(Created page with "==Summary== ====Background==== Many tumors are small and located around the gastrointestinal (GI) tract, and they are difficult to obtain tissue from for pathological diagno...") |
m (Scipediacontent moved page Draft Content 611376630 to Yang et al 2015b) |
(No difference)
| |
Latest revision as of 13:01, 15 May 2017
Summary
Background
Many tumors are small and located around the gastrointestinal (GI) tract, and they are difficult to obtain tissue from for pathological diagnosis by the guidance of conventional methods (sonography or computed tomography. The aim of this study was to analyze the efficacy and benefit of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) in the clinical diagnosis of solid tumors in the mediastinum and abdomen.
Patients and methods
Data from 233 patients with solid tumors on or around the GI tract were reviewed. They had received successful EUS-FNA without on-site cytopathology study.
Results
The lesions were classified according to the anatomic location as pancreatic tumors (Group A, n = 91), mediastinal tumors (including lymph nodes) (Group B, n = 38), abdominal tumors (including lymph nodes) (Group C, n = 49), focal transmural thickening of the GI tract (Group D, n = 6), and submucosal tumors of the GI tract (Group E, n = 49). The accuracies of pathological diagnosis of malignancy were 79.2%, 76.9%, 93.2%, and 80% for Groups A–D, respectively. The overall accuracy for malignancy was 82.9%. For the submucosal tumors of the GI tract in Group E, FNA cytopathology provided evidence of specific diagnosis all were GI stromal tumor in 47% of the cases, 14% were diagnosed as suspicious (most were of a spindle cell tumor nature), and 39% were considered negative of tumor or non-diagnostic. There were three episodes (1.3%) of complication (GI bleeding, n = 1; septic fever, n = 1; gallbladder puncture, n = 1) which occurred among all patients in this study, and all of them were treated appropriately, with no occurrence of life-threatening events.
Conclusion
EUS-FNA appears to be a very useful tool for obtaining tissue diagnosis for lesions that are inaccessible by the conventional methods and was shown to be a safe and effective technique in the hands of experienced operators. Pathological diagnosis can be obtained for the guidance of clinical management to avoid the more invasive ways, such as surgery or mediastinal scope.
Keywords
Abdominal tumor ; Endoscopic ultrasound guided fine needle aspiration (EUS-FNA) ; Mediastinal tumor
Introduction
Clinically, many tumor lesions are located on or around the gastrointestinal (GI) wall. Standard transabdominal ultrasound and computed tomography (CT) are used to guide fine-needle aspiration (FNA) for the purpose of pathological diagnosis or tumor staging [1] ; [2] . Ultrasound guidance is usually preferred over CT because ionizing radiation is avoided and the needle is visualized in real-time, but there are several disadvantages including difficulty in visualizing the needle tip clearly and consistently, presence of overlying bowel gas, and inability to delineate intervening tissues [3] ; [4] . Furthermore, many of these lesions are often too small to be properly detected and evaluated by conventional sonography or a CT scan [5] .
Endoscopic ultrasound (EUS) is now widely applied for the visualization of the GI wall and the surrounding structures, and for the staging of GI tumors [6] ; [7] . Linear scanning ultrasonography allows for close tracking of a needle as it is advanced into the ultrasound plane and thus this technology has led to the development of EUS-guided FNA (EUS-FNA) biopsy. Vilmann et al [8] reported the first case of FNA cytology and Grimm et al [9] treated a case with a pseudocyst by EUS-FNA in 1992. Since then, EUS-FNA has become more popular in the clinical diagnosis, especially in the Western world. According to the literature, the accuracy of EUS-FNA has been 70–100% in mediastinal or intra-abdominal tumors and was relatively lower (38–100%) in GI wall lesions such as submucosal tumors [10] ; [11] ; [12] ; [13] ; [14] ; [15] . However, this modality has still not been so widely applied in Asian countries, because it is technically challenging [11] . Another barrier to more widespread adoption of EUS-FNA is the small size of aspirated specimens it can provide due to the small caliber of the needle. Making the correct cytopathological diagnosis with a EUS-FNA specimen remains a challenge [16] ; [17] ; [18] .
The purpose of the present study was to assess the efficacy and safety of EUS-FNA for clinical diagnosis of solid tumors in the mediastinum and abdomen.
