCI) restores a TIMI grade flow 3 in > 90% of patients [2]. However, STEMI patients have a high risk of intraprocedural thrombotic events (IPTEs) because of elevated thrombotic burden and prothrombotic milieu during the ischemic event [3]. IPTEs occur more frequently in patients with STEMI than in those with unstable angina or non-STEMI and are associated with mortality, bleeding and major adverse cardiac events (MACE) [4].
Distal embolization, slow flow or no reflow and abrupt artery closure are the most common complications during PCI for STEMI. Such complications tend to be life-threatening and to strongly increase the total catheter-related mortality [4]; [5] ; [6]. The occurrence of IPTEs is strongly associated with a lower frequency of TIMI grade flow 3 at the end of the procedure and greatly adds to the procedure. Although the angiographic presence of thrombus has been independently correlated to IPTEs, the routinely use of aspiration thrombectomy is not associated with a reduction of their incidence. Despite the introduction of novel antiplatelet and antithrombotic therapies, the occurrence of IPTEs during primary stenting for STEMI is currently common (~ 1 in 8 patients).
An 81-year old woman was referred to our emergency department for antero-lateral STEMI. Hypertension pharmacologically treated and no previous hospitalizations for cardiac problems. At admission, her blood pressure was 120/70 mm Hg, pulse rate was 65 bpm, O2 Sat: 96%. GRACE risk score was 202 (high), CRUSADE bleeding score: 36 (moderate risk). The ECG showed normal sinus rhythm, Q-waves in DI and aVL with ST-segment elevation (> 0.1 mV) in DI, DII, DIII, aVF, V5, V6 (Fig. 1A). The emergency echocardiogram revealed the akinesia of mid-distal segments of inferior, anterolateral and inferolateral walls and a moderately impaired left ventricle systolic function with ejection fraction (EF) of 45–50%. According to the current ESC guidelines for STEMI [5] urgent PCI via radial artery puncture was performed. The patient was pre-medicated with antiplatelets (300 mg of aspirin plus a loading dose of ticagrelor 180 mg orally) and 5000 UI of unfractionated heparin (UFH) i.v.
|
|
|
Fig. 1. The admission twelve-lead electrocardiogram showed an ST elevation in inferior and lateral leads (A). Registration to the polygraph during PCI on circumflex (LCX) artery (B) and after total occlusion of LAD with the patient in respiratory arrest associated with hypotension and sinus bradycardia (C). ECG post-PCI displays a good resolution of ST-segment elevation (D). |
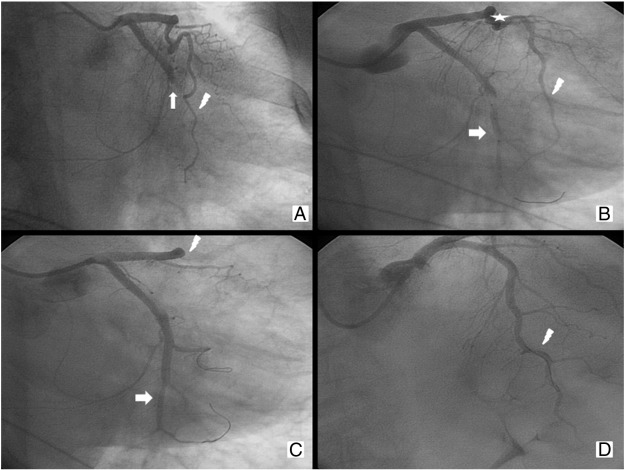
The angiograms showed acute occlusion of the proximal part of the circumflex artery (LCX). We also noticed a myocardial bridge localized in the middle segment of the left anterior descending coronary artery (LAD). LAD and right coronary artery (RCA) were free from significant stenosis (Fig. 2A). Coronary angioplasty for the culprit lesion was planned. A bolus of abciximab i.v. (0.25 mg/Kg) was then administrated. During the intervention procedure, we used a 6 F guiding catheter (Cordis® XB 3.5 6 F) and two 0.014 in. guide wires (Abbott Vascular®, Hi-Torque Balance Middleweight Universal 0.014″ 190 cm). After the insertion of the first guide wire to protect the left marginal artery and the second guide in the LCX we performed a pre-dilation with a compliant balloon (Cordis® EMPIRA™ 2.50 mm × 15 mm 139 cm). Then a bare metal stent (Medtronic® Integrity BMS 2.75 mm × 22 mm) was implanted in the culprit lesion with complete recovery of patency in the LCX and TIMI flow grade 3 (Fig. 2B). The patient was, however, still symptomatic for chest pain. The procedure was complicated by hypotension, vomiting and subsequent respiratory arrest. Resuscitation was started successfully. The check angiography showed total occlusion of middle segment of LAD with thrombus (Fig. 2C). We immediately started i.v. infusion of abciximab (0.125 μg/kg/min for 12 h). LAD was opened with the passage of one guide wire and intracoronary infusion of adenosine and angioplasty (POBA) in the middle part with the balloon of the stent just released on LCX. Final TIMI flow was grade 2 (Fig. 2D). The patient experienced immediate relief of chest pain but clinical course was complicated by a hypertensive pulmonary oedema (Killip II) which was successfully treated with nitrate and furosemide i.v. The post-PCI electrocardiogram showed the resolution of ST-segment elevation (Fig. 1D); the echocardiogram showed akinesia of middle-distal segment of anterolateral, inferolateral and anterior walls with EF 38%. The patient was discharged 10 days later on aspirin, ticagrelor, beta blocker, statin, ARBs, spironolactone and lansoprazole, with improved clinical conditions and completely asymptomatic in the follow-up at a month. Last transthoracic echocardiogram showed hypokinesis of the lateral and posterior walls and improved systolic function (EF 50%).
