Summary
Objectives
This study investigated short-term outcomes of Lichtenstein hernia repair using self-gripping Parietex ProGrip mesh in Chinese patients with inguinal hernias.
Methods
Retrospective analysis of patients undergoing Lichtenstein hernia repair using the Parietex ProGrip mesh at a single hospital in China between July 2012 and June 2013. All patients completed the EuroQol-five dimensions (EuroQoL-5D) and short form-36 questionnaires and were followed up at 1 day, 7 days, 1 month. and 6 months, postoperatively.
Results
Ninety cases (66 males, 24 females) were studied. Mean ± standard deviation (SD) patient age was 48.7 ± 16.8 (range, 21–87) years. Most hernias were Gilberts type II (23%) or III (31%). During 6 months of follow-up, none of the patients had recurrent hernia or systemic postoperative complications. The mean ± SD pain visual analog scale score decreased from 32 ± 10.6 at postoperative Day 1 to 0.67 ± 2.5 at 6 months. From postoperative Day 1 to 6 months, there were marked improvements in health and health-related quality of life; mean ± SD visual analog scale EuroQoL score increased from 55.3 ± 8 to 95.2 ± 3 and mean ± SD HR EuroQoL score from 0.31 ± 0.07 to 0.95 ± 0.02. At 6 months, mean scores in all eight dimensions of the short form-36 questionnaires had increased from baseline.
Conclusion
The use of self-fixating Parietex ProGrip mesh in open inguinal hernia repair is simple, rapid, effective, and safe, and is associated with low postoperative pain and improved quality life among patients.
Keywords
inguinal hernia;mesh repair;open repair;pain;Parietex ProGrip;quality of life
1. Introduction
Surgery for inguinal hernia is one of the most common operations seen in clinical practice,1 with an estimated worldwide incidence of over 20 million each year.2 In the United Kingdom, inguinal hernias affect 0.14% of the population, accounting for around 70,000 operations per year,3 while in the United States, there are approximately 750,000 inguinal hernia repairs performed per year.4 In China, no nationwide epidemiological data are available However two regional investigations reported that the prevalence of inguinal hernia was 0.2% among 5000 participants in Tianjin in 20055 and 0.36% of 20743 participants in Shanghai 2007.6
In the past decade, the outcomes for inguinal hernia surgery have improved dramatically with the routine use of Lichtenstein open tension-free hernioplasty.7 Lichtenstein described his repair technique as “tension-free”, wherein a piece of polypropylene mesh is used to strengthen the fascia transversalis.8 As an ambulatory procedure that can be performed under local anesthesia,9 ; 10 the Lichtenstein mesh repair has remarkable benefits such as reduced cost, low recurrence rates, and a low risk of perioperative morbidity. Many surgeons have since adopted this technique, and it is now regarded as the gold standard surgical procedure for the treatment of inguinal hernias.9 ; 11 However, complications of the open technique include a longer postoperative recovery time and a higher incidence of chronic inguinal pain.12
Chronic pain can be disabling and can affect patients' quality life.13 A Swedish survey estimated that about a third of patients experienced residual pain even 2–3 years after hernia repair surgery, with about 6% reporting that the pain interfered with their daily activities.14 The major reason for post-herniorrhaphy groin pain remains unclear, but it is likely to be associated with certain aspects of the repair technique, such as the perioperative handling of the cutaneous nerves, the type of mesh, and mesh fixation.15
Heavy weight polypropylene meshes have been found to elicit inflammatory reactions responsible for mesh shrinkage when scar tissue evolves.16 Thus, it has been recommended to use low-weight meshes17 ; 18 and to limit the extent of fixation.19 More recently, self-gripping meshes have been developed, avoiding the need for additional fixation. The Parietex ProGri (Covidien, Dublin, Ireland) self-fixating mesh is composed of monofilament polyester and polylactic acid (PLA) grips, and is indicated for use in inguinal and incisional hernia repairs. Kingsnorth et al15 demonstrated that early postoperative pain and infection rates were significantly decreased with ProGrip self-gripping polyester mesh compared with the Lichtenstein repair using polypropylene mesh. Another retrospective study of 220 patients with inguinal hernia revealed that most patients (95.9%) were satisfied with their laparoscopic hernia repair using ProGrip self-gripping mesh.20
However, the benefits of Parietex ProGrip self-fixating mesh for inguinal hernia repairs among Chinese patients are still unclear. Hence, the aim of this study was to demonstrate the safety and efficacy of open hernia repair using the Parietex ProGrip mesh in 90 Chinese cases. The incidence of chronic pain, postoperative complications, and hernia recurrence were evaluated in patients at the 6-month follow-up.
