Summary
Objective
This study was conducted to identify the safety measures of performing clean urologic operations without administration of prophylaxis antibiotics.
Methods
We conducted a double-blind randomized controlled trial with patients who underwent clean urologic operations in Cipto Mangunkusumo Hospital, Jakarta, Indonesia, from April 2013 to January 2014. The local and systemic infection states were compared between the prophylaxis and placebo groups. Local infection was identified as surgical site infection and systemic infection as fever and leukocytosis.
Results
A total of 42 patients participated in the study (21 patients in each group), comprising 14 (33.3%) children and 28 (66.7%) adults. The most frequently performed operation was surgical sperm retrieval. No patients in either group were found to have local or systemic infection. However, there was a statistical difference in the white blood cell counts between the two groups (p = 0.003), although there was no sign of local or systemic infection in any of the patients.
Conclusion
Clean urologic operations without prophylaxis antibiotic therapy can be safely applied to urologic patients.
Keywords
clean urologic operation;local and systemic infection postoperation;prophylaxis antibiotics
1. Introduction
The introduction of prophylaxis antibiotics is a procedure that involves the administration of antibiotics shortly before or at the beginning of an operation or intervention procedure in order to reduce the risk of postoperative infection.1 ; 2 Postoperative infection can be localized or systemic.2 ; 3 The benefit and safety of prophylaxis antibiotics depend on the patients characteristics, type of operation, and potential morbidity after the operation. Thus, prophylaxis antibiotics are recommended if the benefits outweigh the risk involved and the costs incurred.2 ; 4
Similar to other surgical procedures, urologic operations can be categorized into four types: clean, clean-contaminated, contaminated, and dirty operations.5 Clean urologic operations are defined as operations performed in uninfected areas with no involvement of the urinary tract, and primary closure is established after the operation.1; 6 ; 7
International urology associations, such as the European Association of Urology (EAU) and the American Urological Association (AUA), are in favor of prophylaxis antibiotic therapy in those specified categories of operations.2 ; 3 In clean operations, prophylaxis antibiotic therapy is only recommended for patients with risk factors associated with immunosuppression state. Meanwhile, prophylaxis antibiotic therapy is recommended for all clean-contaminated, contaminated, and dirty operations.2; 3 ; 6 Furthermore, prophylaxis antibiotics should not be given to those undergoing clean urologic operations without prior determination of risk factors. Sterilization of the operating theater and instruments as well as adequate aseptic and antiseptic techniques are sufficient to prevent postoperative infections associated with clean urologic operations.2; 7 ; 8 The aim of this study is to evaluate the degree of safety in the case of omission of prophylaxis antibiotics in clean urologic operations. Furthermore, confirmation of the degree of safety could lead to reduction in the cost of treatment as well as prevent the microorganisms resistance to antibiotics.
2. Methods
This study was a double-blind randomized controlled trial in patients who underwent clean urologic surgery at the Urology Department, Cipto Mangunkusumo Hospital, Jakarta, Indonesia, from April 2013 to January 2014. Clean urologic operations are termed as any urologic operation with no involvement of the urinary tract, such as circumcision, hydrocelectomy, varicocelectomy, orchiectomy, orchiopexy, percutaneous sperm aspiration, testicular sperm extraction, genitalia reconstruction, vasoepididymostomy, and vasovasostomy. The inclusion criteria called for individuals who had undergone clean urologic operations, showed no sign of local infection and systemic infection prior to the operation, and who had a white blood cell count (WBC) of 5000–10,000/μL. The exclusion criteria were as follows: operation involving the urinary or digestive tract, contaminated or dirty operation site, diabetes mellitus, immunodeficiency state, and patients undergoing immunosuppressant or steroid therapy.
Participants were categorized into two groups: one group with prophylaxis antibiotic therapy (cefazolin, 1 g) and the second group with placebo (aqua); both drug forms were given intravenously 30 minutes prior to the surgery. Randomization was performed using a random number table, which had been determined before the study started. Prophylaxis antibiotics or placebo was given by an anesthesiologist without giving any information to the surgeon or to the patients as to which form of therapy had been administered. One day prior to the operation, hair at the operative site was shaved off. All patients had povidone–iodine as skin antiseptic prior to the operation.
