Highlights
- This study tested a social-identity mechanism for explaining the impacts of Australia’s plain cigarette packaging legislation.
- Reductions in brand identification were significantly associated with reduced smoking behaviours.
- Reductions in brand identification were also associated with increased quit intentions and quit attempts.
Abstract
This study tests a social identity based mechanism for the effectiveness of plain tobacco packaging legislation, introduced in Australia in December 2012, to reduce cigarette smoking. 178 Australian smokers rated their sense of identification with fellow smokers of their brand, positive brand stereotypes, quitting behaviours and intentions, and smoking intensity, both before and seven months after the policy change. Mediation analyses showed that smokers, especially those who initially identified strongly with their brand, experienced a significant decrease in their brand identity following the introduction of plain packaging and this was associated with lower smoking behaviours and increased intentions to quit. The findings provide the first quantitative evidence that brand identities may help maintain smoking behaviour, and suggest the role of social-psychological processes in the effectiveness of public health policy.
Keywords
Plain tobacco packaging;Smoking cessation;Addiction;Social identity theory;Self-categorisation theory;Social cure
Tobacco is the leading cause of preventable death globally and kills at least 5 million people each year (Jha & Peto, 2014). We might expect that selling a product that causes death on this scale would be difficult, and yet tobacco companies continue to sell their products with breathtaking success. To better understand how they do this, the introduction of plain tobacco packaging in Australia in 2012 provided an opportunity to test a novel, social identity explanation for the power of tobacco branding.
From 1 December 2012, Australia became the first country in the world to implement plain-packaging legislation, whereby all Australian tobacco products were legally required to be sold with drab-olive packaging as well as larger graphic health warning labels. The policy was implemented with the aim of encouraging smokers to quit and discouraging the uptake of smoking. While evaluations of this world-first policy are ongoing, early indications are that the reform is achieving some success. During the phase-in of the reforms, smokers exposed to plain packaging placed greater urgency on quitting compared to smokers who had not yet purchased any plain pack cigarettes (Wakefield, Hayes, Durkin, & Borland, 2013). The number of calls to a local quit helpline also increased by up to 78% and an above-average call rate was observed for approximately 10 months after the reforms were introduced (Young et al., 2014). Emerging evidence has tended to support the effectiveness of the plain-packaging legislation in increasing quit intentions and reducing smoking intensity (Durkin et al., 2015 ; Wakefield et al., 2015).
Experimental and observational simulation studies, comparing regular and mocked-up plain packaged cigarettes, provide evidence for a number of mechanisms to help explain these early impacts (for a review, see Stead et al., 2013). Specifically, plain packaging may reduce false beliefs that certain brands are less harmful and may, as a function of reduced distraction, make health warning labels more salient and so encourage established smokers to quit out of concern for their health (Brennan et al., 2015 ; Yong et al., 2015). There is also consistent evidence that plain packaging reduces pack, product and user appeal, although some researchers argue that this is only likely to deter smoking uptake (especially among youth) and weakly addicted smokers from continuing (Pechey, Spiegelhalter, & Marteau, 2013).
While these mechanisms related to cognitive processing are no doubt important, they may understate the symbolic power of brand identities and brand stereotypes in maintaining smoking behaviour. Such symbolic power has been observed in several qualitative studies of tobacco branding (Fry et al., 2008; Hoek et al., 2012 ; Scheffels, 2008). For instance, an experimental simulation study of socially disadvantaged established adult smokers found that plain packaging significantly reduced the appeal of a value-for-money cigarette brand, but made no difference to the appeal of a premium brand (Guillaumier, Bonevski, Paul, Durkin, & D'Este, 2014). The authors speculated that plain packaging may have stronger effects if the brand is personally relevant to the smoker, but could not confirm this because they did not conceptualise or measure personal relevance. Finally, tobacco industry documents show that companies develop explicit marketing strategies that seek to maintain and grow sales by creating meaningful identities through tobacco brands (Fellows & Rubin, 2006).
From a social psychological perspective, this use of cigarette branding reflects the industrys grasp of the identity processes that explain much of our consumer behaviour (Oyserman, 2009). According to the social identity approach (Tajfel and Turner, 1979 ; Turner et al., 1987) a persons self-concept is informed by their psychological group memberships (e.g., I am Australian, I am a scientist, I am a Manchester United fan). Moreover, people are likely to identify with a social category when that category reflects positively on the self. For example, a smoker who identifies as a ‘Winboro Man’ does not just regularly purchase Winboro tobacco, but also derives a positive sense of who he is by belonging to that social category.
Tobacco brand identities may now be more important than ever in maintaining smoking. In the past, the category “smoker” was viewed quite favourably (Klein, 1995). However many countries, including Australia, have since enacted ‘denormalisation’ policies (e.g. graphic anti-smoking advertisements) aimed at publicly stigmatising smokers (Chapman & Freeman, 2008). Smokers are now viewed by many as unhealthy (Kim & Shanahan, 2003), unattractive (Chapman, Wakefield, & Durkin, 2004), and even dirty (Farrimond & Joffe, 2006). One of a number of possible responses to such devaluation (Jetten, Schmitt, Branscombe, Garza, & Mewse, 2011) is for smokers to identify not (just) as a smoker, but as a smoker of a particular brand ( Hoek et al., 2012 ; Mussweiler et al., 2000). Doing so deflects the negative connotations of the superordinate category (dirty etc.) and may help to define the self with more positive content (e.g. ‘Winboro Woman’ can be sassy, independent and minty fresh).
