Summary
Background
The minimal right vertical infra-axillary thoracotomy could be a safe and cosmetic alternative to standard median sternotomy. This study reviews our results and experience with a minimal right vertical infra-axillary thoracotomy technique for the repair of atrial septal defects compared with standard median sternotomy.
Methods
The study was designed as a retrospective, observational, and case-controlled study. Between May 2007 and November 2012, 26 patients underwent atrial septal defect closure with standard median sternotomy (Group 1). This group was compared with 21 patients who underwent repair of atrial septal defects using minimal right vertical infra-axillary thoracotomy (Group 2). Quantitative data were given as mean ± standard deviation, and qualitative values were expressed as percentages. In the comparison of the normal variables between the two groups, we used independent sample t test, and in the comparison of categorical variables between groups, Chi-square test was used.
Results
The mean length of incision was significantly shorter in Group 2 than in Group 1 (p = 0.03). The time it took to establish cardiopulmonary bypass was longer in Group 2 (p = 0.04). There were no statistically significant differences in cardiopulmonary bypass time (p = 0.11), aortic cross-clamp time (p = 0.10), and total operation time (p = 0.10) between the two groups. Group 2 had less chest tube drainage (p = 0.04), less blood transfusion (p = 0.02), and shorter postoperative mechanical ventilation time (p = 0.09) than Group 1.
Conclusion
Minimal right vertical infra-axillary thoracotomy can be performed with favorable cosmetic and clinical results for atrial septal defects closure. Infra-axillary thoracotomy provides a good alternative to standard median sternotomy for patients with atrial septal defects.
Keywords
atrial septal defect;repair sternotomy;thoracotomy
1. Introduction
Surgical repair of atrial septal defects (ASDs) has been applied with excellent outcomes by many surgeons using standard median sternotomy (SMS) from the beginning of heart surgery until today.1 The mortality and morbidity rate in repair of ASDs with SMS procedure is 0%. Despite its cost, developments in interventional cardiology made the repair of ASDs with transcatheterization a great alternative to surgery because of its perfect cosmetic outcomes and the fact that it is minimally invasive.2 Concurrent developments in surgery and interventional cardiology techniques provide perfect repair results, early return to normal daily activity, and a physically and psychologically high-quality life. However, ASD repair with transcatheter is an alternative to surgery in anatomically suitable defects. Successful ASD repair using SMS was first performed in 1952 by Lewis and Varco.1 Nowadays, because of the SMS-related cosmetics and some psychological results connected to it, in young women and child patients, for ASD closure, one of such minimal invasive procedures as ministernotomy,3 right anterior thoracotomy,4 right anterolateral thoracotomy,5 or posterior thoracotomy6 is preferred. In recent years, minimal right vertical infra-axillar thoracotomy (RVIAT), which is a minimally invasive and aesthetic technique, has become usable for ASD repair. RVIAT is a modification of the original Denis Browne technique. The original Denis Browne technique was applied in 1952 by Denis Browne7 to eliminate n. longus thoracicus injury in standard left thoracotomy used in the repair of patent ductus arteriousus. In this technique, in the left midaxillary line, m. latissimus dorsi is protected, and n. thoracicus longus is separated from m. serratus anterior to prevent damage. The first use of this technique in open-heart surgery was started as a right thoracic procedure in 2001 by Yang et al.8 ; 9 The purpose of our study is to compare SMS with the clinical results of RVIAT performed in ASD and partial atrioventricular septal defect (AVSD) closure for the first time in our clinic in Turkey.
2. Patients and methods
2.1. Study setting and design
This retrospective study included 47 ASD patients who underwent operation in our clinic between May 2007 and November 2012. The patients were divided into two groups according to the surgical incision and technique used. The 26 patients who underwent SMS were designated as Group 1, and 21 patients who underwent minimal RVIAT were designated as Group 2.
The trial was approved by the Institutional Ethics Committee of our center and University of Cukurova was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients or their parents or legal guardians.