Evaluation took place after the operation, performed by the surgeon or ward physician (for inpatients) or by the clinical physician (for patients already discharged), to ascertain whether local or systemic infection had occurred. Local infection included pus, swelling, tenderness, and wound dehiscence in the operation wound. If such signs occurred, a culture study for pathogens was conducted.5 The gauze covering the operation wound was removed, and wound care was performed on Day 7 in the urology clinic to evaluate local infection. Systemic infection evaluation included monitoring of the WBC, body temperature, and heart rate.9 Local and systemic infections were evaluated 1 day and 7 days after the operation. Patients, surgeons, ward physicians, and clinical physicians were not informed if the patients had been administered with prophylaxis antibiotics or placebo. The visual analog scale (VAS) score, a score ranging from 0 to 10—where 0 signifies no pain and 10 the most severe pain felt by patients, was also assessed 1 day and 7 days after the operation by a member of the research team.10
The data were analyzed using the software SPSS17.0 (IBM Inc., New York, United States). Descriptive and analysis studies were conducted on all participants. Descriptive study was applied to assess the patients' characteristics such as age, sex, diagnosis, type of operation, comorbidities, and local and systemic infection. The analysis study was conducted to compare the rate of local and systemic infection between the two groups. Unpaired t test was applied in variables with normal data distribution; otherwise, a nonparametric test (Mann–Whitney test) was used. The study had been approved by the Ethics Committee of the Faculty of Medicine, University of Indonesia, and informed consent was obtained from all adult participants and from the parents or legal guardians of children.
3. Results
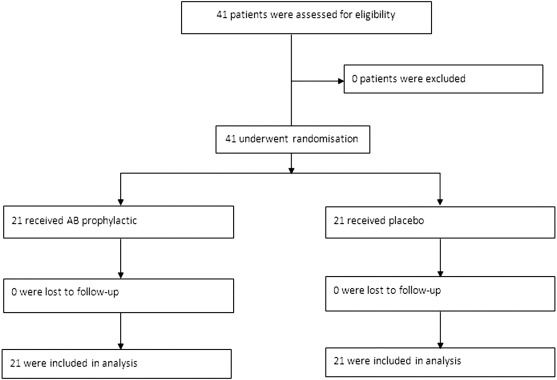
A total of 42 patients participated in this study, of which 21 patients were assigned to the prophylaxis antibiotics (AB) group and 21 patients to the placebo (P) group. The flow diagram of the randomization process of the two groups is shown in Fig. 1.
|
|
|
Figure 1. Flow diagram of the randomization process of the two groups. |
All patients were male; 14 patients (33.3%) were children and 28 patients (66.7%) were adults. The mean age of adult patients was 42.43 ± 2.36 years and that of young patients was 6.43 ± 1.51 years. The most frequent diagnosis was infertility with azoospermia in 16 patients (35.6%), treated with percutaneous sperm aspiration and testicular sperm extraction. Only one patient was diagnosed with hydrocele (2.2%), who later underwent hydrocelectomy; four patients were diagnosed with malignancy: two patients with testicular cancer (4.4%) treated with radical orchiectomy and two patients with prostate cancer (4.4%) treated with bilateral subcapsular orchiectomy. No patients were administered steroid therapy or presented an immunodeficiency state. There were no statistical differences in terms of age group (p = 0.429), diagnosis (p = 0.841), or treatment (p = 0.841). The characteristics of patients in both groups are shown in Table 1.