Speaking to this point, there is some evidence that social identification as a ‘user’ of a particular substance, or with social groups where use of that substance is normative, is a barrier to recovery from addiction (Buckingham et al., 2013 ; Dingle et al., 2015a). There is also evidence that people can derive a sense of belonging and positive esteem from their social networks of substance users (Dingle, Cruwys & Frings, 2015). However, social identity processes have not been investigated in the context of cigarette brand identity or as a mechanism for the effectiveness of public health policy more generally.
Until the recent Australian policy change, branded packaging was the only avenue left to observe and enact ones brand identity, because all other tobacco advertising has been banned in Australia since 1992. Consequently, plain packaging is likely to further divest a brand of its symbolic meanings and associations (Stead et al., 2013). We would therefore predict that, following the introduction of plain packaging, smokers will identify less with their cigarette brand and will less strongly endorse positive stereotypes about their brand (Hypothesis 1). Further, if positive brand identity helps maintain smoking (Hoek et al., 2012) we would expect that reductions in brand identification will be associated with lower smoking behaviours (Hypothesis 2). These effects should be observed even after controlling for other factors thought to affect the early impacts of plain packaging in the Australian context, such as the larger and potentially more salient health warning labels and smokers' prior addiction levels.
Finally, a social identity perspective would suggest a different impact of plain packaging depending on the level of social identification with the cigarette brand. Specifically, those smokers who highly identify with their cigarette brand, who might typically be less likely to quit, may paradoxically be most affected by the implementation of plain packaging. This is because it is these smokers in particular who would be liable to lose the positive brand identity that is maintaining their smoking behaviour ( Hypothesis 3).
1. Method
1.1. Participants and design
In the three months prior to the introduction of plain packaging legislation (between 21 September and 14 November 2012), Australians over the age of 18 who smoked branded cigarettes at least daily were invited, via online discussion forums and noticeboards, to complete a 15–20 min online survey about “social factors influencing smoking” in exchange for a AUD$10 voucher. Following this Wave 1 (W1) survey, participants were sent an email invite to complete a follow-up Wave 2 (W2) survey approximately six months after the introduction of plain packaging (May 2013), in exchange for another $10 voucher. W1 participants were not eligible if they (1) did not smoke branded cigarettes daily, (2) reported having already purchased plain packaged tobacco or (3) if they quit prior to December 1, 2012. From a final eligible sample at W1 of 261 (112 females), 178 (85 females) responded to the W2 survey. Further sample details are provided in Table 1.
| Responded to W2 | N | Mean (%) | Std. deviation | p | |
|---|---|---|---|---|---|
| W1 brand identification | No | 83 | 3.69 | 1.23 | 0.37 |
| Yes | 178 | 3.55 | 1.16 | ||
| W1HSI | No | 83 | 2.07 | 1.44 | 0.32 |
| Yes | 178 | 2.27 | 1.51 | ||
| Age | No | 83 | 28.98 | 10.18 | < 0.001 |
| Yes | 178 | 34.80 | 12.90 | ||
| Index of relative socio-economic disadvantage | No | 83 | 1015.73 | 127.82 | 0.18 |
| Yes | 178 | 1035.31 | 101.68 | ||
| Gender (male) | Yes | 83 | (67.5) | < 0.01 | |
| No | 178 | (50.6) | |||
| Completed university | Yes | 83 | (28.9) | 0.26 | |
| No | 178 | (36.0) | |||
| Intend to quit in next 6 months (%) | No | 83 | (75.0) | 0.64 | |
| Yes | 178 | (72.0) |
1.2. Materials and procedure
In W1, smokers were asked to indicate which brand they smoked most often. At W2, participants who smoked at least a puff during the past week, were reminded of their previously preferred brand (automatically coded to appear in each participants individual survey) and were asked if they still smoked this brand most often. Participants who indicated that they no longer smoked this brand most often were asked to indicate which brand they now smoked most often.
1.2.1. Positive brand stereotypes
Three items drawn from research on plain packaging (Wakefield, Germain, & Durkin, 2008) were used to assess positive brand stereotypes at W1. Participants rated their level of agreement on a 1 (strongly disagree) to 7 (strongly agree) scale: “I feel that a typical smoker of (brand) is”: “trendy/stylish”; “confident/successful”; and “sophisticated” (α = 0.90).
1.2.2. Brand identification
At W1, participants rated 7 items indicating their identification with their preferred brand on a Likert scale from 1 (strongly disagree) to 7 (strongly agree). These items were programmed so that smokers' previously selected brands were automatically incorporated into questionnaire wording. Scale items were based on widely used measures of identification with a social group (Leach et al., 2008 ; Postmes et al., 2012), for example “I feel a bond with other (brand) smokers”, “I identify with the group of (brand) smokers”, (α = 0.89). At W2, all participants were asked the same questions.
1.2.3. Smoking behaviour and intentions
The Heaviness of Smoking Index (HSI; Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989) was used to provide a validated measure of nicotine dependence based on the reported time to first cigarette each day and the number of cigarettes smoked per day.
Quit intentions were assessed with a single item: ‘Are you seriously thinking of quitting smoking’ (1 = ‘yes, within the next 30 days’, 2 = ‘yes, within the next 6 months’, 3 = ‘no, not thinking of quitting’) in W1 and W2. These items were recoded to a dichotomous variable (1 = intending to quit in the next six months, 0 = not intending to quit).
