Summary
Aims
Taiwan implemented a comprehensive and universal National Health Insurance (NHI) program to cover all inhabitants. This study aimed to assess the medical utilization by liver cancer patients under the NHI.
Methods
This retrospective cross-sectional study used a sampled NHI research database, which contained 1 million beneficiaries. The claims of liver cancer patients in 2009 were analyzed. The other beneficiaries without liver cancer who used medical services in 2009 served as the control patients.
Results
Among the 2335 identified liver cancer patients, 2178 (93.3%) patients used outpatient services and 1193 (51.1%) patients used inpatient services. Liver cancer accounted for 1.8% of the NHI’s total cost. The cost per visit was United States dollars (US$)59.30 for outpatient care and US$2070.30 for inpatient care. The annual cost per patient was US$4746.60; US$1951.00 were for outpatient care and US$2795.60 for inpatient care. Patients who were female, in their 60s, had a lower income, and lived in southern Taiwan had a higher cost per patient (p < 0.0001). Fees for consultation, treatment, and medical supplies (57.3%) accounted for the highest portion of outpatient costs, followed by drug fees (30.0%) and diagnosis fees (11.2%). Ward fees accounted for the highest portion of inpatient costs (19.0%), followed by drug fees (18.7%) and X-ray fees (14.9%). Private hospitals were visited more frequently than public hospitals. The cost per visit and cost per patient with liver cancer were 206.0% and 666.8%, respectively, of the cost of the control patients.
Conclusion
The cost of liver cancer care is substantial and varies by sex, age, income, and geographic distribution. It is critical to reduce the incidence of liver cancer and identify cost-effective treatment strategies.
Keywords
Cancer ; Cost ; Health insurance ; Liver ; Utilization
Introduction
Liver cancer is a major cause of cancer mortality worldwide [1] . Its incidence is increasing in Western countries, largely because of infection by hepatitis B virus (HBV) and hepatitis C virus (HCV) [2] ; [3] ; [4] . The prognosis is often poor for patients with advanced symptomatic liver cancer. The burden of liver cancer has increased. However, studies of medical utilization by liver cancer patients are limited.
Taiwan is in a region of high incidence of liver cancer. Liver cancer is the second leading cause of death in Taiwan and caused 7809 deaths in 2007 [5] . The age standardized incidence of liver cancer is 28.1 cases per 100,000 people. Liver cancer accounted for 5.6% of deaths in the year 2007 in Taiwan. The National Health Insurance (NHI) is a comprehensive and universal health insurance program that has provided Western medicine and Chinese medicine since 1995 in Taiwan. More than 90% of Taiwanese inhabitants and medical institutes joined the NHI program. The National Health Insurance Research Database (NHIRD) provides claims and registration datasets for research. In this study, we used the NHIRD datasets to explore medical utilization and costs of liver cancer patients in Taiwan. The purpose of this study was to access the annual medical costs of liver cancer in Taiwan and to determine the factors that were correlated with the medical costs. The hypothesis of this study was that the medical costs would be correlated with demographic factors.
Methods
Data sources
This is a retrospective cross-sectional study using Longitudinal Health Insurance Database 2005 (LHID2005), which was obtained from the NHIRD. The LHID2005 contains all original claim data of 1 million beneficiaries enrolled in 2005 who were randomly sampled from the 2005 Registry for Beneficiaries of the NHIRD, which contained approximately 25.68 million individuals [6] . There was no significant difference in the distribution of age, gender, and insured amount between the patients in the LHID2005 and the original NHIRD. Claims of LHID2005 in 2009 were obtained for analysis. Until 2009, there were 985,628 patients who remained in this sample. The dropout rate was 1.44%. Therefore, this sample is very representative of the whole population. Data in the NHIRD that could be used to identify patients or care providers such as medical institutions and physicians were scrambled prior to being sent to the National Health Research Institutes for database construction and were further scrambled prior to being released to each researcher. All data were also de-identified. The study was approved by the Institutional Review Board of Cheng Hsin General Hospital in Taipei, Taiwan [CHGH-IRB-(298)].
