Summary
We report a rare case of left nutcracker syndrome and right ureteropelvic junction obstruction in a young woman who suffered flank pain and hematuria. The diagnosis was confirmed with the help of Doppler ultrasonography, retrograde pyelography, magnetic resonance angiography, and magnetic resonance urography. A surgery that involves left renal vein decompression and dismembered Anderson–Hynes pelvioplasty was performed. The patient was followed up for 23 months, and her symptoms were relieved.
Keywords
nutcracker syndrome;ureteropelvic junction obstruction
1. Introduction
Left nutcracker syndrome refers to the compression of the left renal vein (LRV) between the abdominal aorta (AO) and the superior mesenteric artery (SMA), which results in renal venous hypertension and its symptoms. Ureteropelvic junction obstruction (UPJO) is defined as a functional or anatomic obstruction to urine flow from the renal pelvis into the ureter at their anatomic junction. To our knowledge, the coexistence of left nutcracker syndrome and right UPJO has not been reported in the literature.
2. Case report
A 25-year-old woman was referred to our hospital with intermittent bilateral flank pain and macroscopic hematuria 18 months in duration. The patients family and medical histories were unremarkable. Her body mass index was 16.0 kg/m2 and her physical examination was unremarkable. Routine urinalysis showed 2+ proteinuria and 4+ hematuria. The urinary red blood cell morphological examination showed isomorphic red blood cells ranging from 52% to 73%. Urinary protein excretion was 0.48 g/d. Hemogram, seurm electrolytes, blood urea nitrogen, and creatinine were within normal range.
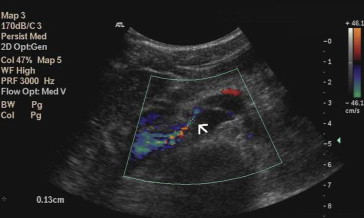
Renal Doppler ultrasound was performed, and peak velocity (PV) was measured at the hilar and aortomesenteric portions of the LRV. In the upright position, the PV in the hilar and aortomesenteric portion of the LRV were 28.4 and 200 cm/s, respectively, and the PV ratio was 7.04; the anteroposterior diameters were 11.1 mm and 1.3 mm (Fig. 1), respectively, and the ratio of the AP diameters was 8.6. The pressure gradient between LRV and inferior vena cava was 16 mmHg. It also showed dilatation of the right renal pelvis. Magnetic resonance angiography (MRA) showed that the LRV is compressed between the AO and the SMA, and the hilar portion of the LRV was distended (Fig. 2). The SMA delineated sharply from the AO, and the aortomesenteric angle where the LRV crosses was 15°. Retrograde pyelograthy (Fig. 3) and magnetic resonance urography revealed right-sided ureteropelvic junction stenosis and hydronephrosis. From these findings, a diagnosis of left nutcracker syndrome and right UPJO was made.
|
|
|
Figure 1. Doppler ultrasound showing nutcracker phenomenon. Narrowing aortomesenteric portion (arrow) of the left renal vein. |
|
|
|
Figure 2. Magnetic resonance angiography showing a compressed left renal vein between the abdominal aorta and the superior mesenteric artery. Left renal vein with distended hilar portion (arrow). |
|
|
|
Figure 3. Retrograde pyelography showing right-sided hydronephrosis and ureteropelvic junction stenosis (arrow). |
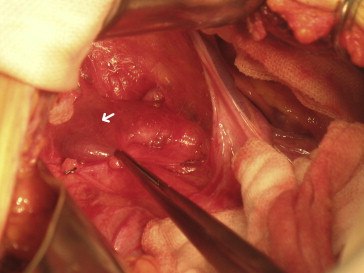
The surgery was performed under general anesthesia with median abdominal incision. During the operation, notching from the LRV (Fig. 4) and high insertion of the right ureter were seen. We dissected branches of LRV and isolated LRV. The fibrous tissue surrounding the SMA–aorta junction was excised. We also found serious dilatation of the renal pelvis and high insertion of the ureter at the right side. A dismembered Anderson–Hynes pelvioplasty was performed to correct the deformity. The patients convalescence was uneventful.
|
|
|
Figure 4. Notching from the left renal vein where compressed by the superior mesenteric artery. Compression line is marked by the white arrow. |
Two months after the operation, the symptoms disappeared. MRA revealed that the distance and the aortomesenteric angle have increased obviously, and the dilatation of the hilar portion of LRV is relieved distinctly. Doppler ultrasound documented that the right-sided hydronephrosis is ameliorated. During 23 months of follow-up, the patients body mass index did not change, and microscopic hematuria was gradually decreased.