At W2, participants were asked “Do you currently smoke cigarettes” with the response options: “yes, every day”, “some days (if less than 7 days per week or less than 1 cigarette per day)”, or “not at all”. Participants who responded “not at all” were asked “How many days ago did you last smoke a cigarette, even a puff?”. Participants who indicated they last smoked more than seven days ago were classified as having quit (Velicer & Prochaska, 2004). Participants were asked “SINCE DECEMBER 1 2012, how many times have you made a serious attempt to stop smoking that lasted for at least a day”. Responses to this item were recoded to a dichotomous measure of quit attempts since 1 December 2012 (0 = “no quit attempts”, and 1 = “at least one quit attempt”).
1.2.4. Exposure to plain packaging and health warning labels
In W1, participants were then asked how many, if any, plain packaged cigarettes they had purchased previously. Participants then rated the salience of health warning labels (“In the last month, how often if at all, have you noticed the warning labels on cigarette packages?”, 1 = “Never” to 5 = “Very Often”) using a validated measure of the salience of health warning labels (Borland et al., 2009). The same questions were asked at W2 after participants had completed the brand identification questions.
1.2.5. Socio-demographic covariates
Participants indicated their age, gender, education level, and suburb. Suburbs were recoded using the socio-economic index of relative disadvantage for areas (Australian Bureau of Statistics [ABS], 2014), assessing area-level characteristics including income and unemployment, to provide an indicator of socio-economic status (SES).
2. Results
Of the 378 participants who completed the W1 survey, participants were excluded who had already purchased plain packaged cigarettes at W1 (N = 90), did not smoke branded cigarettes (n = 2) or smoked cigars (N = 1), or did not provide a valid email address indicating an intent to participate in the follow up survey (N = 20). The eligible sample at the end of W1 was 265. For W2, all participants who had provided valid contact details in W1 were contacted via email. Follow up emails were sent in the second week of June 2013. In the last week of June all participants who had not responded were contacted via a third email and by telephone to ask if they wished to complete the survey. Fifty-eight participants were not contactable, two participants declined to participate in the follow up survey, seventeen participants gave a soft refusal, one participant died in December 2012, and five participants commenced but did not adequately complete the follow up survey. The study was closed on 29 June 2013. Four participants were retrospectively excluded from the eligible sample because they indicated at W2 that they had quit smoking permanently prior to December 1, 2012, yielding a final eligible sample of 261. The final analysis sample was 178 (68.2% of the eligible sample) and the average follow up time for these participants was 28 weeks.
The characteristics of the eligible W1 sample and the final analysis sample are presented in Table 1. Males and younger respondents were significantly less likely to respond to the W2 survey. There was no evidence of differential attrition with respect to W1 brand identification, W1 smoking intensity, W1 quit intentions, SES, or education. The final sample tended to be more highly educated, resided in higher SES neighbourhoods, and were more likely to intend to quit compared to the population of Australian smokers (Australian Bureau of Statistics, 2014).
Before assessing the main hypotheses, we first checked whether self-reported smoking behaviours had decreased. At W2, 100 participants (56.2%) had either quit for at least 1 week and were no longer smoking (n = 29) or had attempted to quit at least once since December 1, 2012, but had since relapsed (n = 71). Table 2 shows the results from a within subjects t-test assessing changes in the number of cigarettes smoked per day, showing that for those participants still smoking at W2, they smoked significantly fewer cigarettes per day at W2 compared to W1.
H1.
Did brand identity and positive brand stereotyping decrease?
| M W1 (SD) | M W2 (SD) | t | df | |
|---|---|---|---|---|
| Brand identification | 3.53 (1.14) | 3.23 (1.18) | − 2.68⁎⁎ | 148 |
| Positive brand stereotypes | 3.79 (1.21) | 3.39 (1.08) | − 3.38⁎⁎⁎ | 148 |
| Cigarettes per day | 14.13 (8.86) | 11.41 (9.27) | − 4.88⁎⁎⁎ | 148 |
| Salience of health warning labels | 2.86 (1.37) | 3.01 (1.26) | 1.18 | 148 |
⁎⁎. p < 0.01.
⁎⁎⁎. p < 0.001.
Table 2 shows that brand identity and positive brand stereotypes were significantly lower at W2 compared to W1. Hypothesis 1 was therefore confirmed: brand identity and positive brand stereotypes decreased after the introduction of plain packaging.
H2.
Did reductions in brand identity predict less smoking behaviour and higher quit intentions?
To assess Hypothesis 2, we first calculated a residualised brand identity decrease score (Kim-Kang & Weiss, 2008) to quantify reductions in brand identity. This is derived by regressing the W2 identity score on the W1 score, and then multiplying the residual by minus one – so that a higher score reflects a larger decrease in brand identity.
We also sought to control for the possible impacts of the increased salience of health warning labels, which is an alternative mechanism that has been proposed for the effectiveness of plain packaging. As shown in Table 1, there was no evidence that reported salience of health warning labels was significantly higher between W2 and W1. Nevertheless, to be more confident that the effects of increased salience of health warning labels were taken into account, we derived a residualised score of the increase in salience of health warning labels, using the methodology described above, for inclusion as a covariate in our multivariate analysis.