Study sample
The patients of this study were identified from the LHIH2005 by diagnosis codes of liver cancer [International Classification of Diseases , 9th Revision, Clinical modification (ICD-9-CM) codes 155 and 155.0-155.2] such as malignant neoplasm of liver and intrahepatic bile ducts [20] . To obtain demographic information, claim data were linked with files of registry for beneficiaries by the beneficiaries’ IDs and birthdays. The other beneficiaries without liver cancer who had used inpatient or outpatient services in 2009 served as the control patients.
Study variables
Dependent variable: cost
In this study, only insurance-covered services were taken into account. All costs were direct medical costs and presented in United States dollars [US$; US$1 = New Taiwan dollars (NT$) $33.05, based on the average exchange rate in 2009]. The detailed medical expenses in this study include the medical benefit claims and copayments. The patients’ copayment does not include registration fees. The categories of “outpatient cost” and “inpatient cost” were based on the definition by the Bureau of Health Insurance.
Independent variable: age
The age categories were < 50 years, 50–59 years, 60–69 years, 70–79 years, and > 80 years.
Independent variable: income
Income was categorized as US$0, US$1–605, US$606–1210, and > US$1210. The calculation of income was based on the insured amount. Dependents were assumed to have no income.
Independent variable: insured region
Insured regions were divided into four regions, based on geographic distribution: northern Taiwan, central Taiwan, southern Taiwan, and eastern Taiwan and offshore islands. Northern Taiwan was defined as the region extending from Keelung to Miaoli, which included Yilan. Central Taiwan included Taichung, Changhua, and Nantou. Southern Taiwan included the regions extending from Yunglin to Pingtung. Eastern Taiwan and offshore islands included Hualien, Taitung, Penghu, Kinmen, and Mazu.
Independent variable: insured unit
Insured units were categorized by six groups, based on the definition of the Bureau of Health Insurance.
Statistical analysis
The database software ASIQ 12.5.7 (Sybase Inc, Dublin, CA, USA) was used for data linkage and processing. The data were analyzed using SPSS for Windows Version 17.0 (SPSS Inc., Chicago, IL, USA). The distribution and frequency of each category of variables were examined by the Kruskal–Wallis test or by one-way analysis of variance (ANOVA). A value of p < 0.05 was considered statistically significant.
Results
In 2009, 2335 patients with liver cancer were identified in this sample. A total of 2178 (93.3%) patients used outpatient services and 1193 (51.1%) patients used inpatient services. The control patients comprised 883,804 patients who had ever used inpatient or outpatient services in 2009.
Medical utilization
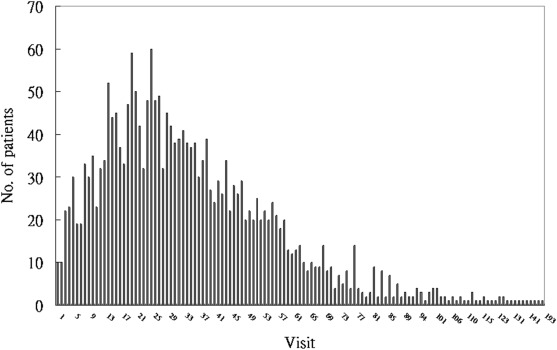
Among the patients, 2178 (93.3%) patients used outpatient services with 76,866 visits (average, 35.3 visits per user) and 1193 (51.1%) patients used inpatient services with 3153 visits (average 2.6 visits per user). The median frequency was 31 visits for outpatient users (Fig. 1 ) and two visits for inpatient users (Fig. 2 ).
|
|
|
Figure 1. Visit frequency of outpatient service use by liver cancer patients in 2009. |
|
|
|
Figure 2. The visit frequency of inpatient service use by liver cancer patients in 2009. |
The most frequently used outpatient service by visit was Western medicine (85.5%), followed by Chinese medicine (6.1%), dentistry (3.8%), emergent medicine (3.3%), and homecare (1.4%) (Table 1 ). The emergent services had the highest cost per visit of outpatient services. The most frequently used inpatient service by visits was ordinary care (94.0%), followed by other services (4.9%) and hospice care (0.7%) (Table 1 ). The hospice care had the lowest cost per visit of inpatient services.