| Prophylaxis AB | Placebo | p | |
|---|---|---|---|
| No. of patients (%) | No. of patients (%) | ||
| Age group | |||
| Children | 6 (42.9) | 8 (57.1) | 0.429 |
| Adult | 15 (53.6) | 13 (46.4) | |
| Diagnosis | |||
| Varicocele | 6 (66.3) | 3 (33.3) | 0.841 |
| Azoospermia | 8 (50) | 8 (50) | |
| UDT | 5 (55.6%) | 4 (44.4) | |
| Testicular cancer | 1 (50) | 1 (50) | |
| Prostate cancer | 1 (50) | 1 (50) | |
| Buried penis | 0 (0) | 3 (100) | |
| Hydrocele | 0 (0) | 1 (100) | |
| Treatment | |||
| Varicocele microligation | 6 (66.7) | 3 (33.3) | 0.841 |
| PESA/TESE | 8 (50) | 8 (50) | |
| Orchidopexy | 5 (55.6) | 4 (44.4) | |
| Radical orchiectomy | 1 (50) | 1 (50) | |
| BSO | 1 (50) | 1 (50) | |
| Penis reconstruction | 0 (0) | 3 (100) | |
| Hydrocelectomy | 0 (0) | 1 (100) | |
AB = antibiotics; BSO = bilateral subcapsular orchiectomy; PESA = percutaneous sperm aspiration; TESE = testicular sperm extraction; UDT = undescended testis.
In local infection evaluation, there were no signs of surgical site infection (pus, swelling, tenderness, or wound dehiscence) in both groups. Local infection evaluations are shown in Table 2. There was no statistical difference in local infection state between the AB prophylaxis (p > 0.99) and placebo groups (p > 0.99), because all patients in both groups have no local infection in on Day 1 and Day 7.
| Parameter | Prophylaxis AB | Placebo | p |
|---|---|---|---|
| No. of patients (%) | No. of patients (%) | ||
| D-1 | |||
| Pus | 0 (0.0) | 0 (0.0) | |
| Swelling | 0 (0.0) | 0 (0.0) | |
| Tenderness | 0 (0.0) | 0 (0.0) | |
| Wound dehiscence | 0 (0.0) | 0 (0.0) | 1 |
| D-7 | |||
| Pus | 0 (0.0) | 0 (0.0) | |
| Swelling | 0 (0.0) | 0 (0.0) | |
| Tenderness | 0 (0.0) | 0 (0.0) | |
| Wound dehiscence | 0 (0.0) | 0 (0.0) | 1 |
AB = antibiotics; D-1 = 1 day after the operation; D-7 = 7 days after the operation.
In systemic infection evaluation, there was no tachycardia in any of the patients in both groups 1 day and 7 days after the operation. However, one patient from the placebo group developed a fever (T = 38°C) 1 day after the operation. There were no differences in all systemic infection parameters in both groups, except in WBC (p < 0.005). Three patients had leukocytosis—one in the prophylaxis group and two in the placebo group. All of the infections occurred 7 days after the operation. No other signs of systemic infections were observed in these patients ( Table 3).
| Parameter | Prophylactic AB (mean ± SD) | Placebo (mean ± SD) | p |
|---|---|---|---|
| WBC D-7 (/μL) | 6783.81 ± 327.10 | 8578.10 ± 475.46 | 0.003* |
| Body temperature D-1 (°C) | 36.31 ± 0.07 | 36.23 ± 0.13 | 0.40 |
| Body temperature D-7 (°C) | 36.25 ± 0.13 | 36.29 ± 0.09 | 0.80 |
| Heart rate D-1 (/min) | 80.76 ± 2.31 | 87.43 ± 1.69 | 0.02 |
| Heart rate D-7 (/min) | 82.67 ± 2.31 | 84.38 ± 2.11 | 0.58 |
| VAS D-1 | 2.24 ± 0.41 | 2.52 ± 0.19 | 0.32 |
| VAS D-7 | 0.19 ± 0.13 | 0.14 ± 0.08 | 0.73 |
AB = antibiotics; D-1 = 1 day after the operation; D-7 = 7 days after the operation; SD = standard deviation; VAS = visual analog scale; WBC = white blood cell count; ∗ = statistically significant.