Patients and methods
Patient selection
From January 2005 to December 2012, 268 patients with tumor lesions received EUS-FNA for clinical diagnosis in this hospital. Patients were recruited into this study if they fulfilled the following conditions: (1) a tumor lesion on the wall of the GI tract that could not be accurately diagnosed by endoscopic biopsy; and (2) a tumor lesion around the GI tract that was difficult to access by conventional ultrasonography or CT scan. The exclusion criteria for EUS-FNA were: (1) patients who declined to undergo the procedure; (2) evidence of coagulopathy, or lesion could not be punctured safely with the needle under linear array endosonography; (3) patients underwent EUS-FNA for cystic lesions (cystic space > 25% of the lesion); and (4) patients under EUS-FNA for the inclusion criteria but the final outcome cannot be verified.
EUS-FNA
An Olympus EU-C2000 EUS center and a linear scanning ultrasound transducer UC2000P (Olympus, Tokyo, Japan) were used for image observation and puncture guidance. A 22-gauge needle including NA-11J-KB/EZ shot (Olympus) and EUSN-1 (Cook Medical, Winston-Salem, NC, USA) was used in all of the puncture procedures. All patients provided informed consent prior to examination. Routine premedication for endoscopy was conducted with intramuscular injections of buscopan (20 mg) and pethidine 25–50 mg, followed by pharyngeal anesthesia. Intravenous injection of midazolam 3 mg was given when required for mild sedation (rarely needed in this study). The lesions were scanned with EUS to determine the proper route of puncture. Power Doppler ultrasonography was used to avoid injury to vessels.
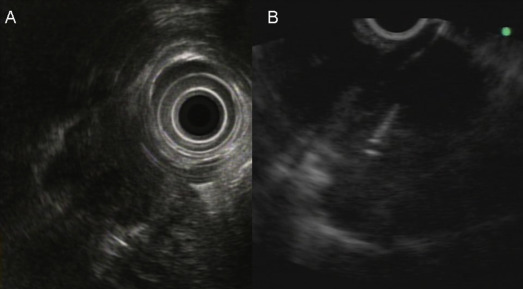
When it was confirmed in the EUS image that the needle had been properly inserted into the lesion, the stylet of the needle was removed and the needle was connected to a syringe with a negative pressure (0∼10 mL). The needle was then moved back and forth > 10 times to obtain a tissue specimen (Fig. 1 ). After withdrawing the needle, the target lesion was observed by EUS to determine whether any changes (shape or internal texture) occurred in the tumor. The adjacent tissue was also carefully observed to determine whether there were any changes, such as hematoma. Because on-site cytopathologic evaluation was not available in our hospital, the needle punctures were repeated several times (2∼5 times puncture when possible) until there was gross evidence that tissue particles had been obtained, or the maximal number of punctures had been performed. At the end of the procedures, absence of bleeding at the point of puncture was confirmed endoscopically. Aspirates were prepared on glass slides and fixed in absolute alcohol solution for the cytological study. When sufficient materials had been obtained, the specimens were also put in the formalin solution for pathological evaluation (hematoxylin-eosin staining and other immunohistochemical stains as necessary).
|
|
|
Figure 1. A patient with pancreatic head neuroendocrine tumor and mediastinal lymph node metastasis diagnosed by endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) cytopathology. (A) The EUS image of the mediastinal lymph node by radial echoprobe and (B) the EUS image of the performance of EUS-FNA.
|
Final diagnosis and statistical analysis
The final diagnosis of malignancy was verified if any of the aspiration/biopsy for the lesion revealed a definite diagnosis of malignancy. If negative results of malignancy were noted from the procedure, the diagnosis were the surgical pathology if a surgery was performed. When a cytopathological diagnosis was not obtained, a diagnosis of malignancy was still made if the physicians who were taking care of the patient were confident of the clinical diagnosis of malignancy (usually by images). The negative malignancy state was verified by long-term clinical follow up. A negative malignancy state without surgical pathology was defined as no prominent progression (< 25% size) of the target lesion after a 1-year follow-up duration. The results of the procedure were compared with the final diagnosis to evaluate the accuracy of this procedure. The safety profile, including minor and major complications, was also analyzed and reported. The diagnostic yield including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated for EUS-FNA by comparing the results of these techniques with the final diagnosis.
Ethical approval
This study was approved by the Ethics Committee of our hospital. Written consent was obtained from each patient or a relative.