3. Discussion
The nutcracker syndrome was originally described by El-Sadr and Mina in 1950.1 In those patients with nutcracker syndrome, the renal vein hypertension leads to the development of capsular collateral pathways around the kidney that may cause hematuria, proteinuria, and left-sided varicocele. Symptoms can also include flank and abdominal pain and pelvic congestion syndrome in females.2 Symptoms are usually aggravated by physical activities. Doppler ultrasonography is a helpful assessment for those patients suspected to have this condition. The result showed that the patients pressure gradient between the LRV and the inferior vena cava is 16 mmHg in the upright position, which indicated LRV stenosis. Pressure gradients of 3 mmHg or greater indicates LRV hypertension.3 Angiographic computed tomography, MRA, and renal angiography can delineate the anatomic relation of LRV with AO and SMA. Multidetector computed tomography can find the unusual locations of LRV compression in patients with nutcracker syndrome.4 Surgical approaches should be considered when symptoms are severe or persistent, including severe unrelenting pain, severe hematuria, renal insufficiency, and failure to respond to conservative treatment after 24 months.3 For adult patients, surgical treatment may be considered earlier with inefficacy or aggravation of conservative treatment after 6–12 months.
UPJO is a benign, congenital condition and is the most common cause of antenatal and neonatal hydronephrosis. Signs and symptoms may include flank pain, nausea and vomiting, hematuria, infection, and palpable mass.5 The etiology of UPJO appears to be multifactorial. High insertion of the ureter at the renal pelvis may result in impaired drainage in the patient, and the abnormal peristalsis at the ureteropelvic junction may simultaneously exist. Retrograde pyelography,6 magnetic resonance urography, and multidetector computed tomography5 can confirm the diagnosis. Retrograde pyelography can rule out any associated pathology of the lower ureter.6 Treatment options have been studied in depth, including open surgical procedures, endoscopic procedures, and laparoscopic procedures, and the gold standard is open pyeloplasty.7
Both nutcracker syndrome and UPJO may have anatomical etiology, and they may have the same symptoms including flank pain and hematuria. It is a rare case to encounter a patient with nutcracker syndrome and UPJO simultaneously. For our patient, we corrected two anatomical abnormalities using an open surgical procedure.
4. Ethical standards
The procedure complied with the current laws of our country.
References
- 1 A.R. El-Sadr, E. Mina; Anatomical and surgical aspects in the operative management of varicocele; Urol Cutaneous Rev, 54 (1950), pp. 257–262
- 2 U. Rudloff, R.J. Holmes, J.T. Prem, G.R. Faust, R. Moldwin, D. Siegel; Mesoaortic compression of the left renal vein (nutcracker syndrome): case reports and review of the literature; Ann Vasc Surg, 20 (2006), pp. 120–129
- 3 A.K. Kurklinsky, T.W. Rooke; Nutcracker phenomenon and nutcracker syndrome; Mayo Clin Proc, 85 (2010), pp. 552–559
- 4 D. Karaosmanoğlu, M. Karcaaltincaba, D. Akata, M. Ozmen; Unusual causes of left renal vein compression along its course: MDCT findings in patients with nutcracker and pelvic congestion syndrome; Surg Radiol Anat, 32 (2010), pp. 323–327
- 5 L.P. Lawler, T.W. Jarret, F.M. Corl, E.K. Fishman; Adult ureteropelvic junction obstruction: insights with three-dimensional multi-detector row CT; Radiographics, 25 (2005), pp. 121–134
- 6 N. Golda, A. Kappoor, J. DeMaria; Laparoscopic pyeloplasty: role of preoperative retrograde pyelography; J Pediatr Urol, 4 (2008), pp. 162–164
- 7 B. Williams, B. Tareen, M.I. Resnick; Pathophysiology and treatment of ureteropelvic junction obstruction; Curr Urol Rep, 8 (2007), pp. 111–117
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?