(Created page with "==Summary== ====Background/Objective==== About 10 years ago, we started to correct buried penis using the technique of modified prepuce unfurling. We have made modifications...") |
m (Scipediacontent moved page Draft Content 160840042 to Chin et al 2014a) |
(No difference)
| |
Latest revision as of 12:30, 26 May 2017
Summary
Background/Objective
About 10 years ago, we started to correct buried penis using the technique of modified prepuce unfurling. We have made modifications in the years since our preliminary results were reported in 2002.
Methods
One hundred and thirty-four patients received modified prepuce unfurling since 2000, with ages ranging from 2 months to 33 years. The surgical procedures included the removal of the narrowest part of the prepuce, dissection of the fibrotic tissue from the Bucks fascia, and unfurling the inner prepuce to cover the penis. Most patients had their procedures in day care service. No urinary catheter was needed. All patients were followed up for at least 2 months.
Results
Most patients had satisfactory results. All patients had the glans exposed after surgery, although one patient needed reoperation for prolonged edema and two patients had wound infections.
Conclusion
Modified prepuce unfurling is a safe and effective method to correct buried penis.
Keywords
buried penis;concealed penis;hidden penis;phimosis;prepuce
1. Introduction
Buried penis is a congenital anomaly that affects the appearance and the function of the external genitalia in boys and men. This anomaly is frequently associated with insufficient outer penile skin, inadequate subcutaneous attachment to the Bucks fascia, and usually, a narrow opening of the prepuce. Surgical correction may be needed because of ballooning of the foreskin while voiding, urine dripping, balanitis, or urinary tract infection, but more often, for the abnormal appearance of the external genitalia.
Numerous surgical techniques have been developed for the correction of this anomaly. Although prepuce unfurling is a relatively simple way to correct the anomaly,1 some patients have prolonged edema after surgery. About 12 years ago, we modified the procedure of preputial unfurling.2 In this retrospective report, we describe our experience of the procedure and the results in 134 patients.
2. Materials and methods
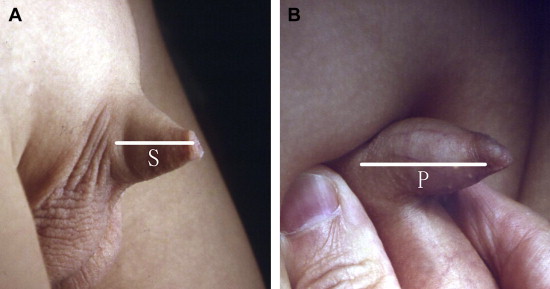
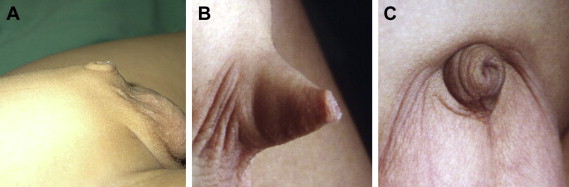
In order to document the severity of buried penis, we developed a method to quantify the anomaly by measuring the length of the penile skin (S) and penile shaft (P) (Fig. 1). S was measured when the penile skin was gently stretched; P was measured by pressing the prepubic fat at the penile base. The severity of buried penis was recorded as S/P ratio (S/P × 100%). We evaluated patients who visited our clinic with complaints of buried penis and separated them into three groups: Group A (severe deficiency of penile skin, S/P ratio < 30%); Group B (moderate deficiency of penile skin, S/P ratio 30–70%); and Group C (mild or no deficiency of penile skin, S/P ratio > 70%) (Fig. 2). Only the patients in Groups A and B were operated using the technique described here.
|
|
|
Figure 1. (A) Measuring the length of penile skin (S) with no or mild skin stretch; (B) measuring the length of the phallus (P) by compression of the prepubic fat.
|
|
|
|
Figure 2. (A) Group A: severe penile skin deficiency; (B) Group B: moderate penile skin deficiency; and (C) Group C: mild penile skin deficiency, much prepubic fat.
|
Since 2000, 134 individuals (36 in Group A, 98 in Group B) with buried penis were operated upon using our modified preputial unfurling. No patient in this series had previous circumcision or other genital surgery. Group C patients (mostly obese patients) were excluded from this procedure. Medical records of the patients were reviewed and analyzed.
All patients underwent surgery with general anesthesia. To minimize postoperative pain, the patients either had caudal blocks provided by anesthesiologists immediately after general anesthesia or regional blocks with 0.5% bupivacaine (Marcaine) by surgeons just after the surgical procedures. The surgical techniques were performed as described previously,2 but with certain modifications since the last publication.