Results
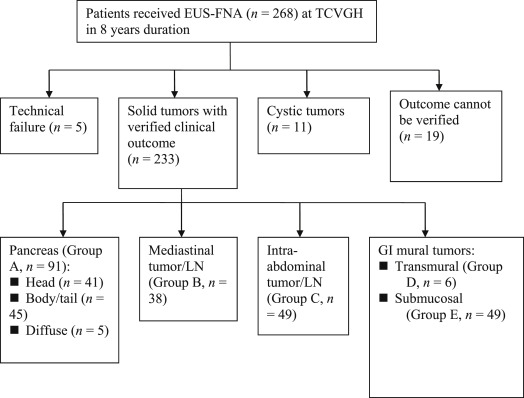
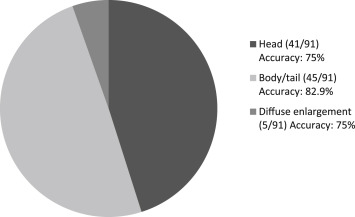
Among the 268 patients, 233 patients with successful FNA procedures for solid tumors (98 women, 135 men) with verified clinical outcome for review were included in this study. These patients were classified according to the anatomic location of the lesions as pancreatic tumors (Group A, n = 91), mediastinal tumors (including lymph node) (Group B, n = 38), abdominal tumorous lesions (including lymph node) (Group C, n = 49), focal transmural thickening of the GI tract (Group D, n = 6, all were with nonspecific diagnosis from endoscopic biopsy), submucosal tumors of the GI tract (Group E, n = 49) ( Table 1 ; Fig. 2 ). The accuracies of pathological diagnosis of malignancy were 79.2%, 76.9%, 93.2%, and 80% for groups A–D, respectively. The respective sensitivity, specificity, PPV, NPV are also shown (Table 2 ). The respective proportion of the pancreatic tumors according to the different locations and their diagnostic accuracies are shown in Fig. 3 . In total, for all of these lesions, the overall accuracy for the diagnosis of malignancy was 82.9%. For the stromal tumors of the GI tract in Group E (all originating from below the submucosal layer), FNA cytopathology showed evidence of specific diagnosis of GIST in all (47%) of these cases, 14% were diagnosed as suspicious (most were of a spindle cell tumor nature, except for one adenocarcinoma) and 39% were considered negative for tumor or non-diagnostic. For the patients with negative or non-diagnostic FNA cytopathology, none were found to have an outcome of malignancy progression or tumor-related morbidity/mortality (Fig. 3 ).
| Clinical characteristics | No. (%) |
|---|---|
| Age (y) | 34∼82 (mean: 67 ± 14.5) |
| Sex | |
| Male | 135 (57.9) |
| Female | 98 (42.1) |
| Tumor size (cm)a | 1∼7 (mean: 3.2 ± 2.8) |
| Tumor location | |
| Pancreas (Group A) | 91 (39.1) |
| Head | 41 (45.1) |
| Body/tail | 45 (49.5) |
| Diffuse enlargement | 5 (5.4) |
| Mediastinum (Group B) | 38 (16.3) |
| Intra-abdomen (Group C) | 49 (21.0) |
| Transmural wall thickening (Group D) | 6 (2.6) |
| Submucosal tumor (Group E) | 49 (21.0) |
| Needle puncture No. | 2–5 (mean: 2.6 ± 2.1) |
a. Not including the diffuse enlargement of pancreatic tumors and the transmural gastrointestinal (GI) lesions.
|
|
|
Figure 2. Patient recruitment and classification according to anatomical characteristics of the lesions.
|
| Group | Lesion location | No. of patients | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|---|---|
| A | Pancreas | 91 | 80.5 | 100 | 100 | 48.3 | 79.2 |
| B | Mediastinum | 38 | 73.1 | 91.7 | 95 | 61.1 | 76.9 |
| C | Intra-abdomen | 49 | 90.9 | 80.0 | 97.6 | 50 | 93.2 |
| D† | GI –thickening (transmural) | 6 | 80 | 100 | 100 | 50 | 80.0 |
| All | 184 | 82.2 | 93.8 | 98.4 | 52.6 | 82.9 |
NPV = negative predictive value; PPV = positive predictive value; TCVGH = Taichung Veterans General Hospital; LN = lymph node.
|
|
|
Figure 3. Number, proportion, and diagnostic accuracies of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for the pancreatic tumor according to the different tumor locations.