2. Methods
2.1. Patients
This was a retrospective study investigating the outcomes of open hernia repair with Parietex ProGrip self-gripping mesh between July 2012 and June 2013 at Tianjin Peoples Hospital, Tianjin, China. Patients were eligible if they were men or women aged > 18 years, who had been diagnosed with unilateral inguinal hernia and were suitable for open hernia repair using Parietex ProGrip mesh. Patients were excluded from this study if they had scrotal, incarcerated, or femoral hernia; had undergone previous laparoscopic inguinal hernia repair; or required emergency procedures. The ethics committee of the Union Medicine Center in Tianjin approved the study and all patients provided written informed consent.
2.2. Self-fixating mesh
Parietex ProGrip is a self-fixating mesh that provides immediate fixation for a secure repair. The PLA microgrips enable surgeons to position and place the mesh in < 60 seconds, without the use of additional fixation.21 In this study, the procedures were performed using the new 12 cm × 8 cm Parietex ProGrip meshes (PP1208DL/DR).
2.3. Modified technique of mesh placement
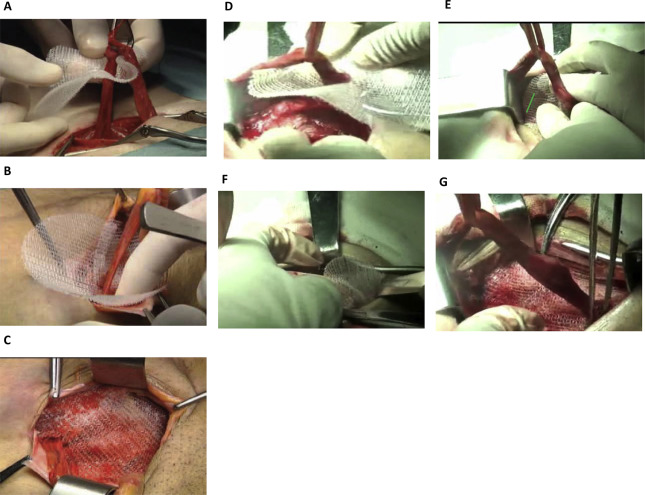
The type of anesthesia (local or spinal) was selected by the attending anesthesiologist on the basis of individual patient needs. The open inguinal hernia repair was performed on all patients by a qualified surgeon according to the Lichtenstein method,8 as described by Amid.22 Briefly, a 4–5 cm oblique incision was made and the external aponeurosis was divided. Then primary inguinal hernia repair was undertaken involving reduction of the hernia, ligation of the hernial sac, and mesh placement. All three nerves in the inguinal canal, i.e., the ilioinguinal nerve, the iliohypogastric nerve, and the genital branch of the genitofemoral nerve, were identified and preserved. The standard technique for ProGrip placement is for the surgeon to introduce a flattened ProGrip mesh into the inguinal canal anterior to the transverse fascia and posterior to the spermatic cord, covering the inguinal floor (Figure 1A–C). In this current study, however, we used a modified technique in which the ProGrip mesh was folded in half along the long axis and the apex of anterior side of the mesh was placed on the pubic tubercle with the help of forceps. The posterior side of the mesh was completely unexposed to tissue until the anterior side of the mesh had been attached to the tissue. Thereafter, the entire mesh was unrolled and affixed to the inguinal canal. The upper edge of the mesh was fixed over the conjoined tendon and the lower edge of the mesh was attached to the inguinal ligament (Figure 1D–G).