|
|
|
Fig. 2. The angiogram shows acute occlusion of the proximal part of circumflex artery (arrow) and the LAD (flash) well-developed and free from stenosis with the myocardial bridging (star) in the middle part (A). Released bare metal stent (BMS) on LCX middle part (arrow). LAD to view (flash) (B). Check angiogram indicated good final result on LCX with TIMI 3 flow (arrow) and the total occlusion of the proximal LAD (flash) (C). Reopened of the LAD (flash) with adenosine i.c. and guide wire and subsequent POBA in the middle part with final TIMI grade flow 2 (D). |
Conclusion
In our knowledge, it is the first case reported in literature of acute and spontaneous total occlusion of LAD during PCI for STEMI in occluded LCX (culprit lesion). Indeed it has been previously published just a similar case of iatrogenic (vs spontaneous) occlusion of a not culprit coronary artery. In our case the complication is not due to the movement of the guide wire or the balloon/stent in the vessel, nor to plaque rupture. One of the possible causes of thrombus formation on LAD may be the presence of myocardial bridging. Moreover, in our opinion its important to underlie that the occlusion occurred despite optimal medical therapy (UHF, aspirin, ticagrelor and abciximab) suggested from the latest guidelines [7]. This means that even the novel anti-platelets drugs are not always so efficient in the setting of acute coronary syndrome.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- [1] S.J. Brener; Insights into the pathophysiology of ST-elevation myocardial infarction; Am Heart J, 151 (2006), p. S4eS10
- [2] Ajay J. Kirtane, et al.; Association between intraprocedural thrombotic events and adverse outcomes after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (a Harmonizing Outcomes With RevasculariZatiON and Stents in Acute Myocardial Infarction [HORIZONS-AMI] substudy); Am J Cardiol, 113 (1) (2014), pp. 36–43
- [3] H. Yasuda, T. Hiraishi, S. Sumitsuji, Y. Nakagawa, A. Fukuhara, E. Tsuchikane, et al.; Comparison of quantitative coronary angiographic results after directional coronary atherectomy and balloon angioplasty of protected left main coronary stenosis; Cathet Cardiovasc Diagn, 44 (1998), pp. 138–141
- [4] R.H. Mehta, K.J. Harjai, D. Cox, G.W. Stone, B. Brodie, J. Boura, et al.; Primary Angioplasty in Myocardial Infarction (PAMI) Investigators. Clinical and angiographic correlates and outcomes of suboptimal coronary flow in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention; J Am Coll Cardiol, 42 (10) (Nov 19 2003), pp. 1739–1746
- [5] Ph. Gabriel Steg, Stefan K. James, The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), et al.; ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation; Eur Heart J, 33 (2012), pp. 2569–2619
- [6] G.W. Stone, C.L. Grines, D.A. Cox, E. Garcia, J.E. Tcheng, J.J. Griffin, et al.; Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) Investigators. Comparison of angioplasty with stenting, with or without abciximab, in acute myocardial infarction; N Engl J Med, 346 (2002), p. 957e966
- [7] H. Gündüz, R. Akdemir, H. Özhan, H. Arinç, C. Uyan; Iatrogenic left main coronary artery thrombosis during percutaneous coronary intervention; Turk Kardiyol Dern Ars, 32 (2004), pp. 197–200
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?