| Characteristic | Visit | % | Cost (US$) | % | Cost per visit (US$) | |
|---|---|---|---|---|---|---|
| Outpatient | Chinese medicine | 4668 | 6.1 | 83,801 | 1.84 | 18.0 |
| Dentistry | 2889 | 3.8 | 89,886 | 1.97 | 31.1 | |
| Emergent medicine | 2515 | 3.3 | 406,824 | 8.93 | 161.8 | |
| Homecare | 1057 | 1.4 | 25,341 | 0.56 | 24.0 | |
| Western medicine | 65,737 | 85.5 | 3,949,824 | 86.70 | 60.1 | |
| Total | 76,866 | 100.0 | 4,555,675 | 100 | 59.3 | |
| Inpatient | Ordinary care | 2963 | 94.0 | 5,539,034 | 84.9 | 1869.4 |
| Hospice care | 23 | 0.7 | 14,546 | 0.2 | 632.4 | |
| Other servicesa | 167 | 4.9 | 974,074 | 14.9 | 5832.8 | |
| Total | 3153 | 100 | 6,527,655 | 100.0 | 2070.3 | |
a. The data include case payment, special case (cost > NT$500,000.00; vascular stent or transplantation), payment demonstration program for breast cancer and hepatitis, tuberculosis program, and diet fees for low-income householders.
Medical cost for liver cancer patients and control patients
The cost for liver cancer patients and the control patients is presented in Table 2 . For liver cancer patients, the cost per visit was US$59.30 for outpatient services and US$2070.30 for inpatient services. The cost per user was US$2091.70 for outpatient services and US$5471.6 for inpatient services. The cost per patient was US$4746.60 with US$1951.00 used for outpatient services and US$2795.60 used for inpatient services.
| Characteristic | Control patients a | Liver cancer patients | % | |
|---|---|---|---|---|
| No. of patients | Total | 881,469 | 2335 | 0.3 |
| Outpatient | 880,745 | 2178 | 0.2 | |
| Inpatient | 74,629 | 1193 | 1.6 | |
| No. of visits | Outpatient | 14,668,653 | 76,866 | 0.5 |
| Inpatient | 128,426 | 3153 | 2.5 | |
| Total cost (US$) | Total | 627,506,394 | 11,083,329 | 1.8 |
| Outpatient | 421,993,697 | 4,555,675 | 1.1 | |
| Inpatient | 205,512,697 | 6,527,655 | 3.2 | |
| Cost per visit (US$) | Outpatient | 28.8 | 59.3 | 206.0 |
| Inpatient | 1600.2 | 2070.3 | 129.4 | |
| Average cost per user (US$) b | Outpatient | 479.1 | 2091.7 | 436.6 |
| Inpatient | 2753.8 | 5471.6 | 198.7 | |
| Cost per patient (US$) c | Total | 711.9 | 4746.6 | 666.8 |
| Outpatient | 478.7 | 1951.0 | 407.5 | |
| Inpatient | 233.1 | 2795.6 | 1199.1 | |
a. All patients who ever used outpatient or inpatients services in this sample database.
b. Outpatient cost divided by outpatient service users; inpatient cost divided by the number of inpatient service users.
c. The cost divided by the number of all liver cancer patients or control participants.
Liver cancer accounted for 1.8% of the total costs, 1.1% of outpatient costs, and 3.2% of inpatient costs of the NHI. The average medical cost for liver cancer patients was higher than that of the control patients. The average costs per visit of the liver cancer patients was 206.0% of that of the control patients. The average cost per patient with liver cancer was 666.8% that of the control patients.
