(Created page with " ==Summary== Perforation peritonitis is the most common surgery performed in an emergency. Upper gastrointestinal tract perforation is more common than lower gastrointestina...") |
(No difference)
|
Revision as of 12:17, 26 May 2017
Summary
Perforation peritonitis is the most common surgery performed in an emergency. Upper gastrointestinal tract perforation is more common than lower gastrointestinal perforation. Multiple peptic perforations in an individual are a relatively rare entity, with fewer than 10 cases reported in the literature. The factor that contributes the most for the occurrence of multiple peptic perforations is analgesic and steroid abuse. Herein, we report a rare case of double peptic perforation in a middle-aged man with history of analgesic use for 18 months.
Keywords
double peptic perforation;NSAIDS abuse
1. Case report
A 42-year-old man presented to the surgical outpatient department of our hospital with a history of abdominal pain, vomiting for 3 days, and constipation and fever for 2 days. There was history of sudden pain in upper abdomen followed by vomitting. Pain was of severe grade and not relieved by medication. He had not passed flatus or feces for 2 days. He had also had fever with chills for 2 days. The patient had significant history of taking nonsteroidal anti-inflammatory drugs (NSAIDs) for toothache for the last 18 months. He was a smoker, nondrinker, and vegetarian.
On admission, he had pallor, tachypnea, tachycardia (110 beats/min), and a fever of 38.5 °C, as well as a rigid abdomen. Guarding and rigidity were present and occasional bowel sounds were also noted. A flat plate skiagram of the abdomen demonstrated free gas under both hemidiaphragms. Preoperative investigations demonstrated altered renal function test (serum urea, 84 mg/L; serum creatinine, 2.8 mg/dl) and dyselectrolytemia (serum sodium 131 meq/L, serum potassium, 2.1 meq/L). The patient was stabilized hemodynamically and broad-spectrum antibiotics, usually a combination of injectable third generation cephalosporin and metronidazole, were administered. After initial resuscitation (placement of intravenous lines and nasogastric tube followed by adequate administration of fluids), the patient underwent an emergency exploratory laparotomy.
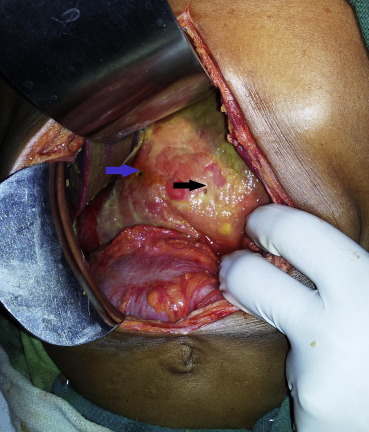
On exploration, 1500 mL of dirty bilious fluid were removed. There was gross peritoneal contamination with flakes all over the gut and in the subhepatic region. After thorough peritoneal lavage, two gastric perforations were identified, one in the prepyloric region of ∼0.75 cm × 0.5 cm and another ∼0.5 cm × 0.5 cm was present over the body of the stomach along the greater curvature (Fig. 1). Both of these perforations were repaired with a 2-0 silk interrupted suture with omental patch in between (Fig. 2). A 30F abdominal drain was placed in the pelvis and anatomical closure was done in layers. The patient recovered completely and was discharged uneventfully on the 10th postoperative day.
|
|
|
Figure 1. Multiple gastric perforations.
|
|
|
|
Figure 2. Repairing the perforations.
|
Postoperative gastroscopy revealed erosive gastritis involving the majority of the greater curvature and prepyloric region.