Table 3 shows the bivariate correlations between the main study variables and Table 4 shows the results of the multivariate regression models assessing whether residualised decrease in brand identity was associated with lower W2 smoking behaviours, and higher quit intentions. Our base model (model 1) controlled for the covariates age, sex, education level, and SES. Model 2a added W1 HSI, and residualised increase in health warning labels salience. Linear regression was used to assess the continuous outcome variable W2 HSI, and logistic regression analyses were run to assess the dichotomous variables of quitting, quit attempts, and quit intentions. The full sample was used to assess quitting (N = 178), and the sub-sample of participants who had not quit at W2 was used to assess the other outcome variables (N = 149).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Sex (1 = male, 0 = female) | 1.00 | |||||||||
| 2 | Age | − 0.017 | 1.00 | ||||||||
| 3 | Education (1 = university, 0 = less than university) | 0.010 | − 0.205⁎ | 1.00 | |||||||
| 4 | SES (1 = above average, 0 = below average) | − 0.042 | − 0.099 | 0.093 | 1.00 | ||||||
| 5 | W1 HSI | 0.077 | 0.458⁎⁎ | − 0.236⁎⁎ | − 0.210⁎⁎ | 1.00 | |||||
| 6 | W1 Brand Identity | 0.143 | − 0.006 | − 0.025 | 0.107 | − 0.050 | 1.00 | ||||
| 7 | Residualised decrease in brand identitya | − 0.157 | − 0.024 | − 0.038 | 0.045 | 0.012 | nac | 1.00 | |||
| 8 | Quit for at least 7 daysb | 0.101 | − 0.218⁎⁎ | − 0.087 | 0.060 | − 0.033 | − 0.063 | 0.163⁎ | 1.00 | ||
| 9 | W2 HSI | − 0.082 | 0.280⁎⁎ | − 0.142 | − 0.181⁎ | 0.746⁎⁎ | − 0.127 | − 0.138 | na | 1.00 | |
| 10 | W2 at least 1 quit attempt (no attempts = 0, attempts = 1) | 0.008 | − 0.172⁎ | 0.085 | − 0.017 | − 0.142 | − 0.025 | 0.199⁎ | na | − 0.206⁎ | 1.00 |
| 11 | W2 quit intentions (intend to quit in next 6 months = 1, no intent = 0) | − 0.072 | − 0.119 | − 0.020 | − 0.087 | 0.053 | − 0.332⁎⁎ | 0.261⁎⁎ | na | − 0.028 | 0.375⁎⁎ |
a. Decrease in brand identity, measured as: − 1 ×(residualised change in brand identity).
b. Correlations with quitting are calculated based on the full sample (N = 178), all other correlations are presented for the sample who had not quit (N = 149).
c. The association between brand identity and residualised change, is zero by definition. The latent decrease score analysis shown in Fig. 1 provides a valid method for statistically analysing the relationship between W1 brand identity and the decrease in brand identity (see McArdle, 2009 for a statistical discussion of this issue).
⁎. p < 0.05.
⁎⁎. p < 0.01.
| Outcome variable and predictor variables | Model 1a | Model 2ab | Model 2bc | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AdjOR (β) | 95% CI | N | p | AdjOR (β) | 95% CI | N | p | AdjOR (β) | 95% CI | N | p | |
| Quit at W2 | 178 | 178 | 142 | |||||||||
| Brand identity decrease | 1.67 | 1.06,2.61 | 0.024 | 1.61 | 1.02,2.54 | 0.040 | 1.91 | 1.17,3.11 | 0.01 | |||
| W1 Heaviness of Smoking Index | 1.16 | 0.81,1.65 | 0.42 | 1.04 | 0.73,1.49 | 0.83 | ||||||
| Increased warning label salience | 1.02 | 0.64,1.64 | 0.92 | 1.03 | 0.63,1.68 | 0.90 | ||||||
| W2 HSI | 149 | 149 | 113 | |||||||||
| Brand identity decrease | (− 0.10) | − 0.43,0.09 | 0.19 | (− 0.17) | − 0.45,−0.10 | < 0.01 | − 0.12 | − 0.41,−0.02 | 0.035 | |||
| W1 Heaviness of Smoking | (0.80) | 0.74,1.01 | < 0.001 | 0.82 | 0.73,1.0 | < 0.001 | ||||||
| Increased warning label salience | (− 0.025) | − 0.22,0.14 | 0.64 | − 0.05 | − 0.27,0.12 | 0.43 | ||||||
| At least 1 quit attempt | 148 | 148 | 113 | |||||||||
| Brand identity decrease | 1.44 | 1.01,2.05 | 0.044 | 1.47 | 1.03,2.11 | 0.036 | 1.35 | 0.88,2.07 | 0.16 | |||
| W1 Heaviness of Smoking Index | 0.88 | 0.68,1.15 | 0.36 | 0.95 | 0.71,1.28 | 0.74 | ||||||
| Increased warning label salience | 1.56 | 1.08,2.25 | 0.017 | 1.78 | 1.16,2.72 | < 0.01 | ||||||
| W2 intention to quit in next 6 months | 149 | 149 | 113 | |||||||||
| Brand identity decrease | 1.80 | 1.20,2.71 | < 0.01 | 1.75 | 1.16,2.63 | < 0.01 | 1.94 | 1.17,3.21 | 0.01 | |||
| W1 Heaviness of Smoking Index | 1.22 | 0.91,1.63 | 0.18 | 1.24 | 0.89,1.71 | 0.20 | ||||||
| Increased warning label salience | 1.26 | 0.86,1.85 | 0.23 | 1.46 | 0.93,2.28 | 0.10 | ||||||
a. Model 1 adjusted for gender, age, education, and socio-economic status.
b. Model 2a adjusted for Model 1 covariates in addition to W1 HSI, and residualised increase in W2 salience of health warning labels.
c. Model 2b was identical to Model 2a but excluded participants who stated they no longer regularly smoked the same brand at W2.