Cost component and service provider
Private hospitals were visited more frequently than public hospitals for outpatient and inpatient services (Table 3 ). The cost per visit was highest in public hospitals for outpatient services and highest in private hospitals for inpatient services. Fees for consultation, treatment, and medical supplies accounted for the highest portion of outpatient costs (57.3%), followed by drug fees (30.0%), and diagnosis fees (11.2%). Ward fees accounted for the highest portion of inpatient cost (19.0%), followed by drug fees (18.7%), and X-ray fees (14.9%).
| Characteristic | Public hospitals | Private hospitals | Public clinics | Private clinics | Nursing institutions | Total | % | ||
|---|---|---|---|---|---|---|---|---|---|
| Outpatient | Visit | 16,198 | 31,173 | 1313 | 28,088 | 94 | 76,866 | ||
| Cost (US$) | Drug fees | 473,050 | 805,676 | 10,340 | 76,427 | 199 | 1,365,692 | 30.0 | |
| Consultation, treatment, and medical supplies | 706,417 | 1,410,737 | 4295 | 480,414 | 6495 | 2,608,359 | 57.3 | ||
| Diagnosis fees | 102,246 | 192,992 | 9166 | 203,856 | 61 | 508,322 | 11.2 | ||
| Dispensing service fees | 20,871 | 39,484 | 912 | 12,032 | 4 | 73,303 | 1.6 | ||
| Total | 1,302,584 | 2,448,889 | 24,714 | 772,729 | 6758 | 4,555,675 | 100.0 | ||
| Average cost per visit | 80.4 | 78.6 | 18.8 | 27.5 | 71.9 | 59.3 | |||
| Inpatient | Visit | 1075 | 2078 | 3153 | |||||
| Cost (US$) | Diagnosis fees | 118,076 | 237,067 | 355,143 | 5.4 | ||||
| Ward fees | 406,677 | 832,322 | 1,238,999 | 19.0 | |||||
| Tube feeding fees | 9991 | 24,333 | 34,324 | 0.5 | |||||
| Laboratory fees | 234,987 | 445,798 | 680,785 | 10.4 | |||||
| X-ray fees | 307,755 | 665,261 | 973,017 | 14.9 | |||||
| Therapeutic procedure fees | 114,646 | 256,952 | 371,597 | 5.7 | |||||
| Surgical fees | 99,382 | 279,293 | 378,675 | 5.8 | |||||
| Rehabilitation fees | 5520 | 7160 | 12,679 | 0.2 | |||||
| Hemodialysis fees | 27,577 | 41,042 | 68,619 | 1.1 | |||||
| Blood/plasma fees | 112,569 | 245,457 | 358,027 | 5.5 | |||||
| Anesthesia fees | 39,321 | 78,105 | 117,426 | 1.8 | |||||
| Special materials fees | 157,023 | 418,265 | 575,289 | 8.8 | |||||
| Drug fees | 336,760 | 885,711 | 1,222,471 | 18.7 | |||||
| Dispensing service fees | 30,500 | 58,682 | 89,182 | 1.4 | |||||
| Psychiatric treatment fees | 1752 | 3594 | 5347 | 0.1 | |||||
| Injection technology fees | 14,847 | 31,227 | 46,074 | 0.7 | |||||
| Total | 2,017,384 | 4,510,271 | 6,527,655 | 100.0 | |||||
| Average cost per visit (US$) | 1876.6 | 2170.5 | 2070.3 | ||||||
Demographics
The correlation between cost and demographic characteristics is presented in Table 4 . A greater proportion of liver cancer patients was male, in their 50s, earned a monthly middle income (US$606.00–1210.00), lived in northern Taiwan, or were dependents. Patients had a higher cost per patient if they were female, in their 60s, earned no income (by insured amount), lived in southern Taiwan, and lived in low-income households (by insured unit) (p < 0.0001). The correlation between cost and age was further analyzed ( Table 5 ). The patients in their 60s had a higher cost per visit for outpatient and inpatient services.