|
About two thirds of these cases received FNA at the outpatient clinic. These patients recovered from the light sedation shortly after the procedure and were discharged without complication. There were three episodes of complication (UGI bleeding, n = 1; septic fever, n = 1; gallbladder puncture, n = 1) among all patients (1.3%) in this study. The gallbladder puncture was related to the incorrect interpretation of an EUS image for a paragastric GIST due to echoprobe dysfunction, and cholecystectomy was performed during the elective gastrectomy. The case of UGI bleeding was related to incidental puncture of a gastric wall vessel and such events are rare. The case of septic fever may be due to a tumor necrosis effect after repeated punctures (no bacteremia was found through the course). All of these three patients recovered uneventfully after appropriate treatment.
Discussion
The study results show that the yield of punctures differed according to the lesions with location of the puncture and the pathological nature. The best diagnostic yields were from the aspiration of enlarged lymph nodes or tumors from the intra-abdominal region. Pancreatic tumors constituted the largest proportion of the targets of EUS-FNA because most suspected pancreatic malignancies were out of the range of surgical resection. Tissue diagnosis is thus important for further management. The accuracy of EUS-FNA for pancreatic tumors overall was 79.2%. The accuracy was better for tumors over the body or tail of the pancreas (82.9%), but was relatively lower (75%) for tumors on the pancreatic head, especially the uncinate process. The relatively low yield rate may have been due to necrosis inside the tumor and technical difficulty on this area. Performing puncture for the pancreatic head lesions, especially the uncinate process, was the most difficult, because a certain amount of bending and twisting of the echoendoscope is needed to correctly position the instrument for puncture and this brings considerable resistance for the needle to extrude from the sheath. The pushing force, thus, cannot be transmitted to the needle from the proximal handle [11] . In some cases, collateral vessels were seen around the pancreatic head due to the compression or invasion of the tumor and this hindered the access of the needle. In fact, three of five patients with EUS-FNA failure had pancreatic head lesions.
The accuracy of EUS-FNA for the abdominal tumors other than the pancreas was 93.2%, and this high yield rate was highly related to the low necrotic nature of the lymph node as well as the tissue characteristics. Technically, the puncture of the mediastinal lymph node was the easiest, because it is usually possible to maintain the echoprobe in a relatively straight position [19] . However, the accuracy for the mediastinal lesion was lower than that for abdominal lesions, which may have been due to the relatively smaller tumor size and the higher risk associated with the puncture over this location.
Most of the mural lesions were submucosal tumors originating from below the submucosal layer. For the lesions which received FNA in our hospital, the size was usually intermediate (2∼4 cm in diameter). For tumors > 4 cm, needle puncture was not usually necessary, because surgical resections were always the first option unless there were unresectable, or a poor surgical condition was considered. For tumors < 2 cm, malignant behavior is unusual and so endoscopic follow-up was typically suggested. For those submucosal tumors which received FNA, a diagnostic yield of 61% was attained if samples with spindle cell cytology were included. Only 47% of lesions could be given a more precise pathologic diagnosis (all were GIST). However, evaluation of the malignant potential, such as mitotic figures, is still difficult due to the small size of the specimens. This phenomenon in the present study is comparable with the results of previous studies [16] . The difficulty of performing puncture for submucosal tumors depends on the size of the tumor and also on the location. If the tumor was > 3 cm, the puncture was not too difficult irrespective of the location. However, for a smaller tumor, location over the fundus and the lesser curvature side of the antrum result in a relatively difficult puncture, because the echoscope must be placed in a tortuous position.
Another possible cause of the relatively low yield of submucosal tumor subjected to aspiration was the nature of the fibrous stroma [17] . The aspiration content in our study was usually low despite our best efforts. There is still much room left for improvement of aspiration from submucosal tumors. The usage of larger bore puncture needles or the Tru-cut needle may help to acquire a greater volume of specimens, although its application may be more difficult compared with the use of a conventional small bore needle [20] . The application of a special immunohistochemical stain may also improve the diagnostic rate for specimens with a small volume [21] . The application of FNA for submucosal tumors provides other advantages. Dig-in biopsy or strip biopsy were also used to obtain tissue from submucosal tumors. However, this may create a large mucosal defect on the tumor and recurrent tumor bleeding may occur.