|
|
|
Figure 1. Mesh placement procedures. (A–C) Traditional mesh placement. (D–G) Modified mesh placement technique used in our patients. (A) Closing the self-gripping flap around the cord prior to lowering and positioning the mesh. (B) Working the mesh under the aponeurosis of the external oblique muscle. (C) The mesh anchors to the tissue with the micro-grips immediately and may not require any additional fixation. (D) ProGrip mesh was folded in half along the long axis, placed on the pubic tubercle (blue position line) and inguinal ligament. (E) Fix ProGrip mesh onto the pubic tubercle (blue position line) and inguinal ligament, make sure the mesh is around the deep inguinal ring. (F) Pull spermatic cord outside of the operation field, unfold ProGrip mesh. (G) Affix ProGrip mesh onto the posterior wall of inguinal canal. |
2.4. Data collection
The Gilberts classification23; 24; 25; 26 ; 27 was used to differentiate the hernias in this study. Patients were also graded according to the American Society of Anesthesiologists (ASA) criteria for assessment of comorbidities present before the surgical procedure.28 Follow-up examination was performed by a surgeon at 1 day, 7 days, 1 month, and 6 months after surgery. Outcome measures included the duration of surgery and mesh placement, postoperative hernia recurrence, and health status during follow-up. Pain was assessed using the EuroQoL visual analog scale (EQ-VAS) which includes scores from 0 to 100, where 0 represents no pain and 100 indicates the most severe pain.29 The EuroQoL–Five Dimensions (EQ-5D) questionnaire and short form-36 (SF-36) were used to assess general health. The EQ-5D consists of the EQ-5D descriptive system and the EQ-VAS. The descriptive system comprises the following five dimensions: (1) mobility; (2) self-care; (3) usual activities; (4) pain/discomfort; and (5) anxiety/depression.30 The EQ-VAS records the respondents self-rated health on a vertical, visual analogue scale where the endpoints are labeled “Best imaginable health state” and “Worst imaginable health state”.30 Health scores (EQ-VAS) ranged from 0 (worst imaginable health state) to 100 (best imaginable health state),30 while health-related quality of life (HR-EuroQoL) ranged from 0 (worst) to 1 (best).31 The EQ-5D health state may be converted to a single summary index by applying a formula that essentially attaches weights to each of the levels in each dimension (VAS Euro-QoL). The SF-36 consists of eight scaled scores, namely, physical functioning, role physical, role emotional, social functioning, mental health, vitality, bodily pain, and general health. Each scale is directly transformed into a 0–100 scale on the assumption that each question carries equal weight. The outcomes of the SF-36 were transformed from 0 (worse) to 100 (best) points based on those eight dimensions.32
3. Results
3.1. Patient characteristics
A total of 90 eligible patients, mean ± standard deviation (SD) age 48.7 ± 16.8 years, were included in the study (Table 1); 24 (27%) women and 66 (73%) men. The majority of patients with inguinal hernia were diagnosed as Gilberts type II (n = 21; 23%) and type III (n = 28; 31%). Most patients in the study group were ASA Grades 1 (47%) or Grade 2 (41%), with ASA Grade 3 accounting for 12% of all patients. No patient was classified as ASA Grade 4 or Grade 5. The mean ± SD surgical duration was 32 ± 8.15 minutes (range, 20–60 minutes) and the time taken for self-gripping mesh placement ranged from 0.5 minutes to 5 minutes (mean 1.2 ± 0.62 minutes).
| All patients (n = 90) | |
|---|---|
| Age (y) | 48.7 ± 16.8 (21–87) |
| Gender | |
| Female | 24 (27) |
| Male | 66 (73) |
| BMI (kg/m2) | 24.1 ± 3.3 (18.3–36.1) |
| Smoker | |
| Yes | 28 (31) |
| No | 62 (69) |
| Hernia location | |
| Left | 30 (33) |
| Right | 60 (67) |
| ASA score | |
| 1 | 42 (47) |
| 2 | 37 (41) |
| 3 | 11 (12) |
| 4 | 0 |
| Gilbert classification | |
| I | 11 (12) |
| II | 21 (23) |
| III | 28 (31) |
| IV | 12 (13) |
| V | 14 (16) |
| VI | 4 (5) |
| Surgical duration (min) | 32 ± 8.15 (20–60) |
| Mesh placement time (min) | 1.2 ± 0.62 (0.5–5) |
Data are presented as n (%) or mean ± SD (range).