| Characteristics | No. of patients a | % | Average cost per patient (US$) | pb | ||
|---|---|---|---|---|---|---|
| Outpatient | Inpatient | Total | ||||
| Gender | < 0.0001 | |||||
| Female | 818 | 35.1 | 1964 | 3031 | 4995 | |
| Male | 1515 | 64.9 | 1930 | 2367 | 4298 | |
| Age (y) | < 0.0001 | |||||
| < 50 | 425 | 18.2 | 1322 | 1682 | 3003 | |
| 50s | 575 | 24.6 | 1995 | 3111 | 5105 | |
| 60s | 563 | 24.1 | 2223 | 3332 | 5555 | |
| 70s | 543 | 23.3 | 2199 | 2725 | 4924 | |
| > 80 | 227 | 9.7 | 1764 | 2946 | 4710 | |
| Income (US$/mo) c | < 0.0001 | |||||
| 0 | 665 | 28.5 | 2301 | 2670 | 4972 | |
| 1–605 | 419 | 18.0 | 1869 | 2917 | 4786 | |
| 606–1210 | 991 | 42.5 | 1874 | 2926 | 4800 | |
| > 1210 | 258 | 11.1 | 1489 | 2443 | 3932 | |
| Insured region | < 0.0001 | |||||
| Northern Taiwan | 1057 | 45.3 | 1631 | 2365 | 3996 | |
| Central Taiwan | 358 | 15.3 | 2521 | 2681 | 5201 | |
| Southern Taiwan | 846 | 36.3 | 2127 | 3442 | 5569 | |
| Eastern Taiwan and offshore islands | 72 | 3.1 | 1791 | 2171 | 3962 | |
| Insured unit | < 0.0001 | |||||
| Employees of government, schools, enterprises, or institutions | 423 | 18.1 | 1442 | 2492 | 3934 | |
| Members of occupational unions and alien seamen | 345 | 14.8 | 1907 | 3114 | 5020 | |
| Farmers and fishermen | 534 | 22.9 | 1975 | 2853 | 4828 | |
| Low-income households | 30 | 1.3 | 1722 | 3892 | 5614 | |
| Veterans and other regional population | 336 | 14.4 | 1934 | 2927 | 4861 | |
| Dependents | 665 | 28.5 | 2301 | 2670 | 4972 | |
a. Two patients with missing demographic data were excluded.
b. The p value of the total cost, based on the Kruskal–Wallis test.
c. The calculation of income was based on the insured amount. Dependents were assumed to have no income.
| Variable | < 50 y | 50–59 y | 60–69 y | 70–79 y | > 80 y | pa | |
|---|---|---|---|---|---|---|---|
| Outpatient | No. of patients | 425 | 575 | 563 | 543 | 227 | |
| Visits | 10,971 | 167,39 | 20,844 | 20,917 | 7359 | ||
| Average visit per patient | 25.8 | 29.1 | 37.0 | 38.5 | 32.4 | ||
| Drug fees | 402 | 576 | 737 | 627 | 476 | 0.0146 | |
| Consultation, treatment and medical supplies | 722 | 1203 | 1210 | 1279 | 1027 | 0.0109 | |
| Diagnosis fees | 177 | 190 | 240 | 253 | 226 | 0.0000 | |
| Dispensing service fees | 20 | 26 | 35 | 40 | 35 | 0.0000 | |
| Total | 1322 | 1995 | 2223 | 2199 | 1764 | 0.0001 | |
| Inpatient | No. of patients | 425 | 575 | 563 | 543 | 227 | |
| Visits | 402 | 755 | 832 | 801 | 363 | ||
| Average visit per patient | 0.9 | 1.3 | 1.5 | 1.5 | 1.6 | ||
| Diagnosis fees | 98 | 148 | 174 | 158 | 198 | 0.0000 | |
| Ward fees | 318 | 506 | 611 | 564 | 715 | 0.0000 | |
| Tube feeding fees | 4 | 8 | 16 | 20 | 34 | 0.0016 | |
| Laboratory fees | 173 | 306 | 337 | 299 | 350 | 0.0001 | |
| X-ray fees | 275 | 453 | 482 | 445 | 365 | 0.0017 | |
| Therapeutic procedure fees | 76 | 140 | 195 | 163 | 264 | 0.0009 | |
| Surgical fees | 119 | 242 | 198 | 114 | 68 | 0.0035 | |
| Rehabilitation fees | 1 | 2 | 14 | 3 | 6 | 0.2540 | |
| Hemodialysis fees | 7 | 27 | 44 | 39 | 19 | 0.6229 | |
| Blood/plasma fees | 87 | 190 | 200 | 124 | 138 | 0.0120 | |
| Anesthesia fees | 43 | 63 | 60 | 41 | 29 | 0.0252 | |
| Special materials fees | 137 | 240 | 302 | 293 | 218 | 0.0000 | |
| Drug fees | 294 | 724 | 631 | 404 | 469 | 0.0279 | |
| Dispensing service fees | 27 | 39 | 43 | 38 | 47 | 0.0016 | |
| Psychiatric treatment fees | 8 | 3 | 0 | 0 | 0 | 0.0696 | |
| Injection technology fees | 13 | 20 | 23 | 19 | 26 | 0.0648 | |
| Total | 1682 | 3111 | 3332 | 2725 | 2946 | 0.0003 | |
a. Based on the one-way analysis of variance (ANOVA) test.