There were several cases (1.9%) for which successful puncture of the target lesion could not be accomplished when we attempted to perform FNA. In most of these cases, the lesions were small and located on the pancreatic neck or uncinate process, requiring considerable bending of the echoscope to orient the needle, and this caused great friction between the needle and its outer sheath. Concerning the safety of the procedure, puncture performed with a 22G fine needle for a solid mass lesion is generally considered to be safe, because significant complications are rare. Three complications (1.3%) in all puncture cases occurred in this study. The complications of these three patients improved after medical or surgical treatment. However, complications such as bleeding may still occur if the needle punctures a large vessel [22] . A clear visualization of the needle on the sonographic scanning is very important, especially in the mediastinum, due to the close proximity of the mediastinal large vessels.
With the help of curvilinear electronic echoendoscopy, the puncture needle can be visualized clearly in most situations. Therefore, EUS provides a safe and reliable modality for obtaining pathological specimens [23] ; [24] . However, the puncture needle should be visualized clearly on sonographic monitoring. If visualization of the needle becomes compromised, the puncture should not proceed unless the needle can be redirected in the appropriate orientation.
Clinical benefits are evident if a malignant state can be proved by the FNA procedure, because tissue diagnosis is often crucial for the clinical decision. Further treatment planning may include surgery, chemotherapy, or just hospice care can be proceeded. Thus, patients can be spared from a more invasive way such as surgery or mediastinal scope for tissue diagnosis. There was no on-site cytopathologic evaluation in this study. The adequacy of FNA specimens can be judged grossly by the appearance of tissue fragments or tissue particles evident on the smear. If the specimens were bloody, gross interpretation of adequacy was difficult, so on-site cytopathology would be helpful as it would obviate the need for additional puncture. However, on-site cytopathology is not always available.
In summary, EUS-FNA was demonstrated to be a very useful tool for performing tissue diagnosis of lesions that are inaccessible by conventional methods. The technique was shown to be extremely safe and was effective in the hands of experienced operators, even without on-site cytopathology. The accuracy of this diagnostic tool depends on the experience of the operator performing the puncture technique, appropriate tumor position, and the tumor pathology.
Conflicts of interest
All authors declare no conflicts of interest.
Acknowledgments
This study was supported in part by grants from Taichung Veterans General Hospital , Taichung, Taiwan (TCVGH-933304B ), and the statistical results were verified by the Biostatistics Task Force of Taichung Veterans General Hospital.
References
- [1] J.F. Botet, C.J. Lightdale, A.G. Zauber, H. Gerdes, C. Urmacher, M.F. Brennan; Preoperative staging of esophageal cancer: comparison of endoscopic US and dynamic CT; Radiology, 181 (1991), pp. 419–425
- [2] T. Rosch, R. Lorenz, K. Zenker, A. von Wichert, H. Dancygier, H. Höfler, et al.; Local staging and assessment of resectability in carcinoma of the esophagus, stomach and duodenum by endoscopic ultrasonography; Gastrointest Endosc, 38 (1992), pp. 460–467
- [3] H. Snady, A. Cooperman, J.H. Siegel; Endoscopic ultrasonography compared with computed tomography and ERCP in patients with obstructive jaundice or small peripancreatic mass; Gastrointest Endosc, 38 (1992), pp. 27–34
- [4] T. Rosch, C. Braig, T. Gain, S. Feuerbach, J.R. Siewert, V. Schusdziarra, et al.; Staging of pancreatic and ampullary carcinoma by ultrasonography; Gastroenterology, 102 (1992), pp. 188–199