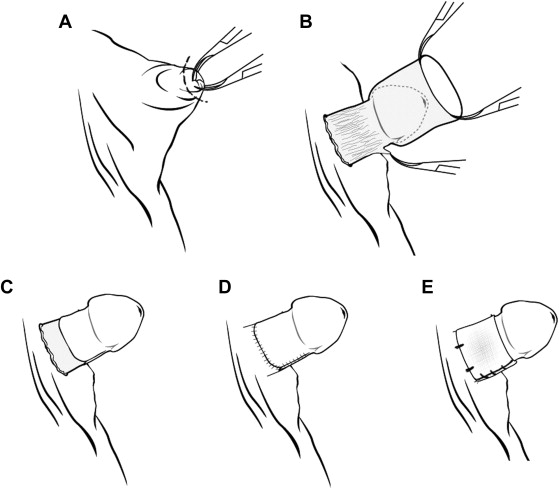
The procedure started with opening the phimosis by removing the narrow ring of the foreskin (Fig. 3A). Under adequate traction, the inner preputial skin was separated from its subcutaneous tissue and the outer skin. The dissection of the inner skin continued to the penile base. In most patients, detaching the fibrous tissues from Bucks fascia was necessary to release the trapped phallus (Figure 3 ; Figure 4). Some subcutaneous tissues between the inner and outer penile skin were removed to reduce edema after surgery. The inner penile skin might need tailoring to an adequate size prior to being fixed to the Bucks fascia of the proximal phallus (Fig. 3C). The outer skin was approximated to restore the skin covering of the penile shaft (Fig. 3D). We used chromic catgut as suture material in the first few years, but changed to 5-0 PDS (Ethicon) later to reduce tissue reaction. Compressive dressings with nonadhesive sterile gauze were applied at the end of surgery. In young patients, the dressings were sutured to the base of the penis for better fixation (Fig. 3E). Bladder catheterization was not necessary. Most patients were treated in day-care service. The patients were followed for 1 week, 1 month, and 2 months after surgery.
|
|
|
Figure 3. The procedures of the technique. (A) Circumferential incision to enlarge the narrow opening of the foreskin; (B) degloving the inner penile skin and the penile shaft, release of the fibrotic tissue attached to the Bucks fascia; (C) unfurling the inner penile skin; (D) restoration of skin coverage of the penile shaft; and (E) compressive dressing sutured to the base of penis.
|
|
|
|
Figure 4. Degloving and dissection down to the penile base, dividing the fibrotic tissue. The white arrow shows the fibrotic tissue attached to the Bucks fascia.
|
The surgical technique was similar in Group A and Group B. In Group A patients, more skin had to be preserved and skin closure was more difficult than in Group B. In Group B patients, some of the inner skin needed to be adequately tailored.
3. Results
The age distribution of the patients ranged from 2 months to 33 years. The mean age of the patients was 5.5 ± 4.9 years and the median age was 4.2 years. The initial symptoms of the patients are listed in Table 1. Although some patients had urinary symptoms, most of the patients were operated upon to correct the appearance of the genitalia. Symptoms of ballooning and urinary tract infections were more frequently seen in younger patients. The youngest patient in the series was operated at the age of 2 months. This infant had urinary tract infection and high grade vesicoureteral reflux. After correction of his buried penis, vesicoureteral reflux. resolved spontaneously 3 months later. Three adults, aged 22 years, 23 years, and 33 years, were operated upon for cosmetic purposes.
| Initial complaints | Number |
|---|---|
| Cosmetic reason (small phallus) | 110 |
| Ballooning of foreskin | 18 |
| Urine dripping | 13 |
| Dysuria | 10 |
| Balanoposthitis | 15 |
| Urinary tract infection | 5 |
| Not recorded | 10 |
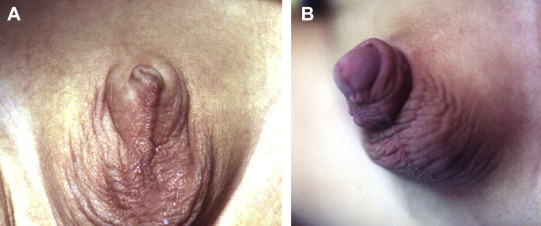
Most patients had satisfactory results (Fig. 5). All patients had their glanses exposed but there were various degrees of postoperative edema of the inner skin. The edema usually subsided within 1 month in most patients. One patient at the beginning of our series, however, had persisting edema after 6 months. The boy received a second operation to remove the edematous tissue.
|
|
|
Figure 5. Appearance of the penis (A) before and (B) 1 month after the operation.
|
Two patients (aged 3 years and 5 years) had postoperative wound infections, which were managed by removing some stitches, followed by wound care and antibiotics for 5 days. Their wounds recovered without the need of further surgery.