Discussion
Liver cancer is the third leading cause of cancer-related deaths in the world [1] . However, information on the economic burden of liver cancer is limited. This study is the first to evaluate the annual medical costs of liver cancer in Taiwan. Our data can serve as an important reference for health care providers and policymakers. Using the NHI data, our study assessed the medical utilization and costs of liver cancer patients who used medical services in 2009. The NHI in Taiwan is a comprehensive and universal health insurance program, which has provided Western medicine, Chinese medicine, dental care, and hospital care since 1995. Until 2009, the NHI covered more than 99% of residents and 92% of medical institutions in Taiwan. Therefore, the claim and registration datasets of the NHI are an ideal tool to investigate the utilization of medical services of the studied population.
In this study, we used sample datasets containing 1 million NHI beneficiaries. A total of 2335 liver cancer patients were identified. All claims of liver cancer patients were collected for analysis. Therefore, the study results were representative.
This study found that liver cancer patients accounted for 0.3% of medical service users, 0.2% of outpatient service users, and 1.6% of inpatient service users. However, liver cancer accounted for 1.8% of the total medical costs, 1.1% of outpatient costs, and 3.2% of inpatient costs for all beneficiaries. The average medical costs were higher for liver cancer patients than for the control patients. Liver cancer patients used more medical resources. Since 1984, there has been a successful universal vaccination plan for HBV for newborns in Taiwan. The average incidence of liver cancer per 100,000 children decreased from 0.7 in 1981–1986 to 0.36 in 1990–1994 in children 6–14 years old. However, the lower incidence of liver cancer in adults will be effected after 3–4 decades [7] ; [8] . Liver cancer remains a heavy burden on the health system in Taiwan. Therefore, the development of cost-effective treatment strategies for liver cancer is critical to reduce the financial burden in Taiwan.
It is difficult to compare the cost in different studies because of heterogeneity across studies in the settings, populations studied, measurement of costs, and study methods. Lang et al [9] conducted a claim data analysis from a medical center in Taiwan and found that the 10-year lifetime average cost of patients with liver cancer was NT$418,554.00 [New Taiwan dollars (NT$) = US $12,683.00]. The Huang study [10] used the NHI data from 1996 to 2002 with ICD-9 code 155. For all incident cases of liver cancer in 1997, the average 5-year cumulated cost was NT$219,398.00 (US $6648.00).
The prognosis of liver cancer is poor. The 1-year and 5-year overall survival rate of liver cancer in Taiwan is 48.98% and 19.72%, respectively [11] . In this study, the average cost per patient was US$4746.60 in 2009. Lang et al [12] found the overall per patient cost of liver cancer was US$32,907.00 in the United States of America (USA) with US$29,354.00 spent on health care cost and US$3553.00 spent on the value of lost productivity. Our study found that the annual overall per patient cost of liver cancer was US$4746.60 in Taiwan. The per patient monthly cost was US$7845.00 in the USA and US$395.60 in Taiwan. The cost of liver cancer is much lower in Taiwan than in the USA; however, the 5-year survival rate of liver cancer is better in Taiwan than in the USA [11] ; [13] . Taiwan’s medical system provided efficiency and quality medical services. Taiwans NHI system has attracted attention from around the world for its many achievements such as its universality, ability to care for socially and economically disadvantaged groups, and a wide range of coverage and consistent level of quality. Physician visits per person per year was 13.9 in Taiwan, 3.8 in the USA, 7.5 in Germany, and five in the United Kingdom [14] . The average life expectancy and infant mortality rate in Taiwan were compatible with those in Economic Co-operation and Development (OECD) countries. The utilization of medical services increased, although the health expenditure remained at 6.1% of the gross domestic product (GDP) in Taiwan [14] . This finding is in sharp contrast with the USA (16% of the GDP) and lower than that of most OECD countries [15] .