ASA = American Society of Anesthesiologists; BMI = body mass index; SD = standard deviation.
3.2. Recurrence and complications
No anesthesia-related complications or treatment-related mortalities were reported. There was no readmission, hernia recurrence, systemic complications, or death during 6 months of follow-up.
Postoperative pain, health status, and HR-QoL at 1 day, 7 days, 1 month, and 6 months of follow-up are shown in Table 2. Notably, the mean ± SD health VAS EuroQoL score increased from 55.3 ± 8 at Day 1 to 95.2 ± 3 at the end of the follow-up period. The number of patients classified as having good health status was 30% at Day 1 and 80% at Day 7 postoperatively. The mean ± SD pain VAS score decreased from 32 ± 10.6 on Day 1 to 0.67 ± 2.5 at 6 months. Of the 90 cases, 24 (27%) patients reported no/slight postoperative pain on Day 1; this number increased to 76 (84%) on postoperative Day 7. In addition, the mean ± SD HR-QoL scores increased dramatically from 0.31 ± 0.07 at Day 1 to 0.95 ± 0.02 at the end of the follow-up period. The number of patients who complained of bad health-related quality of life (score < 0.3) dramatically declined from 34 (38%) at Day 1 to 0 at Day 7 days postsurgery. The incidence of moderate HR-QoL was 62% on Day 1 and 78% on Day 7. Overall, none of patients reported severe pain (score > 60) or low health status (score < 30) during the entire follow-up. All 90 cases achieved good quality of life with good health status and no/slight pain after 1 month of follow-up.
| All patients (n = 90) | ||||
|---|---|---|---|---|
| Day 1 | Day 7 | Month 1 | Month 6 | |
| Health (visual analog scale EuroQoL) 0–100 | ||||
| VAS EuroQoL score | 55.3 ± 8 | 67.6 ± 6.2 | 83.6 ± 5 | 95.2 ± 3 |
| No. of patients | ||||
| Bad (< 30) | 0 | 0 | 0 | 0 |
| Moderate (30–60) | 63 (70) | 18 (20) | 0 | 0 |
| Good (> 60) | 27 (30) | 72 (80) | 90 (100) | 90(100) |
| Pain (visual analog scale) 0–100 | ||||
| Pain VAS score | 32 ± 10.6 | 17.8 ± 7.3 | 4.4 ± 5.2 | 0.67 ± 2.5 |
| No. of patients | ||||
| No/slight (< 30) | 24 (27) | 76 (84) | 90 (100) | 90 (100) |
| Moderate pain (30–60) | 66 (73) | 14 (16) | 0 | 0 |
| Severe pain (> 60) | 0 | 0 | 0 | 0 |
| Health-related quality of life (HR EuroQoL) 0–1 | ||||
| HR EuroQoL Score | 0.31 ± 0.07 | 0.53 ± 0.1 | 0.74 ± 0.04 | 0.95 ± 0.02 |
| No. of patients | ||||
| Bad (< 0.3) | 34 (38) | 0 | 0 | 0 |
| Moderate (0.3–0.6) | 56 (62) | 70 (78) | 0 | 0 |
| Good (> 0.6) | 0 | 20 (22) | 90 (100) | 90 (100) |
Data are presented as n (%) or mean ± SD.