2.1.1. Patients
Prior to undergoing either sternotomy or minimal RVIAT, the patients with ASD or partial AVSD were made aware of the differences between the two procedures.
2.1.2. Study evaluations
The patients who had a cardiac anomaly, had persistent left superior vena cava, required dilatation for right ventricular outflow tract, had right pleural adhesion, had a body mass index >30 kg/m2, or those whose families preferred SMS were excluded from the study. Average incision length, cardiopulmonary bypass (CBP)’s setup time, CPB time, aortic cross-clamp (ACC) time, total operating time, mechanical ventilation time, chest tube drainage volume, the amount of blood transfusion, hospital stay, time to return to normal daily activity, pain after the operation, postoperative mortality rate, and residual shunt ratio variables were analyzed and recorded (Table 1). The assessment of pain was made according to the Universal Pain Assessment Tool (pain is scored on a 0–10 scale, where 0 represents no pain and 10 is the worst imaginable pain).
| Variables | SMS (n = 26) | Minimal RVIAT (n = 21) | p∗ |
|---|---|---|---|
| Incision length (cm) | 15.1 ± 2.1 | 6.1 ± 1.1 | 0.03 |
| CPB setup length (min) | 24.3 ± 3.4 | 40.1 ± 6.2 | 0.04 |
| CPB time (min) | 32.6 ± 5.1 | 34.1 ± 4.6 | 0.11 |
| ACC time (min) | 25 ± 4.8 | 26.3 ± 3.2 | 0.10 |
| Total operation time (min) | 116.1 ± 6.5 | 110.4 ± 5.3 | 0.10 |
| Mechanical ventilation time (h) | 3.5 ± 2.1 | 2.4 ± 1.2 | 0.044 |
| The amount of chest tube drainage in postoperative period (mL/m2) | 150 ± 50 | 100 ± 25 | 0.04 |
| The amount of blood transfusion (mL) | 250 ± 50 | – | – |
| Hospital stay (d) | 7.1 ± 1.6 | 4 ± 1.4 | 0.03 |
| Time of stay in intensive care unit (h) Postoperative normal daily activity time (h) Universal Pain Assessment Tool | 48.2 ± 2.1 16.4 ± 1.7 2–3 | 24.8 ± 6.2 9.5 ± 2.6 2–5 | 0.025 0.035 0.07 |
| Residual shunt (%) | – | – | |
| Mortality (%) | – | – |
Continuous variables are presented as mean ± SD.
ACC = aortic cross-clamp; CPB = cardiopulmonary bypass; SD = standard deviation.
∗. Independent samples described as t test and Chi-square test; statistical significance is described as p < 0.05.
2.1.3. Anesthetic technique
Prior to the surgery, all phenomena were examined preoperatively. The same anesthetic technique was used in all patients who were taken to the operating room without premedication and according to a suitable fasting period for each age. After ketamine bolus (2 mg/kg, i.v.) was administered in anesthesia induction, vecuronium bromide (0.1 mg/kg) was administered as a muscle relaxant. When the muscle relaxation was adequate (after about 3 minutes), tracheal intubation was performed. Anesthesia maintenance was provided with sevoflurane (0.5–2%).