Residualised decrease in brand identity was associated with lower smoking behaviours. This included higher odds of quitting (AdjOR = 1.61, p = 0.04), a greater likelihood of attempting to quit even if unsuccessful (AdjOR = 1.47, p = 0.04), being more likely to intend to quit in the future (AdjOR = 1.75, p < 0.01), and lower current smoking intensity (W2 HIS; β = − 0.17, p < 0.01). These effects were found after controlling for other potential predictors, such as socio-demographic covariates, W1 HSI, and increased health warning labels salience (shown in model 2a). As a sensitivity analysis, Model 2b was run to ensure the findings were robust after excluding participants who said they no longer regularly smoked the same brand at W2. Parameter estimates were mostly similar, except for quit attempts for which the parameter estimate was somewhat smaller and no longer statistically significant (AdjOR = 1.35, p = 0.16).
These findings generally confirm Hypothesis 2: residualised decrease in brand identity predicted a higher likelihood of quitting, and, for those still smoking at W2, a higher likelihood of having attempted to quit, intending to quit in the future and smoking less intensely. These effects were maintained after controlling for W1 HSI and the perceived increases in the salience of health warning labels.
H3.
Were high brand identifiers more strongly affected by plain packaging than low identifiers?
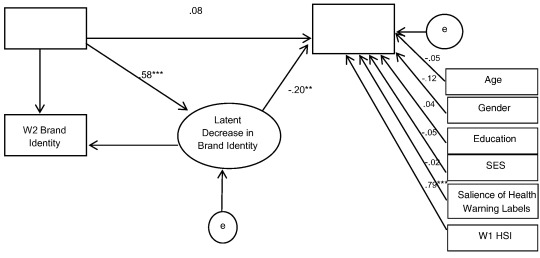
To assess Hypothesis 3, we tested the hybrid structural equation model shown in Fig. 1 (using AMOS; Arbuckle & Amos, 2006). This model tested whether W1 brand identity predicted lower W2 smoking behaviours (W2 HIS, in the case of Fig. 1) via latent brand identity decrease. Latent decrease scores are akin to residualised decrease scores and are defined as that part of W2 scores that are not contained within W1 scores. This statistical strategy was used to address a potential confound, whereby high brand identifiers may experience a greater decline in their brand identity not because of their sensitivity to plain packaging but because of regression to the mean. 1
|
|
|
Fig. 1. Hybrid structural equation model, testing mediation between brand identity and smoking behaviours (HSI). All exogeneous variables were covaried (not depicted here).1 The model depicted shows the standardised path coefficients and significance levels (*p < .05, **p < .01, ***p < .001) for the model testing the direct and indirect effects between W1 Brand ID and W2 HSI (n = 149). An otherwise identical model was tested, replacing the main DV presented here (W2 HSI), with the outcome variables: quitting smoking (N = 178), quit attempts (N = 148), and W2 quit intentions (N = 149). |
Categorical dependent variables were modelled using Markov Chain Monte Carlo estimations (Lee & Song, 2003). For the continuous variable W2 HSI, maximum likelihood estimation was used. All analyses controlled for W1 HSI, the residualised increase in perceived salience of health warning labels, and socio-demographic covariates. Table 5 shows the corresponding parameter estimates and fit statistics, indicating that our proposed model demonstrated a good fit to the data. W1 brand identity significantly predicted latent brand identity decrease in both the full sample (M = 0.62, 95% confidence interval:0.70, 0.51) and the non-quitting subsample (M = 0.58, 95% confidence interval: 0.69,0.44), such that participants who had high brand identity at W1 were most likely to experience decreases in their brand identity following the introduction of plain packaging. As shown in Table 1, this in turn predicted quit intentions and reduced smoking behaviours, such that there was a significant negative indirect effect of initial brand identification on quit intentions and smoking behaviours. The direct effect between initial brand identification and quit intentions and smoking behaviours, however, was positive, indicating a suppression effect. This is consistent with Hypothesis 3 and implies that while brand identification is typically associated with greater smoking behaviour (directly), but following the introduction of plain packaging brand identification also led to a reduction in smoking behaviour (indirectly) as these individuals were most sensitive to the new legislation due to their sense of identity derived from, and signalled by, the cigarette brand.
| Outcome variable | Standardised direct effect of W1 brand identity | 95%CI | Standardised indirect effect of W1 brand identity via latent decrease in brand identity | 95% CI | Model fit statistics | ||
|---|---|---|---|---|---|---|---|
| Quit at W2, N = 178 | − 0.204 | − 0.435 | 0.050 | 0.167 | 0.019 | 0.312 | PPP = 0.42 |
| W2 HSI, N = 149 | 0.078 | − 0.045 | 0.207 | − 0.116 | − 0.200 | − 0.048 | RMSEA < 0.01 χ2(df) = 9.42(12), p = 0.67 |
| At least one quit attempt, N = 148 | − 0.248 | − 0.460 | − 0.001 | 0.167 | 0.025 | 0.311 | PPP = 0.46 |
| Quit intentions, N = 149 | − 0.642 | − 0.847 | − 0.403 | 0.217 | 0.076 | 0.364 | PPP = 0.46 |
All SEM models controlled for age, gender, education, SES, W1HSI, and increased salience of health warning labels. PPP = posterior predictive probability (Lee & Song, 2003).
Hypothesis 3 was therefore confirmed: people with higher W1 brand identity were most likely to experience a reduction in brand identity, which in turn predicted a higher likelihood of quitting, attempting to quit, smoking less, and intending to quit in the future.