4. Discussion
It is not uncommon for pediatric surgeons or urologists to see parents who worried about the small appearance of their boys' penises. In most of these boys, the penises are normal in size by palpation. Several conditions have been described that result in small appearance of the penis, with inconspicuous penis,3 buried penis, hidden penis,4 concealed penis, trapped penis, and other terms being used to describe the various causes of the problem.5 Various classifications have also been developed.6 A few published reports have combined the results of correcting different types of anomalies.7 In this report, we focused on the problem of buried penis with insufficient penile skin only.
Buried penis is a congenital condition resulting from abnormal penile skin, and sometimes worsened by excessive suprapubic fat. This condition is associated with insufficient outer penile skin, inadequate fixation of the skin to the Bucks fascia, resulting in tenting and phimosis with trapping of the penis within the prepubic tissues. We noticed all Group A and most of the Group B patients had more or less chordee-like tissue attached to the Bucks fascia. After detaching this tissue, the trapped phallus was released and lengthened in appearance. This procedure significantly corrects buried penis.
The severity of buried penis can be described by the ratio of the length of penile skin and the exact length of penile shaft (S/P ratio). These measurements facilitate a more objective way to record the severity of the patients' conditions. In our opinion, only the patients with S/P ratio ≤ 70% (Group A and Group B patients) are candidates for preputial unfurling. Buried penises with obesity (mainly Group C patients) should be managed in different ways, such as diet control or liposuction. As a result of the insufficiency of penile skin, circumcision was a contraindication, especially for those patients in our Group A.
We performed similar procedures for Group A and Group B patients. Given that Group A patients had a more severe deficiency of penile skin, more inner prepuce was preserved to cover the penile shaft. From our observation, postoperative edema was more common in these patients. In Group B patients, some inner skin could be removed to reduce edema.
Although some patients had urinary symptoms such as balanitis or urinary tract infection, most of them were asymptomatic, with the exception of unsatisfactory appearance. The indication of surgery may be controversial. A small penis is a source of psychological trauma, especially in older children and adults.8 Buried penis is also seen in adults9 with no evidence that it will resolve with age, therefore, early surgery may be justified, especially if the patients are symptomatic. Less postoperative pain was observed in younger patients, thus, we suggest the ideal age of correction is from 6 months to 2 years for patients with severe buried penis (Group A).
Postoperative edema is a frequent complication after the correction of buried penis. Some patients in our early experience had prolonged edema after surgery. We thus modified our techniques in several ways to minimize the complication. First, we remove a portion of subcutaneous tissue from the inner prepuce; this lymphatic-rich tissue causes persistent swelling after operation; second, if there is excessive inner skin, it has to be tailored; third, a tight stricture due to the cutaneous ring should be avoided after approximation of the skin; fourth, a compressive dressing helps to reduce postoperative edema.
In this paper, we describe our experience in the correction of buried penis. There were several shortcomings in this study. First, it was a retrospective study; second, we had limited information of the outcome of the patients without any correction; and third, the follow-up time was short.
References
- 1 P.K. Donahoe, M.A. Keating; Preputial unfurling to correct the buried penis; J Pediatr Surg, 21 (1986), pp. 1055–1057
- 2 T.W. Chin, C.S. Liu, C.F. Wei; A simple modified method to correct buried penis in boys; Chin Med J (Taipei), 65 (2002), pp. 422–425
- 3 P.S. Bergeson, R.J. Hopkin, R.B. Bailey, L.C. McGill, J.C. Piatt; The inconspicuous penis; Pediatrics, 92 (1993), pp. 794–799
- 4 S. Rivas, R. Romero, A. Parente, M. Fanjul, J.M. Angulo; Simplification of the surgical treatment of a hidden penis; Actas Urol Esp, 35 (2011), pp. 310–314
- 5 M. Maizels, M. Zaontz, J. Donovan, P.N. Bushnick, C.F.J. Firlit; Surgical correction of the buried penis: description of a classification system and a technique to correct the disorder; Urol, 136 (1986), pp. 268–271
- 6 A.J. Casale, S.D. Beck, M.P. Cain, M.C. Adams, R.C. Rink; Concealed penis in childhood: a spectrum of etiology and treatment; J Urol, 162 (1999), pp. 1165–1168
- 7 M. Abbas, A. Liard, F. Elbaz, B. Bachy; Outcome of surgical management of concealed penis; J Pediatr Urol, 3 (2007), pp. 490–494
- 8 G.J. Alter, R.M. Ehrlich; A new technique for correction of the hidden penis in children and adults; J Urol, 161 (1999), pp. 455–459
- 9 A.G. Warren, Z.M. Peled, L.J. Borud; Surgical correction of a buried penis focusing on the mons as an anatomic unit; J Plast Reconstr Aes, 62 (2009), pp. 388–392
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?