2.2. Surgical technique
2.2.1. Minimal RVIAT
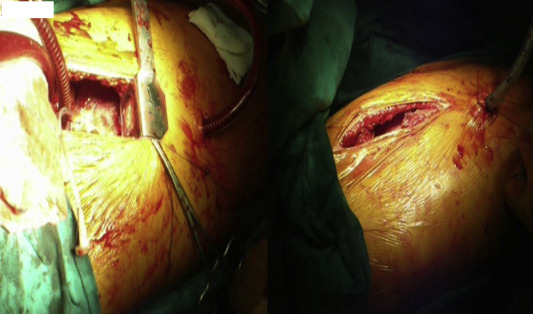
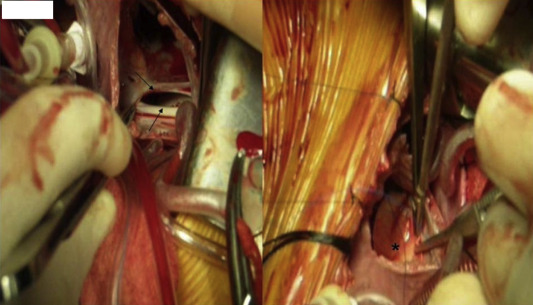
Preoperative anterior–posterior and lateral chest positions and the location of the shadow of the heart in the chest X-ray were carefully examined to enable the choice between the third and the fourth intercostal space, from which the heart could be easily accessed and the thorax could be handled. The atrial shadows' relationship with the ribs was used as a guide. The patient was canted to the right at an angle of 60°. The right arm was placed on the head with a 120° abduction from the shoulder. Skin incision was started from the third intercostal space in the midaxillary line and applied until the fifth intercostal space. The length of the skin incision is approximately 5–7 cm, but this can be adjusted according to the patients weight and height. The right thoracic cavity was accessed from the third or fourth intercostal space. The right lung was pushed back with a wet sponge and a malleable retractor. The pericardium was opened from 2 cm in front of the phrenic nerve. Then, it was hanged with sling sutures from the top-middle and bottom parts so the ascendan aorta and vena cava inferior can be viewed more easily. Standard purse sutures were placed in the right side of the ascendan aorta, the superior vena cava, and the right atriocaval junction. After heparinization, the aorta was cannulated with the help of two long vascular clamps. One of the clamps was placed on the lower section of the ascending aorta for pulling down and stabilization of the aorta. After this, the top of the aortic cannula was held using the other clamp, and with the aid of this clamp the aortic cannula was placed. If the inferior vena cava cannula moves on the small thoracotomy incision area, it can create difficulties in manipulations as the operation progresses. To prevent this from happening, a 2-cm skin incision was made in the anterior axillary line on the seventh intercostal space level and the vena cava cannula was passed from here, and cannulation was done (Fig. 1). Thus, a better exposure was provided in the surgical field during the operation, and the place from where the cannula passed was used as the thorax drain place after the surgery. After bicaval cannulations, CPB was started. As a standard, a cross-clamp was placed on the ascending aorta, and adequate myocardial protection was achieved by isothermal blood cardioplegia. Moderate hypothermia (32 °C) was provided, and a vent cannula was placed in the left superior pulmonary vein. Whereas the defects were closed with bovine pericardium patches in 18 of the patients (Fig. 2), in three other patients they were closed with primary suturation using 5–0 polypropylene. After CPB, the pericardium was closed partially. The thorax was closed after the placement of a single thorax tube to the right thorax.
|
|
|
Figure 1. In patients who had right vertical infra-axillar thoracotomy (RVIAT), inferior vena cava cannula passed from the seventh intercostal range and, at the end of the operation, thoracic drain is placed from the same range. |
|
|
|
Figure 2. Atrial septal defect (arrows) and the defect that will be closed with a patch (*). |
2.2.2. SMS
In Group 1 (patients who underwent SMS), the standard surgical technique was performed. In this group, the defects were closed with bovine pericardium patches in 17 patients, whereas in nine of them the defects were closed with 5–0 polypropylene primary sutures.
2.3. Follow-up
All patients were followed up by physical examination and transthoracic echocardiography. The average follow-up period was 27.6 ± 10.8 (range, 8–49) months.
2.4. Statistical analysis
SPSS for Windows version 12.0 pocket program (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Quantitative data were given as mean ± standard deviation. Qualitative values were expressed as percentages. In the comparison of normal variables between the two groups, we used the independent sample t test; in the comparison of categorical variables between groups, the Chi-square test was used. All tests were mutual, and p < 0.05 was considered statistically significant.