3. Discussion
These results are consistent with the proposed social identity analysis for explaining the impact of plain packaging on adult smoking behaviour. As predicted in Hypothesis 1, both brand identity and positive brand stereotypes decreased following the introduction of plain packaging, consistent with previous experimental evidence showing plain packaging reduces positive brand perceptions (Stead et al., 2013). In line with Hypothesis 2, reductions in brand identity were associated with decreased smoking behaviours, even after controlling for demographic characteristics, prior smoking intensity and perceived changes in the salience of health warning labels. Specifically, decrease in brand identity was associated with higher odds of quitting. For those still smoking at W2, decreased brand identity was associated with higher odds of: having attempted to quit since the legislative change, intending to quit smoking in the next six months, and smoking less intensely at W2. Finally, we found evidence that plain packaging is particularly likely to impact high brand identifiers (Hypothesis 3). This implies that those smokers who perceived their brand to be self-defining to begin with were more likely to be affected by plain packaging because they experience a decline in their brand identity (which was a likely maintenance factor for their smoking) compared to smokers with a weak brand identity.
These results build on qualitative research showing how smokers use brand identities as a social tool (Fry et al., 2008) for conveying status (Barnard & Forsyth, 1996), making positive associations with specific regional, gender and class identities (Scheffels, 2008), and resisting unfavourable connotations of being a smoker (Hoek et al., 2012). Our findings extend these insights by showing for the first time how brand identity, operationalised as a social identification as a smoker of a particular cigarette brand, can predict quantitative changes in self-reported smoking behaviour in the context of plain packaging. These findings support the argument that social identities can powerfully shape both the meaning and enactment of health behaviours and do so in ways that cannot be predicted by predominant health behaviour models focussing on individual and socio-demographic characteristics (see also Jetten, Haslam, & Haslam, 2012). Moreover, while social identities are often important resources for promoting health and wellbeing ( Jetten, Haslam, Haslam, Dingle, & Jones, 2014), these findings are a reminder that the social identity approach can also elaborate how identities sometimes maintain unhealthy behaviours (see also Best et al., 2016; Cruwys and Gunaseelan, 2016 ; Walter et al., 2015). This focus can assist in the development of novel ‘social cures’ that harness group processes to drive positive behavioural change.
Any causal interpretations of the current study are obviously limited by the observational design. By including W1 HSI, age, education, socio-economic status and perceived increases in the salience of health warning labels as covariates, we attempted to control for other factors that might explain our results – for example that high brand identifiers smoked less intensely to begin with, or that the more prominent health warning labels reduced both brand identification and smoking behaviours. Our mediation analysis also showed that high initial brand identification was prospectively (indirectly) associated with lower smoking behaviour. This makes it less plausible that brand identity decreases were outcomes of other attitudinal or behavioural changes, or reflected natural declines in brand identity.
A further potential limitation of the study is that smoking behaviours were self-reported. While such measures have been validated in previous research (Heatherton et al., 1989), it is likely that most smokers would have been aware of the intention of plain packaging legislation and so participants' responses may reflect a degree of expectancy bias. In light of this, future research could usefully examine how, over time, and as plain packaging becomes normalised, the sharp reductions in brand identity observed here reach a plateau. Conceivably, remaining smokers could also identify more strongly as “united smokers” rather than as smokers of a particular brand.
This study is the first to investigate social identity as a mechanism of action for a large-scale public health intervention. Given that Australia is the first testing-ground for the highly contentious legislation to require plain packaging of cigarettes (legislation that has been subject to legal challenge from multinational tobacco companies), these findings have particular relevance not just to social and health researchers, but also to policymakers. From this perspective, it is worth highlighting not only that our data support the effectiveness of plain packaging (in line with other early evidence, e.g., Durkin et al., 2015), but also that those who derived a positive identity from their cigarette brand were most sensitive to this intervention. These smokers might be harder to reach with policies targeting other mechanisms such as economic disincentives (Hughes, 2011). This suggests that attention to social identity phenomena in the context of addiction is a fruitful avenue for both conceptualising and informing public health policy.
Our results imply that, in addition to selling a product that causes death, tobacco companies also sell strong brand identities that help positively redefine what smoking means for a smokers sense of self. The introduction of plain packaging was a rare opportunity to consider this thesis: since we can barely imagine what the world would be like without brands, we can easily underestimate their influence in shaping identity, perceptions and behaviour. Plain packaging allows us to glimpse such a world, and to begin to understand the power of branding and brand identity in maintaining smoking behaviour.