The correlation was analyzed between cost and medical utilization, demographics, and service providers. The most frequently used outpatient services by visits was Western medicine (85.5%), followed by Chinese medicine (6.1%). Our previous study [16] in 2007 found that 3.9% patients with liver cancer (with diagnosis codes 155 and 155.0) used cancer-related outpatient services of Chinese medicine (CM) at least once. Chinese medicine accounted for 2.6% visits and 0.7% expenditure of ambulatory services for liver cancer. Western medicine is the mainstream. In liver cancer care, CM has more a complementary role than an alternative role. Our results also demonstrated that hospice care had the lowest average cost per inpatient service visit. This is consistent with a previous study in Taiwan [17] .
Our study demonstrated that the cost of liver cancer care to the NHI varied by sex, age, income, and geographic distribution. A higher proportion of liver cancer patients were male, in their 50s, earned a monthly middle income (US$606–US$1210), and lived in northern Taiwan, or were dependents. However, patients who were female, in their 60s, earned no income (by the insured amount), lived in southern Taiwan, or were from low-income households (by insured unit) had a higher average cost per patient (p < 0.0001). The role of HBV and HCV in liver cancer in Taiwan differs in different age groups. Hepatitis B virus was more frequent in young liver cancer patients, and HCV was more frequent in elderly liver cancer patients in Taiwan [18] . Chen et al [19] found that HCV infection was very common in some villages and townships in southern Taiwan [19] . Our study also found that patients in their 60s had a higher cost per visit for outpatient and inpatient services.
Several limitations of this study must be acknowledged. (1) This is a claim-based study; only insurance-covered services and medications were taken into account. Out-of-pocket herbal medicine and noncontracted medical institutes were not included. This may underestimate the cost. (2) The cost was the points that the contracted medical institutions declared and was not corrected for the point value by global budget payment and deduction by NHI. The NHI paid medical fees to health care providers on a fee-for-service basis. The global budget payment scheme was promoted from dental services to CM, followed by Western medicine primary care, and finally hospitals. The system was universally implemented in all medical care institutions by July 2002. The point value by global budget payment system is floating. In 2009, one point value was equal to NT$0.8872–1.0002. Furthermore, the service costs to be deducted by NHI were not adjusted. Adjusting the point value and deduction would decrease the cost by approximately 10%. (3) The study population was selected by the diagnosis codes. The number of liver cancer patients may be overestimated because of overcoding. (4) The NHIRD is primarily for administrative purposes. The clinical characteristics such as staging and biochemical data were unavailable. The disease severity and survival could not be evaluated in this study. The cost effectiveness could not be analyzed. (5) This study included all medical services for analysis, regardless of their relevance to the liver cancers. Among the services that liver cancer patients utilized, some services were not relevant to the liver cancer. Some services were relevant to the liver cancer. Some services were not directly relevant to the liver cancers, but may be contributed to or accounted for by the disease. This may overestimate the cost.
This study was designed to explore the economic burden of liver cancer in Taiwan. The methods of treatment, disease severity, and type of hospital influence the differences in the health care costs between patients or between geographical regions. In a cross-sectional study, this sample is not well reflective of the whole course of liver cancer. Therefore, the aforementioned factors were not analyzed. In the future, a longitudinal study is warranted to explore these important factors.
In conclusion, liver cancer is a heavy burden on the health service system in Taiwan. Liver cancer patients used more medical resources than the other people. The cost of liver cancer care is substantial and varies by sex, age, income, and geographic distribution. Based on the findings of the study, it is critical to reduce the incidence of liver cancer and identify cost-effective treatment strategies.
Conflicts of interest
All authors declare no conflicts of interest.
Acknowledgments
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, the Department of Health, and managed by the National Health Research Institutes. The interpretations and conclusions contained in this paper do not represent those of the Bureau of National Health Insurance, Department of Health, or National Health Research Institutes. This work was supported by Cheng Hsin General Hospital in Taipei, Taiwan (grant number 102-35 ).