3.4. SF-36 assessment of quality life
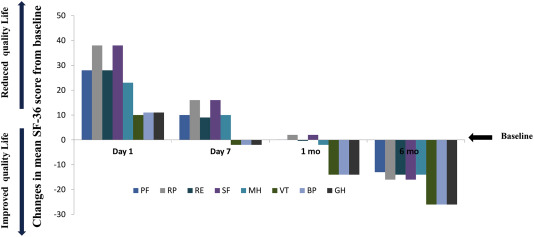
All 90 patients completed the SF-36 assessment at baseline and at 6-month follow-up (Figure 2). The postoperative SF-36 score decreased in all eight domains at Day 1. However, the SF-36 scores in five of the eight domains (role emotional, mental health, vitality, bodily pain, and general health) were higher at 1 month than at baseline. At the end of the follow-up, there were marked improvements in mean SF-36 scores over baseline for all eight dimensions.
|
|
|
Figure 2. Changes from baseline to 6-month follow-up in mean SF-36 dimension scores. BP = bodily pain; GH = general health; MH = mental health; PF = physical functioning; RP = role physical; RE = role emotional; SF = social functioning; VT = vitality. |
4. Discussion
To the best of our knowledge, this report is the first study evaluating the use of Parietex ProGrip mesh in open inguinal hernia repair using a modified method of mesh placement in a Chinese population. The results of this short-term study suggest that inguinal hernia repair with the Lichtenstein approach using self-gripping meshes is a safe and efficient procedure for Chinese patients. Similar conclusions were drawn from previous studies conducted in developed countries.15 ; 27 Furthermore, in this study, satisfactory results were achieved with regards to postoperative pain, health status, HR-QoL, and eight items of the SF-36.
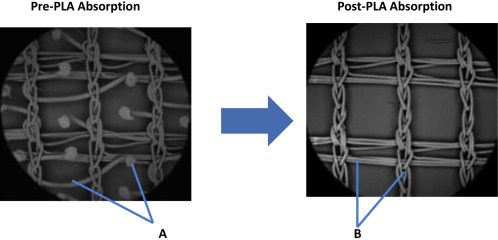
The sutureless ProGrip mesh is a revolutionary mesh as it can be secured without a suture, avoiding any risk for nerve entrapment, and preserving anatomical structures. Moreover, the resorbable PLA micro-grips of the ProGrip mesh are substantially blunt to prevent damage to the surrounding tissues. Kolbe et al33 examined the impact of ProGrip mesh on fertility in rat models and found that self-gripping mesh posed no harm to the ductus deferens. Given the larger dimensions of the human ductus deferens, there is little or no risk for a detrimental effect on fertility by application of a ProGrip mesh on exposed tissue.33
In general, the ProGrip mesh is disentangled and kept flat using two graspers during placement.20 This, however, can make operative manipulation more difficult, particularly if the size of the incision is kept to < 5 cm for aesthetic reasons. For obese patients, more than three attempts may be needed to attach the mesh in place through the incision in deep fat layers. Repeated manipulation of mesh placement may reduce the adherence of the mesh to the tissues, thus increasing the risk of mesh dislocation or migration. In the current study, the mesh was folded in half along the long axis, thereby minimizing the mesh area and making it easier to position the mesh. Importantly, this modified method may avoid mesh dislocation or migration, which may be associated with hernia recurrence and chronic pain after surgery.
The mean operation time in our analysis was 32 ± 8.15 minutes, which is comparable to times reported in other clinical trials using the laparoscopic or open approach.20; 34 ; 35 There were also no reports of hernia recurrence or postoperative complications among our cohort. The self-gripping mesh provides the advantage of obtaining fixation without using any sutures entrapping nerves in the groin. Furthermore, our modified method of mesh placement minimized the time of operative manipulation. This may have contributed to the significantly lower pain VAS scores in our study compared with those described in previous studies.35 ; 36 All patients reported no/slight pain with good health status and high HRQoL scores after 1 month follow-up. While there were decreases in the SF-36 dimension scores at 1 day and 7 days after surgery compared with baseline scores, the SF-36 values showed a remarkable improvement at 6 months follow-up (Figure 3). Scores in all eight health domains of the SF-36 were above baseline at the 6-month follow-up assessment, demonstrating the benefits of using the ProGrip mesh on postoperative health and QoL. Analogous results were published recently by Post et al.32 The retrospective nature of this study may be viewed as a limitation; however, the surgical technique was standardized, and careful postoperative follow-up was carried out to assess the hernia recurrence rate, pain, general health status, and patient quality-of-life. Further long-term follow-up studies in Chinese populations need to be undertaken.