4. Discussion
Nowadays, the application of prophylaxis antibiotic therapy to urology patients has to be carefully considered to determine clearly the benefits and potential risk factors. The possible benefits include avoidance of surgical site infection, which occurs in 2% of patients undergoing surgery. The possible risks are allergic reaction, development of microorganisms' resistance, and incurred costs.1; 2; 11; 12 ; 13 A recommendation for use of prophylaxis antibiotics should be based on the type of urologic operation. Furthermore, prophylaxis antibiotic therapy could be omitted in clean urologic operations, with the exception of patients with known risk factors.2; 3 ; 14
In this study, postoperation infections were categorized into two categories: local and systemic infections. All patients in both groups presented with no local infection 1 day and 7 days after the operation. Adequate aseptic and antiseptic techniques, and wound treatment, serve to prevent local infection without prophylaxis antibiotic therapy in those patients undergoing clean urologic operations.2; 14; 15 ; 16
In systemic infection monitoring, one patient from the placebo group presented with fever. The patient, who had testicular cancer, underwent radical orchiectomy. Although the patients temperature was 38°C on Day 1, he showed no other signs of local or systemic infections. His WBC was 8130/μL at the time of fever. We believe that the cause of his fever was not an infection but was possibly attributable to dehydration or systemic inflammatory response syndrome. Thus, we continued to observe the patient without giving him any antibiotics. The fever lasted for 1 day only. On Day 7, his temperature was 36.1°C, and his WBC was 9460/μL.
There were three patients (7.1%) who presented with increasing WBC (with the highest WBC of 15,930/μL in the placebo group) 7 days after the operation; however, there were no signs of local or other systemic infections in these patients. There was a significant difference in mean WBC between the two groups (p < 0.005), with a lower mean in the prophylaxis AB group. This could be due to the prophylaxis antibiotic therapy, resulting in reduced pathogen microorganisms and a lower WBC in this particular group.
Local and systemic infections often result in pain, and in those cases, the postoperative pain was also evaluated by measuring VAS. VAS was low in both groups 1 day after the operation and even lower 7 days after the operation. No patient presented with increasing VAS in either group 7 days after the operation.
Although several international surgeons are not in favor of antibiotic prophylaxis in clean urologic operations, there are still only a few studies to date, especially double-blind randomized controlled trials that compare prophylaxis antibiotics and placebo.1 ; 2 Many available studies were large-scale retrospective studies reporting on surgical site infections in clean urologic operations without antibiotic prophylaxis. A study by Yamamoto et al3 found low surgical site infection rates after 227 laparascopic and 177 open clean urologic surgeries (1.3% and 1.1%). Fahlenkamp et al17 found a low incidence rate of surgical site infections (0.8%) after 2407 clean laparoscopic urologic surgeries. Another large retrospective study was carried out by O'Connor et al,16 and also by Richardson and Nagler,18 who reported low rates of wound infection (<0.2% and 0.01%, respectively) in microsurgical varicocelectomy without prophylaxis antibiotics. A controlled trial study by Yoshida et al19 found no difference between prophylaxis antibiotics and placebo in the occurrence of surgical site infections after minimal invasive surgery to remove renal and adrenal tumors. To date, there is no study that compares the signs of systemic infection (temperature, heart rate, and WBC) and VAS between the two groups in clean urologic operations. The EAU recommendation for clean urologic operations mentioned no indication for antibiotic prophylaxis in clean urologic surgery, although there is no clear urologic evidence for this recommendation apart from the lines of evidence taken from the general surgical literature.1 The AUA recommendation was also similar to the EAU recommendation, which is to give prophylaxis antibiotics only to patients with existing risk factors who are undergoing clean urologic operations.2 In our study, those patients were excluded, hence there was no bias. The result of the study was concurrent with EAU and AUA recommendations.
This study confirms that clean urologic operations can be safely applied to urologic patients without the need for prophylaxis antibiotic therapy in our setting.
Acknowledgments
This study was supported by a grant from the Cipto Mangunkusumo Hospital, Jakarta.