2. Discussion
Peptic perforation is the most prevalent surgical emergency. With high mortality and morbidity, peptic perforation is most commonly present in the first part of the duodenum (35–65%), with 25–45% located in the pylorus, and 5–25% in the stomach.1
The etiological factors responsible for peptic perforation and annual incidence vary depending upon sociodemographic factors,2 ; 3 The factors that contribute the most for occurrence of peptic perforation are Helicobacter pylori infection and chronic use of NSAIDs. 4 Gastrointestinal perforation in our region generally occurs as a result of chronic inflammation due to H. pylori, NSAIDs such as Aspirin, stress, excessive smoking, and consumption of alcohol, coffee, and spicy food. Because these two factors, NSAIDs and H. pylori, produce gastroduodenal injury through different mechanisms, they may have additive effects in terms of producing ulcers. This is quite a controversial issue, with conflicting results having been reported as to the presence or absence of such an interaction. Hawkey suggested that in patients with chronic NSAID use, those who are H. pylori positive are less likely to develop ulcers, particularly if taking acid-suppressive therapy. 5
We successfully managed a rare and interesting case of double perforation of the stomach. While studying our case retrospectively we discovered that our patient had been taking analgesics for toothache for the preceding 18 months and was a known smoker. Studies have demonstrated the obvious relationship of analgesic abuse, smoking, and peptic perforation.6 The occurrence of multiple peptic perforations is a rare entity in which multiple gastric perforations are further not very common. Multiple peptic perforation reported are due to analgesic (NSAID) or steroid abuse, Zollinger–Ellison syndrome, burn, postsurgery stress, tubercular stromal ulcer, or Degos disease.7; 8; 9; 10 ; 11 After a thorough literature search, only eight cases were found (Table 1). Most of the gastric perforations are located along lesser curvature while in our case, one was along the greater curvature and the other in the prepyloric region (Fig. 2).
| Ref no. | Author | Year | Sex | Medical history | Coexisting disease | Condition |
|---|---|---|---|---|---|---|
| 10 | Kanai M et al | 1988 | Male | Leg pain | Degos' disease | Multiple gastric and ileal perforations |
| 11 | Grigirov et al | 1968 | Male | Steroid therapy | n/a | Morbid |
| ??? | Maly L | 1996 | Male | Recurrent pain abdomen | Gall bladder perforation | Double gastric perforation with gall bladder Perforation |
| 12 | Kuzionov and Polinkova | 1973 | Male | n/a | Isolated gastric Tuberculosis | Morbid |
| ??? | Dahm | 1962 | Male (4 y) | n/a | n/a | Multiple duodenal perforation |
| 13 | Mynhardat | 1951 | Male | n/a | Peptic ulcer disease with burn | Double duodenal perforation |
| 14 | Chaudhary et al | 1965 | Male | n/a | n/a | Simultaneous multiple peptic peroration |
| 15 | Akhmedzhanov I et al | 1979 | Male (2 mo) | Pyloric stenosis | Pyloromyotomy |
n/a = not applicable.
Gastroscopy performed 6 weeks postoperatively revealed erosive gastritis at the greater curvature and prepyloric region. This further confirms the occurrence of gastric perforation due to NSAID abuse in our case: because of gravity, the inciting agents lie on the greater curvature of the stomach. This explains the development of acute gastritis distally on or near the greater curvature of the stomach in the case of orally administered NSAIDs. Patients with H. pylori infection are usually asymptomatic but in our case, patient who present with upper abdominal pain for more than 6 months with endoscopic finding of lower abdominal gastritis and from area which are endemic for H. pylori infection are taken as H. pylori Positive. However, we advise all the patients to take H. pylori eradication therapy for 2 weeks, especially in tropical countries such as India where prevalence of H. pylori infection is very high; it is also the most common etiology for occurrence and recurrence of peptic perforation. 1 ; 7 A recent study based on endoscopic findings also confirmed the propensity of multiple peptic perforation in NSAID abusers, regardless of H. pylori infection. 12
Increased age, delay in operation, and NSAID abuse adversely affect the operative death rate.13 The best surgical option for these patients is simple closure with omental patch. It is the easiest, quickest, safest operation, and can be applied to all situations by every surgeon; moreover, it can be complemented later with an effective medical treatment that should include eradication of H. pylori.
For peptic perforation, a Graham patch repair, with or without an acid reducing surgery is probably the most appropriate management. In our patient we repaired both the perforation with Graham patch technique and administered acid suppression therapy postoperatively. Every surgeon should strictly follow the basic principles for abdominal surgery. Exploration with thorough peritoneal lavage should be done in every case of perforation peritonitis, even if the pathology appears obvious to avoid missing the rare but important possibility of multiple peptic perforations.