References
- Arbuckle and Amos, 2006 J.L.A. Arbuckle, W.W. Amos; 7.0 Users' Guide; Amos Development Corporation, SPSS (2006)
- Australian Bureau of Statistics, 2014 Australian Bureau of Statistics; (Retrieved 22 August 2013, from) http://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa (2014)
- Barnard and Forsyth, 1996 M. Barnard, A. Forsyth; The social context of under-age smoking: A qualitative study of cigarette brand preference; Health Education Journal, 55 (2) (1996), pp. 175–184
- Barnett et al., 2005 A.G. Barnett, J.C. van der Pols, A.J. Dobson; Regression to the mean: What it is and how to deal with it; International Journal of Epidemiology, 34 (1) (2005), pp. 215–220
- Best et al., 2016 D. Best, M. Beckwith, C. Haslam, S.A. Haslam, J. Jetten, E. Mawson, D.I. Lubman; Overcoming alcohol and other drug addiction as a process of social identity transition: The Social Identity Model of Recovery (SIMOR); Addiction Research and Theory, 24 (2) (2016), pp. 111–123
- Borland et al., 2009 R. Borland, H.-H. Yong, N. Wilson, G.T. Fong, D. Hammond, K.M. Cummings, ... A. McNeill; How reactions to cigarette packet health warnings influence quitting: Findings from the ITC Four-Country survey; Addiction, 104 (4) (2009), pp. 669–675
- Brennan et al., 2015 E. Brennan, S. Durkin, K. Coomber, M. Zacher, M. Scollo, M. Wakefield; Are quitting-related cognitions and behaviours predicted by proximal responses to plain packaging with larger health warnings? Findings from a national cohort study with Australian adult smokers; Tobacco Control, 24 (Suppl. 2) (2015), pp. ii33–ii41
- Buckingham et al., 2013 S.A. Buckingham, D. Frings, I.P. Albery; Group membership and social identity in addiction recovery; Psychology of Addictive Behaviors, 27 (4) (2013), p. 1132
- Burt and Obradović, 2013 K.B. Burt, J. Obradović; The construct of psychophysiological reactivity: Statistical and psychometric issues; Developmental Review, 33 (1) (2013), pp. 29–57
- Chapman and Freeman, 2008 S. Chapman, B. Freeman; Markers of the denormalisation of smoking and the tobacco industry; Tobacco Control, 17 (1) (2008), pp. 25–31
- Chapman et al., 2004 S. Chapman, M.A. Wakefield, S.J. Durkin; Smoking status of 132,176 people advertising on a dating website. Are smokers more ‘desperate and dateless’?; Medical Journal of Australia, 181 (11–12) (2004), pp. 672–674
- Cruwys and Gunaseelan, 2016 T. Cruwys, S. Gunaseelan; “Depression is who I am”: Mental illness identity, stigma and wellbeing; Journal of Affective Disorders, 189 (2016), pp. 36–42
- Dingle et al., 2015a G.A. Dingle, C. Stark, T. Cruwys, D. Best; Breaking good: Breaking ties with social groups may be good for recovery from substance misuse; British Journal of Social Psychology, 54 (2015), pp. 236–254 https://doi.org/10.1111/bjso.12081
- Dingle et al., 2015b G.A. Dingle, T. Cruwys, D. Frings; Social identities as pathways into and out of addiction; Frontiers in Psychology, 6 (2015), p. 1795 https://doi.org/10.3389/fpsyg.2015.01795
- Durkin et al., 2015 S. Durkin, E. Brennan, K. Coomber, M. Zacher, M. Scollo, M. Wakefield; Short-term changes in quitting-related cognitions and behaviours after the implementation of plain packaging with larger health warnings: findings from a national cohort study with Australian adult smokers; Tobacco Control, 24 (Suppl. 2) (2015), pp. ii26–ii32
- Farrimond and Joffe, 2006 H.R. Farrimond, H. Joffe; Pollution, peril and poverty: A British study of the stigmatization of smokers; Journal of Community and Applied Social Psychology, 16 (6) (2006), pp. 481–491
- Fellows and L. Rubin, 2006 K.L. Fellows, D. L. Rubin; Identities for sale: How the tobacco industry construed Asians, Asian Americans, and Pacific Islanders; Journal of Intercultural Communication Research, 35 (3) (2006), pp. 265–292
- Fry et al., 2008 G. Fry, S. Grogan, B. Gough, M. Conner; Smoking in the lived world: How young people make sense of the social role cigarettes play in their lives; British Journal of Social Psychology, 47 (4) (2008), pp. 763–780
- Guillaumier et al., 2014 A. Guillaumier, B. Bonevski, C. Paul, S. Durkin, C. D'Este; Socioeconomically disadvantaged smokers' ratings of plain and branded cigarette packaging: An experimental study; BMJ Open, 4 (2) (2014), Article e004078
- Heatherton et al., 1989 T.F. Heatherton, L.T. Kozlowski, R.C. Frecker, W. Rickert, J. Robinson; Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day; British Journal of Addiction, 84 (7) (1989), pp. 791–799
- Hoek et al., 2012 J. Hoek, P. Gendall, H. Gifford, G. Pirikahu, J. McCool, G. Pene, ... G. Thomson; Tobacco branding, plain packaging, pictorial warnings, and symbolic consumption; Qualitative Health Research, 22 (5) (2012), pp. 630–639
- Hughes, 2011 J.R. Hughes; The hardening hypothesis: Is the ability to quit decreasing due to increasing nicotine dependence? A review and commentary; Drug and Alcohol Dependence, 117 (2011), pp. 111–117
- Jetten et al., 2012 J. Jetten, C. Haslam, S.A. Haslam; The social cure: Identity, health and well-being; Psychology Press, Hove (2012)
- Jetten et al., 2014 J. Jetten, C. Haslam, S.A. Haslam, G. Dingle, J.M. Jones; How groups affect our health and well-being: The path from theory to policy; Social Issues and Policy Review, 8 (1) (2014), pp. 103–130