References
- 1 A. Bootsma, M.P. Laguna Pes, S.E. Geerlings, A. Goossens; Antibiotic prophylaxis in urologic procedures: a systematic review; Eur Urol, 54 (2008), pp. 1270–1286
- 2 J.S. Wolf Jr., C.J. Bennett, R.R. Dmochowski, B.K. Hollenbeck, M.S. Pearle, A.J. Schaeffer; Best practice policy statement on urologic surgery antimicrobial prophylaxis; J Urol, 179 (2008), pp. 1379–1390
- 3 S. Yamamoto, H. Shima, T. Matsumoto; Controversies in perioperative management and antimicrobial prophylaxis in urologic surgery; Int J Urol, 15 (2008), pp. 467–471
- 4 J.P. Steinberg, B.I. Braun, W.C. Hellinger, et al.; Timing of antimicrobial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors; Ann Surg, 250 (2009), pp. 10–16
- 5 A.J. Mangram, T.C. Horan, M.L. Pearson, L.C. Silver, W.R. Jarvis; Guideline for prevention of surgical site infection, 1999; Infect Control Hosp Epidemiol, 27 (1999), pp. 97–134
- 6 M. Grabe; Controversies in antibiotic prophylaxis in urology; Int J Antimicrob Agents, 23 (2004), pp. 17–23
- 7 K. Shigemura, S. Arakawa, M. Yamashita, M. Yasufuku, M. Fujisawa; Surgical site infections may be reduced by shorter duration of prophylactic antibiotic medication in urological surgeries; Jpn J Infect Dis, 62 (2009), pp. 440–443
- 8 E.P. Dellinger; Prophylactic antibiotics: administration and timing before operation are more important than administration after operation; Clin Infect Dis, 44 (2007), pp. 928–930
- 9 R.M. Kleinpell, B.T. Graves, M.H. Ackerman; Incidence, pathogenesis, and management of sepsis: an overview; AACN Adv Crit Care, 17 (2006), pp. 385–393
- 10 L.J. DeLoach, M.S. Higgins, A.B. Caplan, J.L. Stiff; The visual analog scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale; Anesth Analg, 86 (1998), pp. 102–106
- 11 D.W. Bratzler, P.M. Houck, C. Richards, et al.; Use of antimicrobial prophylaxis for major surgery: baseline results from the National Surgical Infection Prevention Project; Arch Surg, 140 (2005), p. 174
- 12 D.W. Bratzler, D.R. Hunt; The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery; Clin Infect Dis, 43 (2006), pp. 322–330
- 13 W.B. Dale, M.H. Peter; Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project; Clin Infect Dis, 38 (2004), pp. 1706–1715
- 14 T. Matsumoto, H. Kiyota, M. Matsukawa, M. Yasuda, S. Arakawa, K. Monden; Japanese guidelines for prevention of perioperative infections in urological field; Int J Urol, 14 (2007), pp. 890–909
- 15 S. Takahashi, K. Takeyama, K. Hashimoto, et al.; Disinfection by antiseptics in management of postoperative surgical wounds in urologic operations; Acta Urol Jpn, 52 (2006), pp. 89–94
- 16 L.T. O'Connor Jr., M. Goldstein; Topical perioperative antibiotic prophylaxis for minor clean inguinal surgery; J Am Coll Surg, 194 (2002), pp. 407–410
- 17 D. Fahlenkamp, J. Rassweiler, P. Fornara, T. Frede, S.A. Loening; Complications of laparoscopic procedures in urology: experience with 2,407 procedures at 4 German centers; J Urol, 162 (1999), pp. 765–771
- 18 I. Richardson, H.M. Nagler; Systemic antibiotic prophylaxis not needed for microsurgical varicocelectomy; Urology, 71 (2008), pp. 669–671
- 19 S. Yoshida, H. Masuda, M. Yokoyama, T. Kobayashi, S. Kawakami, K. Kihara; Absence of prophylactic antibiotics in minimum incision endoscopic urological surgery (MEUS) of adrenal and renal tumors; Int J Urol, 14 (2007), pp. 384–387
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?