3. Conclusion
Multiple peptic perforations are rare but could potentially be lethal if missed. One should always keep the possibility of multiple perforations in mind. Analgesic abuse appears to be the underlying cause for multiple perforations. Repair of the perforation with Graham patch with acid suppression therapy with analgesic (NSAID) avoidance is the treatment of choice for multiple peptic perforations. Postoperatively, a proton pump inhibitor with anti-H. pylori regimen, especially in tropical countries, should be given to patients with multiple peptic perforations.
References
- 1 O.B. Bulut, C. Rasmussen, A. Fischer; Acute surgical treatment of complicated peptic ulcers with special reference to the elderly; World J Surg, 20 (1996), pp. 574–577
- 2 C. Svanes, H. Salvesan, B. Espehaug, O. Søreide, K. Svanes; A multifactorial analysis of factors related to lethality after treatment of perforated gastroduodenal ulcer; Ann Surg, 209 (1989), pp. 418–423
- 3 L. Sharma, S. Gupta, A.S. Soin, S. Sikora, V. Kapoor; Generalized peritonitis in India—the tropical spectrum; Jpn J Surg, 21 (1991), pp. 272–277
- 4 R.J. Hopkins, L.S. Girardi, E.A. Turney; Relationship between Helicobacter pylori eradication and reduced duodenal and gastric ulcer recurrence: a review; Gastroenterology, 110 (1996), pp. 1244–1252
- 5 C.J. Hawkey; What consideration should be given to Helicobacter pylori in treating nonsteroidal anti-inflammatory drug ulcers?; Eur J Gastroenterol Hepatol, 12 (2000), pp. 17–20
- 6 B. Aydinli, O. Yilmaz, G. Ozturk, M.I. Yildigan, N. Gursan, M. Basoglu; Is perforated marginal ulcer after the surgery of gastroduodenal ulcer associated with inadequate treatment for Helicobacter pylori eradication?; Langenbecks Arch Surg, 392 (2007), pp. 593–599
- 7 M. Kanai, S. Kondoh, H. Kuriki, H. Mukaiyama, K. Mori, T. Tanno; A report of an atypical case of Degos' disease with multiple perforations of the stomach and small intestine; Nihon Geka Gakkai Zasshi, 89 (1988), pp. 1127–1131 [Article in Japanese]
- 8 G. Grigorov, F. Mitov; A case of double perforation of duodenal ulcer in a young man following cortisone therapy; Khirurgiia (Sofiia), 21 (1968), pp. 511–512 [Article in Bulgarian]
- 9 M.R. Mynhardt; Double duodenal ulcer with perforation following a burn; S Afr Med J, 25 (1951), pp. 114–115
- 10 M. Chaudhuri, S.B. Chakravorty; Simultaneous multiple peptic perforations; J Indian Med Assoc, 45 (1965), pp. 276–277
- 11 J.C. Rodríguez-Sanjuán, R. Fernández-Santiago, R.A. García, et al.; Perforated peptic ulcer treated by simple closure and Helicobacter pylori eradication; World J Surg, 29 (2005), pp. 849–852
- 12 Mukerjee Prem, Rajor Ravi; Abdominal tuberculosis; IJT, 26 (2) (1979), pp. 62–66
- 13 Y. Kim, S. Yokoyama, J. Watari, et al.; Endoscopic and clinical features of gastric ulcers in Japanese patients with or without Helicobacter pylori infection who were using NSAIDs or low-dose aspirin; J Gastroenterol, 47 (2012), pp. 904–911
- 14 E. Hennessy; Perforated peptic ulcer: mortality and morbidity in 603 cases; Aust N Z J Surg, 38 (1969), pp. 243–252
- 15 A.H. Al salem, C. Grant, S. Khwaja, et al.; Infantile hypertrophic pyloric stenosis and congenital diaphragmatic hernia; J Urol, 121 (2) (1979), pp. 217–220
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?