|
|
|
Figure 3. Parietex ProGrip mesh pre- and post- polylactic acid (PLA) absorption. (A) Monofilament resorbable PLA microgrips; (B) monofilament nonresorbable polyethylene terephthalate textile. |
5. Conclusion
We report the clinical outcomes related to the self-fixating Parietex ProGrip mesh used in open inguinal hernia repair in Chinese patients. Additionally, a modified technique of mesh placement was introduced to minimize the size of the incision and facilitate operative manipulation. Our findings demonstrate that a Lichtenstein open repair using Parietex ProGrip mesh is a simple, rapid, effective, and safe method for inguinal hernia repair, and may reduce postoperative pain, improve patient general health, and quality of life.
Acknowledgments
The authors are grateful to Jiadong Xie and Huang Huang for their help in data collection and data analysis. All views and any errors are the responsibility of the authors alone. Editorial support was provided by MIMS Pte Ltd and this was funded by Covidien Ltd.
References
- 1 I.M. Rutkow; Surgical operations in the United States: then (1983) and now (1994); Arch Surg, 132 (1997), pp. 983–990
- 2 A. Kingsnorth, K. LeBlanc; Management of abdominal hernias; Edward Arnold, London, New York (2003), pp. 40–47
- 3 M.D. Rawlins, A.J. Culyer; National Institute for Clinical Excellence and its value judgments; BMJ, 329 (2004), pp. 224–227
- 4 J.D. Spitz, M.E. Arregui; Laparoscopic surgery of the abdomen. Laparoscopic totally extraperitoneal repair for inguinal hernias; Springer, New York (2004), pp. 295–302
- 5 Y. Wang, B. Yao, Z. Tian, J. Xie, X. Wang; An epidemiological study of groin hernia in the adults in Tianjin; Chin J Hernia Abdom Wall Surg, 8 (2007), pp. 13–15
- 6 X. Tang, L. Hua, D. Zhang, et al.; The multiple epidemiological study of prevalence rate on groin hernia in the adults; J Surg Concepts Practice, 7 (2002), pp. 421–422
- 7 M. Liem, T.J. van Vroonhoven; Laparoscopic inguinal hernia repair; Br J Surg, 83 (1996), pp. 1197–1204
- 8 I.L. Lichtenstenin, A.G. Shulman, P.K. Amid, M.M. Montllor; The tension-free hemioplasty; Am J Surg, 157 (1989), pp. 188–193
- 9 M. Simons, T. Aufenacker, M. Bay-Nielsen, et al.; European Hernia Society guidelines on the treatment of inguinal hernia in adult patients; Hernia, 13 (2009), pp. 343–403
- 10 P. Amid, A. Shulman, I. Lichtenstein; A critical evaluation of the Lichtenstein tension-free hernioplasty; Int Surg, 79 (1994), pp. 76–79
- 11 A. Kingsnorth, K. LeBlanc; Hernias: inguinal and incisional; Lancet, 362 (2003), pp. 1561–1571
- 12 M. Douek, G. Smith, A. Oshowo, D. Stoker, J. Wellwood; Prospective randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: five year follow up; BMJ, 326 (2003), pp. 1012–1013
- 13 Y. Fountain; The chronic pain policy coalition; Bull R Coll Surg Eng, 88 (2006), p. 279
- 14 U. Fränneby, G. Sandblom, P. Nordin, O. Nyrén, U. Gunnarsson; Risk factors for long-term pain after hernia surgery; Ann Surg, 244 (2006), pp. 212–219
- 15 A. Kingsnorth, M. Gingell-Littlejohn, S. Nienhuijs, et al.; Randomized controlled multicenter international clinical trial of self-gripping Parietex™ ProGrip™ polyester mesh versus lightweight polypropylene mesh in open inguinal hernia repair: interim results at 3 months; Hernia, 16 (2012), pp. 287–294
- 16 R. Gonzalez, K. Fugate, D. McClusky III, et al.; Relationship between tissue ingrowth and mesh contraction; World J Surg, 29 (2005), pp. 1038–1043
- 17 S. Bringman, T.-J. Heikkinen, S. Wollert, et al.; Early results of a single-blinded, randomized, controlled, Internet-based multicenter trial comparing Prolene and Vypro II mesh in Lichtenstein hernioplasty; Hernia, 8 (2004), pp. 127–134
- 18 S. Bringman, S. Wollert, J. Österberg, et al.; Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia; Br J Surg, 93 (2006), pp. 1056–1059
- 19 C. Helbling, R. Schlumpf; Sutureless Lichtenstein: first results of a prospective randomised clinical trial; Hernia, 7 (2003), pp. 80–84
- 20 D. Birk, S. Hess, C. Garcia-Pardo; Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip™ mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months; Hernia, 17 (2013), pp. 313–320
- 21 Covidien. ProGrip™ Laparoscopic Self-Fixating Mesh http://surgical.covidien.com/products/hernia-repair/progrip-laparoscopic-self-fixating-mesh.