3. Results
3.1. Study populations
The preoperative demographic and diagnostic data of the study groups are detailed in Table 2. There were 11 (42.3%) males and 15 (57.7%) females, with a mean age of 21.2 ± 10.1 years, in the SMS group. There were eight (38.1%) males and 13 (68.9%) females, with a mean age of 17.1 ± 14.4 years, in the minimal RVIAT group. Patient distribution according to the diagnosis was 12 (46.1%) secundum ASD, nine (34.6%) sinus venosus ASD, five (19.7%) partial AVSD in the SMS group, and 10 (47.6%) secundum ASD, eight (38%) sinus venosus ASD, and three (14.3%) partial AVSD in the minimal RVIAT group.
| Variables | SMS (n = 26) | Minimal RVIAT (n = 21) | p∗ | ||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | ||||
| Age (y) | 21.2 ± 10.1 (2–34) | 17.1 ± 14.4 (3–28) | 0.81 | ||
| Female/male | 15/11 | 13/8 | |||
| Weight (kg) | 24.3 ± 12.9 | 26.1 ± 14.0 | 0.90 | ||
| Cardiothoracic rate | 0.54 ± 0.4 | 0.60 ± 0.4 | 0.4 | ||
| ASD types | |||||
| Secundum ASD | 12 (46.1) | 10 (47.6) | 0.6 | ||
| Sinus venosus ASD | 9 (34.6) | 8 (38) | 0.33 | ||
| Partial AVSD | 5 (19.2) | 3 (14.3) | 0.25 | ||
Data are presented as mean for continuous variables ±SD, median (minimum–maximum) and ratios are given as percent values.
ASD = atrial septal defect; AVSD = atrioventricular septal defect; RVIAT = right vertical infra-axillar thoracotomy; SD = standard deviation; SMS = standard median sternotomy.
∗. Independent sample is explained as t test and Chi-square test; statistical significance described as p < 0.05.
3.2. Operative data
The results obtained from the operations are given in Table 1. It is statistically significant that the time for the setup of CBP was clearly longer in the minimal RVIAT group than in the SMS group (p = 0.04). No statistical difference was observed between the two groups in terms of CBP time, aortic cross clamp time, and total operation time.
3.3. Clinical outcomes
In the postoperative period, mechanical ventilation time (p = 0.04), amount of chest drainage (p = 0.04), and need for blood transfusion (p = 0.02) were found to be less in minimal RVIAT than in SMS. The average incision length in minimal RVIAT was found to be significantly shorter than that in SMS (6.1 ± 1.1 cm vs. 15.1 ± 2.1 cm; p = 0.03; Fig. 3). Perioperative and late mortality during follow-up was not observed in both groups. Residual shunt was not observed in transthoracic echocardiography, which was done in both groups before the patients were discharged and during the follow-up period. No complication was observed in both groups during the follow-up period at the incision place. It was considered a significant cosmetic advantage that minimal RVIAT incision is short and left over in the axilla (Fig. 3). All the patients and relatives in this group were pleased with the cosmetic results. Our clinical evaluation showed that the patients with minimal RVIAT returned to normal daily activities in less time than the patients with SMS, and that difference was statistically significant (p = 0.035). Patients who underwent SMS experienced less postoperative pain compared with patients who had minimal RVIAT, but the difference was not statistically significant (p = 0.07). Hospital stay was shorter among minimal RVIAT patients, at a statistically significant level (p = 0.03). The average follow-up period was 27.6 ± 10.8 (8–49) months.