References
- [1] D.M. Parkin, F. Bray, J. Ferlay, P. Pisani; Global cancer statistics, 2002; CA Cancer J Clin, 55 (2005), pp. 74–108
- [2] A.S. Lok, L.B. Seeff, T.R. Morgan, A.M. di Bisceglie, R.K. Sterling, T.M. Curto, HALT-C Trial Group, et al.; Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advanced liver disease; Gastroenterology, 136 (2009), pp. 138–148
- [3] K.A. McGlynn, R.E. Tarone, H.B. El-Serag; A comparison of trends in the incidence of hepatocellular carcinoma and intrahepatic cholangiocarcinoma in the United States; Cancer Epidemiol Biomarkers Prev, 15 (2006), pp. 1198–1203
- [4] S.F. Altekruse, K.A. McGlynn, M.E. Reichman; Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005; J Clin Oncol, 27 (2009), pp. 1485–1491
- [5] Bureau of Health Promotion. Department of Health; 2009 Annual report; Bureau of Health Promotion, Taipei, Taiwan (2009)
- [6] National Health Insurance Research Database (2014) Available at: http://nhird.nhri.org.tw/en/index.htm [accessed 09.02.14]
- [7] J.H. Kao, D.S. Chen; Global control of hepatitis B virus infection; Lancet Infect Dis, 2 (2002), pp. 395–403
- [8] J.H. Kao, D.S. Chen; Changing disease burden of hepatocellular carcinoma in the Far East and Southeast Asia; Liver Int, 25 (2005), pp. 696–703
- [9] H.C. Lang, J.C. Wu, S.H. Yen, C.F. Lan, S.L. Wu; The lifetime cost of hepatocellular carcinoma: a claims data analysis from a medical centre in Taiwan; Appl Health Econ Health Policy, 6 (2008), pp. 55–65
- [10] C.F. Huang; Medical cost and treatment outcome related factors for HCC; Institute of Health Care Management, National Sun Yat-sen University, Kaohsiung (2005), p. 97
- [11] Bureau of Health Promotion. Department of Health. Executive Yuan; Cancer registry annual report, 2007; Bureau of Health Promotion, Taipei, Taiwan (2010)
- [12] K. Lang, N. Danchenko, K. Gondek, S. Shah, D. Thompson; The burden of illness associated with hepatocellular carcinoma in the United States; J Hepatol, 50 (2009), pp. 89–99
- [13] A. Jemal, R. Siegel, E. Ward, Y. Hao, J. Xu, T. Murray, et al.; Cancer statistics, 2008; CA Cancer J Clin, 58 (2008), pp. 71–96
- [14] Bureau of National Health Insurance; National Health Insurance in Taiwan 2010; Bureau of Health Promotion, Taipei, Taiwan (2010)
- [15] Organisation for Economic Co-operation and Development (OECD); OECD health data 2009 – Statistics and indicators for 30 countries ; OECD, Paris, France (2009)
- [16] Y.H. Lin, J.H. Chiu; Use of Chinese medicine among patients with liver cancer in Taiwan; J Altern Complement Med (New York, NY), 16 (2010), pp. 527–528
- [17] W.Y. Lin, T.Y. Chiu, H.S. Hsu, L.E. Davidson, T. Lin, K.C. Cheng, et al.; Medical expenditure and family satisfaction between hospice and general care in terminal cancer patients in Taiwan; J Formos Med Assoc [Taiwan Yi Zhi], 108 (2009), pp. 794–802
- [18] D.S. Chen; Hepatocellular carcinoma in Taiwan; Hepatol Res, 37 (Suppl. 2) (2007), pp. S101–S105
- [19] D.S. Chen; Viral hepatitis in East Asia; J Formos Med Assoc [Taiwan Yi Zhi], 95 (1996), pp. 6–12
- [20] U.S. Centers for Disease Control and Prevention; International classification of diseases, ninth revision, clinical modification (ICD-9-CM); (2014) Available at: http://www.cdc.gov/nchs/icd/icd9cm.htm [accessed 09.02.14]
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?