- 22 P.K. Amid; Lichtenstein tension-free hernioplasty: its inception, evolution, and principles; Hernia, 8 (2004), pp. 1–7
- 23 I.M. Rutkow, A. Robbins; “Tension-free” inguinal herniorrhaphy: a preliminary report on the “mesh plug” technique; Surgery, 114 (1993), pp. 3–8
- 24 A. Robbins, I. Rutkow; The mesh-plug hernioplasty; Surg Clin N Am, 73 (1993), pp. 501–512
- 25 A.I. Gilbert; An anatomic and functional classification for the diagnosis and treatment of inguinal hernia; Am J Surg, 157 (1989), pp. 331–333
- 26 A.L. Gilbert; Prosthetic adjuvants to groin hernia repair: a classification of inguinal hernias; Contemp Surg, 32 (1988), pp. 28–35
- 27 T. Fasih, T. Mahapatra, R. Waddington; Early results of inguinal hernia repair by the ‘mesh plug’ technique–first 200 cases; Ann R Coll Surg Eng, 82 (2000), pp. 396–400
- 28 P. Sanjay, P. Jones, A. Woodward; Inguinal hernia repair: are ASA grades 3 and 4 patients suitable for day case hernia repair?; Hernia, 10 (2006), pp. 299–302
- 29 F. Wolfe, D. Hawley; Measurement of the quality of life in rheumatic disorders using the EuroQol; Rheumatology, 36 (1997), pp. 786–793
- 30 R. Rabin, Fd Charro; EQ-SD: a measure of health status from the EuroQol Group; Ann Med, 33 (2001), pp. 337–343
- 31 M. Poley, E. Stolk, D. Tibboel, J. Molenaar, J. Busschbach; Short term and long term health related quality of life after congenital anorectal malformations and congenital diaphragmatic hernia; Arch Dis Child, 89 (2004), pp. 836–841
- 32 S. Post, B. Weiss, M. Willer, T. Neufang, D. Lorenz; Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair; Br J Surg, 91 (2004), pp. 44–48
- 33 T. Kolbe, C. Hollinsky, I. Walter, A. Joachim, T. Rülicke; Influence of a new self-gripping hernia mesh on male fertility in a rat model; Surg Endosc, 24 (2010), pp. 455–461
- 34 J. McGreevy, P. Goodney, C. Birkmeyer, S. Finlayson, W. Laycock, J. Birkmeyer; A prospective study comparing the complication rates between laparoscopic and open ventral hernia repairs; Surg Endosc, 17 (2003), pp. 1778–1780
- 35 F. Asencio, J. Aguiló, S. Peiró, et al.; Open randomized clinical trial of laparoscopic versus open incisional hernia repair; Surg Endosc, 23 (2009), pp. 1441–1448
- 36 S. Nienhuijs, I. Van Oort, M. Keemers-Gels, L. Strobbe, C. Rosman; Randomized trial comparing the Prolene® Hernia System, mesh plug repair and Lichtenstein method for open inguinal hernia repair; Br J Surg, 92 (2005), pp. 33–38
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?