|
|
|
Figure 3. Skin incisions in the operations made with right vertical infra-axillar thoracotomy (RVIAT). |
4. Discussion
In our study, the early and midterm results of minimal RVIAT (which is a minimally invasive technique), as an alternative to median sternotomy in the closure of ASDs, were compared with those of SMS. Median sternotomy is frequently applied as an operation incision in the repair of ASDs. Along with this, negative cosmetic and psychological effects are seen especially in children, and teenage females and males. Because median sternotomy incisions are visible and are thus considered a lifelong reminder of the operation, several alternative techniques (surgical and transcatheter techniques) have been developed. Nonsurgical interventional transcatheter techniques have been used regardless of their cost because they are minimally invasive and have favorable cosmetic results.2 ; 10 Incisions done as an alternative to median sternotomy (right anterolateral thoracotomy, right posterolateral thoracotomy, right submammarian anterior approach) have been used in defect repair with similar results.5; 6; 11; 12 ; 13 Although these different incisions allow the patients to return to their normal daily activities, among prepuberty female patients, they can cause chest disorders and pectoral muscle development, as well as a decrease in sensitivity of the nipple.14 ; 15 Additionally, in the ministernotomy approach, related to femoral arterial cannulation risk of scar formation, the threat of infection and ischemia is present.16 Minimal RVIAT application in ASD repair in pediatric patients was first done in 2001 by Yang et al.8 It was reported in two articles that ASD and partial AVSD repair with this technique provided splendid cosmetic results.8 ; 9 Minimal RVIAT application is an easy technique to learn and is very similar to SMS. There are three critical technical factors in minimal RVIAT implementation. The first factor is to decide from which intercostal space to enter the thoracic cavity for a good surgical exposure. This decision can be made by examining multiple chest graphics. This intercostal spaces distance to the aorta and the vena cava inferior is crucial. If the thorax cavity is accessed from a high level, vena cava inferior cannulation becomes very difficult to control. Moreover, when access is attempted from a low level, aorta cannulation also becomes difficult to control. In our series, we used the third intercostal space in many patients who had RVIAT (18 patients; 86%); the fourth intercostal space was used in three more patients. The second factor, one of the critical phases in the operation, is aortic cannulation. The distance between the intercostal space and the aorta gets longer as the body mass index increases, which in turn creates difficulty in aortic cannulation. In our study, we observed that aortic cannulation could be more easily performed in patients under the age of 14 years. For elevation and approximation of the aorta, pericardial slings were used. The aorta was held with a vascular clamp and was pulled toward the caudal, and an aortic cannula was placed with the help of other vascular clamps. The use of long aortic cannula facilitates aortic cannulation. Aortic cannulation was easily conducted according to these details. The third technical factor involves vena cava inferior cannulation. After the first critical factor is performed, a 2-cm skin incision was made in a place where it fits the seventh intercostal space just enough so the inferior vena cava cannula could pass through. Thus, it becomes easy to work within the small thoracotomy, and a postoperation thorax drain is placed from this incision. The most important cosmetic advantage of minimal RVIAT is the short incision in the axilla. Amount of chest tube drainage (p = 0.04) and need for blood transfusion (p = 0.02) were significantly less in patients who underwent minimal RVIAT than those who had SMS. This may be attributable to sternum medullary bleeding and mediastinal tissue dissection in SMS patients. Furthermore, return to normal daily activities occurred earlier in minimal RVIAT patients (p = 0.035). Although spreading of the ribs is considered more painful than sternotomy, based on the Universal Pain Assessment Tool score, postoperative pain in Group 1 was unexpectedly lower, but not statistically different (p = 0.07).
In conclusion, our clinical experience suggests that minimal RVIAT incision can easily be used as an alternative to SMS in some patients who have ASD diagnosis, and are in the appropriate age range and have suitable anatomic features. Because RVIAT provides a better surgical exposure in young males and females whose thoracic cavity is narrow, related complications are not seen because there is no need for femoral cannulation, and the incision scar is cosmetic. After a review of the related literature, it came to our notice that the first ASD repair with minimal RVIAT in Turkey was done in our clinic. We consider that in the next few years, we can make use of minimal RVIAT in our clinic, in the surgical treatment of cardiac pathology that can be accessed from the right and left atrium (VSD, AVSD, and mitral and tricuspid valve disease).