- [5] J.F. Botet, C.J. Lightdale, A.G. Zauber, H. Gerdes, S.J. Winawer, C. Urmacher, et al.; Preoperative staging of gastric cancer: comparison of endoscopic US and dynamic CT; Radiology, 181 (1991), pp. 426–432
- [6] E.P. DiMagno, P.T. Regan, J.E. Clain, E.M. James, J.L. Buxton; Human endoscopic ultrasonography; Gastroenterology, 83 (1982), p. 824
- [7] S.J. Gordon, Rifkin, B.B. Goldberg; Endosonographic evaluation of mural abnormalities of the upper gastrointestinal tract; Gastrointest Endosc, 32 (1986), p. 193
- [8] P. Vilmann, G.K. Jacobsen, F.W. Henriksen, S. Hancke; Endoscopic ultrasonography with guided fine needle aspiration biopsy in pancreas disease; Gastrointest Endosc, 38 (1992), pp. 172–173
- [9] H. Grimm, K. Binmoeller, N. Soehendra; Endosonography guided drainage of a pancreas pseudocyst; Gastrointest Endosc, 38 (1992), p. 170
- [10] M.J. Wiersema, M.L. Kochman, H.M. Cramer, L.C. Tao, L.M. Wiersema; Endosonography-guided real-time fine-needle aspiration biopsy; Gastrointest Endosc, 40 (1994), pp. 700–707
- [11] F.G. Gress, R.H. Hawes, T.J. Savides, S.O. Ikenberry, G.A. Lehman; Endoscopic ultrasound guided fine-needle aspiration biopsy using linear and radial scanning endosonography; Gastrointest Endosc, 45 (1997), pp. 243–250
- [12] K.J. Chang, P. Nguyen, R.A. Erickson, T.E. Durbin, K.D. Katz; The clinical utility of endoscopic ultrasound-guided fine-needle aspiration in the diagnosis and staging of pancreas carcinoma; Gastrointest Endosc, 45 (1997), pp. 387–393
- [13] B.R. Stotland, M.L. Kochman; Diagnostic and therapeutic endosonography: endoscopic ultrasound-guided fine-needle aspiration in clinical practice; Gastrointest Endosc, 45 (1997), pp. 329–331
- [14] D.B. Willams, A.V. Sahai, L. Aabakken, I.D. Penman, A. van Velse, J. Webb, et al.; Endoscopic ultrasound guided fine needle aspiration biopsy: a large single centre experience; Gut, 44 (1999), pp. 720–726
- [15] K.J. Chang, K.D. Katz, T.E. Durbin, R.A. Erickson, J.A. Butler, F. Lin, et al.; Endoscopic ultrasound guided fine-needle aspiration; Gastrointest Endosc, 40 (1994), pp. 694–699
- [16] M.J. Wiersema, P. Vilmann, M. Giovannini, K.J. Chang, L.M. Wiersema; Endosonography-guided fine-needle aspiration biopsy: diagnostic accuracy and complication assessment; Gastroenterology, 112 (1997), pp. 1087–1095
- [17] M. Giovannini, J.F. Seitz, G. Monges, H. Perrier, I. Rabbia; Fine-needle aspiration cytology guided by endoscopic ultrasonography: results in 141 patients; Endoscopy, 27 (1995), pp. 171–177
- [18] K.J. Chang, C.G. Albers, R.A. Erickson, J.A. Butler, R.B. Wuerker, F. Lin; Endoscopic ultrasound-guided fine needle aspiration of pancreatic carcinoma; Am J Gastroenterol, 89 (1994), pp. 263–266
- [19] M.F. Catalano, S. Sial, A. Chak, M.V. Sivak Jr., R. Erickson, J. Scheiman, et al.; EUS-guided fine needle aspiration of idiopathic abdominal masses; Gastrointest Endosc, 55 (2002), pp. 854–858
- [20] K. Okubo, K. Yamao, T. Nakamura, M. Tajika, A. Sawaki, K. Hara, et al.; Endoscopic ultrasound-guided fine-needle aspiration biopsy for the diagnosis of gastrointestinal stromal tumors in the stomach; J Gastroenterol, 39 (2004), pp. 747–753
- [21] K.M. Hoda, S.A. Rodriguez, D.O. Faigel; EUS-guided sampling of suspected GI stromal tumors; Gastrointest Endosc, 70 (2009), pp. 254–261
- [22] M. Arima, M. Tada; Endoscopic ultrasound-guided fine needle aspiration biopsy in esophageal and mediastinal diseases: clinical indications and results; Digestive Endoscopy, 15 (2003), pp. 93–99
- [23] M. Kida, Y. Saito; EUS-guided FNA for the improvement in the rate of extraction and diagnostic capability. What is the standard of EUS guided FNA in Japan?; Digestive Endoscopy, 16 (Suppl.) (2004), pp. S100–S103
- [24] M.F. Catalano, M.L. Rosenblatt, A. Chak, M.V. Sivak Jr., J. Scheiman, F. Gress; Endoscopic ultrasound–guided fine needle aspiration in the diagnosis of mediastinal masses of unknown origin; Am J Gastroenterol, 97 (2002), pp. 2559–2565
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?