- Jetten et al., 2011 J. Jetten, M.T. Schmitt, N.R. Branscombe, A.A. Garza, A.J. Mewse; Group commitment in the face of discrimination: The role of legitimacy appraisals; European Journal of Social Psychology, 41 (1) (2011), pp. 116–126
- Jha and Peto, 2014 P. Jha, R. Peto; Global effects of smoking, of quitting, and of taxing tobacco; New England Journal of Medicine, 370 (1) (2014), pp. 60–68
- Kim and Shanahan, 2003 S.H. Kim, J. Shanahan; Stigmatizing smokers: Public sentiment toward cigarette smoking and its relationship to smoking behaviors; Journal of Health Communication, 8 (4) (2003), pp. 343–367
- Kim-Kang and Weiss, 2008 G. Kim-Kang, D.J. Weiss; Adaptive measurement of individual change; The Journal of Psychology, 216 (1) (2008), pp. 49–58
- Klein, 1995 R. Klein; Cigarettes are sublime; Picador (1995)
- Leach et al., 2008 C.W. Leach, M. van Zomeren, S. Zebel, M.L. Vliek, S.F. Pennekamp, B. Doosje, ... R. Spears; Group-level self-definition and self-investment: A hierarchical (multicomponent) model of in-group identification; Journal of Personality and Social Psychology, 95 (1) (2008), pp. 144–165
- Lee and Song, 2003 S.-Y. Lee, X.-Y. Song; Bayesian analysis of structural equation models with dichotomous variables; Statistics in Medicine, 22 (19) (2003), pp. 3073–3088
- McArdle, 2009 J.J. McArdle; Latent variable modeling of differences and changes with longitudinal data; Annual Review of Psychology, 60 (1) (2009), pp. 577–605
- Mussweiler et al., 2000 T. Mussweiler, S. Gabriel, G.V. Bodenhausen; Shifting social identities as a strategy for deflecting threatening social comparisons; Journal of Personality and Social Psychology, 79 (3) (2000), p. 398
- Oyserman, 2009 D. Oyserman; Identity-based motivation: Implications for action-readiness, procedural-readiness, and consumer behavior; Journal of Consumer Psychology, 19 (3) (2009), pp. 250–260
- Pechey et al., 2013 R. Pechey, D. Spiegelhalter, T.M. Marteau; Impact of plain packaging of tobacco products on smoking in adults and children: An elicitation of international experts' estimates; BMC Public Health, 13 (1) (2013), p. 18
- Postmes et al., 2012 T. Postmes, S.A. Haslam, L. Jans; A single-item measure of social identification: Reliability, validity, and utility; The British Journal of Social Psychology (2012)
- Scheffels, 2008 J. Scheffels; A difference that makes a difference: Young adult smokers' accounts of cigarette brands and package design; Tobacco Control, 17 (2) (2008), pp. 118–122 https://doi.org/10.1136/tc.2007.021592
- Stead et al., 2013 M. Stead, C. Moodie, K. Angus, L. Bauld, A. McNeill, J. Thomas, ... S.L. Bryce; Is consumer response to plain/standardised tobacco packaging consistent with framework convention on tobacco control guidelines? A systematic review of quantitative studies; PLoS ONE, 8 (10) (2013), Article e75919
- Tajfel and Turner, 1979 H. Tajfel, J.C. Turner; An integrative theory of intergroup conflict; The social psychology of intergroup relations33 (1979), p. 47
- Turner et al., 1987 J.C. Turner, M.A. Hogg, P.J. Oakes, S.D. Reicher, M.S. Wetherell; Rediscovering the social group: A self-categorization theory; Basil Blackwell; US, Cambridge, MA (1987)
- Velicer and Prochaska, 2004 W.F. Velicer, J.O. Prochaska; A comparison of four self-report smoking cessation outcome measures; Addictive Behaviors, 29 (1) (2004), pp. 51–60 https://doi.org/10.1016/S0306-4603(03)00084-4
- Wakefield et al., 2015 M. Wakefield, K. Coomber, M. Zacher, S. Durkin, E. Brennan, M. Scollo; Australian adult smokers' responses to plain packaging with larger graphic health warnings 1 year after implementation: Results from a national cross-sectional tracking survey; Tobacco Control, 24 (Suppl. 2) (2015), pp. ii17–ii25
- Wakefield et al., 2008 M.A. Wakefield, D. Germain, S.J. Durkin; How does increasingly plainer cigarette packaging influence adult smokers' perceptions about brand image? An experimental study; Tobacco Control, 17 (6) (2008), pp. 416–421
- Wakefield et al., 2013 M.A. Wakefield, L. Hayes, S. Durkin, R. Borland; Introduction effects of the Australian plain packaging policy on adult smokers: A cross-sectional study; BMJ Open, 3 (7) (2013)
- Walter et al., 2015 Z.C. Walter, J. Jetten, C. Parsell, G.A. Dingle; The impact of self-categorizing as “homeless” on well-being and service use; Analyses of Social Issues and Public Policy, 15 (1) (2015), pp. 333–356
- Yong et al., 2015 H.H. Yong, R. Borland, D. Hammond, J.F. Thrasher, K.M. Cummings, G.T. Fong; Smokers' reactions to the new larger health warning labels on plain cigarette packs in Australia: Findings from the ITC Australia project; Tobacco Control (2015) https://doi.org/10.1136/tobaccocontrol-2014-051979
- Young et al., 2014 J.M. Young, I. Stacey, T.A. Dobbins, S. Dunlop, A.L. Dessaix, D.C. Currow; Association between tobacco plain packaging and Quitline calls: A population-based, interrupted time-series analysis; Medical Journal of Australia, 200 (1) (2014)
Notes
1. There is a possible confound explaining why high brand identifiers might be more likely to experience a decline in brand identity, other than their (hypothesised) greater sensitivity to the introduction of plain packaging. The problem is regression to the mean, such that extreme scores are more likely to moderate toward the sample average over time (Barnett et al., 2005 ; Burt and Obradović, 2013). Latent change scores are recommended for addressing this confound (McArdle, 2009).
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?