References
- 1 R.A. Hopkins, A.A. Bert, B. Buchholz, K. Guarino, M. Meyers; Surgical patch closure of atrial septal defects; Ann Thorac Surg, 77 (2004), pp. 2144–2149
- 2 G. Butera, G. De Rosa, M. Chessa; Transcatheter closure of atrial septal defect in young children: results and follow-up; J Am Coll Cardiol, 42 (2003), pp. 241–245
- 3 W. Lou, C. Chang, S. Chen; Ministernotomy versus full sternotomy in congenital heart defects: a prospective randomized study; Ann Thorac Surg, 71 (2001), pp. 473–475
- 4 B. Daglar, G. Ipek, K. Kirali, A. Gurbuz, T. Berki, M. Balkanay; Median sternotomi için submammarian insizyonla kozmetik yaklaşım; Haydarpaşa Kardiyol ve Kardiyovaskuler Cerrahi Bülteni, 4 (1996), pp. 97–99 [In Turkish, English Abstract]
- 5 J.M. Grinda, T.A. Folliguet, P. Dervanian, L. Macé, B. Legault, J.Y. Neveux; Right anterolateral thoracotomy for repair of atrial septal defect; Ann Thorac Surg, 62 (1996), pp. 175–178
- 6 N. Yoshimura, M. Yamaguchi, Y. Oshima, S. Oka, Y. Ootaki, M. Yoshida; Repair of atrial septal defect through a right posterolateral thoracotomy: a cosmetic approach for female patients; Ann Thorac Surg, 72 (2001), pp. 2103–2105
- 7 D.J. Browne; Patent ductus arteriousus; Proc R Soc Med, 45 (1952), pp. 719–722
- 8 X. Yang, D. Wang, Q. Wu; Repair of atrial septal defect through a minimal right vertical infra-axillary thoracotomy in a beating heart; Ann Thorac Surg, 71 (2001), pp. 2053–2054
- 9 D. Yang, D. Wang, Q. Wu; Repair of partial atrioventricular septal defect through a minimal right vertical infra axillary thoracotomy; J Card Surg, 18 (2003), pp. 262–264
- 10 D. Zhong-Dong, Z.M. Hijazi, C.S. Kleinman, N.H. Silverman, K. Lamtz; Amplatzer Investigators. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults; J Am Coll Cardiol, 39 (2002), pp. 1836–1844
- 11 C.A. Dieti, A.R. Torres, G.R. Favalora; Right submammarian thoracotomy in female patients with atrial septal defects and anomalous pulmonary venous connections; J Thorac Cardiovasc Surg, 104 (1992), pp. 723–727
- 12 I.A. Nicholson, D.P. Bichell, E.A. Bacha, P.J. Del Nido; Minimal sternotomy approach for congenital heart operations; Ann Thorac Surg, 71 (2001), pp. 469–472
- 13 H.J. Van de Wal, M. Barbero-Marcial, S. Hulin, Y. Lecompte; Cardiac surgery by transxiphoid approach without sternotomy; Eur J Cardiothorac Surg, 13 (1998), pp. 551–554
- 14 L.L. Cherup, R.D. Siewers, J.W. Futrell; Breast and pectoral muscle maldevelopment after anterolateral and posterolateral thoracotomies in children; Ann Thorac Surg, 41 (1986), pp. 492–497
- 15 J.C. Fisher, R. Rudolph; Augmentation mammaplasty; J.C. Fisher, J. Guerrerosantos, M. Gleason (Eds.), Manual of Aesthetic Surgery (1st ed), Springer, New York (1985), pp. 13–23
- 16 B. Shirasawa, K. Hamano, T. Katoh, Y. Fujimura, H. Tsuboi, K. Esato; A case report of open heart surgery in an infant with MNMS caused by femoral arterial cannulation during cardiopulmonary bypass; J Jpn Assoc Thorac Surg, 44 (1996), pp. 1902–1906
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?