Abstract
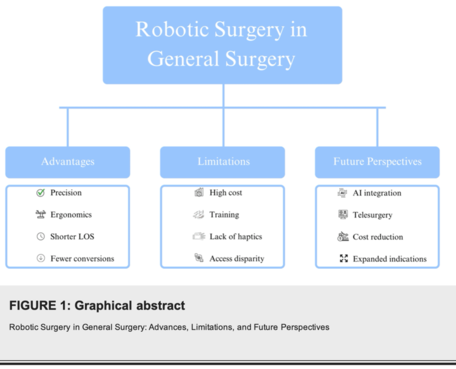
Background: Robotic surgery is an important advancement in minimally invasive surgery, providing enhanced precision, ergonomics, and visualization compared to laparoscopy. Its increasing adoption in general surgery reflects both its potential and its limitations.
Objective: To review the current role of robotic surgery in general surgery, emphasizing advances, limitations, and future perspectives.
Methods: A narrative review was performed using PubMed, Scopus, and Web of Science (2020-2023). Search terms included “robotic surgery,” “general surgery,” “da Vinci system,” and “cost-effectiveness.” Priority was given to guidelines, randomized controlled trials, systematic reviews, and meta-analyses.
Results: Robotic surgery shows advantages in ergonomics, dexterity, visualization, and conversion rates, particularly in colorectal, hernia, and hepatopancreatobiliary procedures. Limitations include high cost, limited access, absence of haptic feedback, and the need for structured training. Emerging technologies such as novel robotic platforms, artificial intelligence, and augmented reality suggest promising directions.
Conclusions: Robotic surgery improves outcomes but requires addressing cost, access, and training challenges.
Keywords: future perspectives, surgical training, cost-effectiveness, Da Vinci system, minimally invasive surgery, general surgery, robotic surgery
Introduction And Background
Robotic-assisted surgery has revolutionized the surgical landscape over the past two decades [1,2]. Initially introduced in urology and gynecology, it has now expanded into the realm of general surgery, including bariatric, colorectal, hepatopancreatobiliary, and abdominal wall reconstruction procedures. The da Vinci Surgical System, first approved by the U.S. Food and Drug Administration (FDA) in 2000, remains the most widely used platform, although newer systems are emerging [3,4].
Minimally invasive surgery (MIS) has long been the gold standard for reducing postoperative pain, blood loss, and length of hospital stay compared to open surgery [5]. However, conventional laparoscopy presents limitations, including a steep learning curve, restricted range of motion, two-dimensional imaging, and surgeon fatigue. Robotic surgery addresses many of these shortcomings by providing three-dimensional visualization, tremor filtration, enhanced ergonomics, and wristed instruments with seven degrees of freedom[6,7].
The rise of robotic surgery also reflects broader technological shifts in healthcare, where innovation is driven by artificial intelligence, big data, and virtual reality [8,9]. Robotic systems are increasingly integrated into teaching hospitals and tertiary care centers worldwide, prompting debates about equity, sustainability, and health economics [10]. For general surgeons, robotic platforms represent both an opportunity for enhanced patient care and a challenge in terms of training, accessibility, and cost-effectiveness [11].
The global market for robotic surgical systems has experienced exponential growth. Estimates suggest the robotic surgery market will surpass USD 20 billion by 2030, with an annual growth rate of approximately 15%. This expansion underscores the need for critical evaluation of the true benefits and limitations of robotic surgery in general practice [12]. Importantly, while robotic surgery demonstrates promise in select procedures, its widespreadimplementation must be supported by robust clinical evidence and careful cost- benefit analysis.
This review aims to synthesize current knowledge regarding the role of robotic surgery in general surgery, focusing on its technological advances, patient outcomes, limitations, and future perspectives.
Review
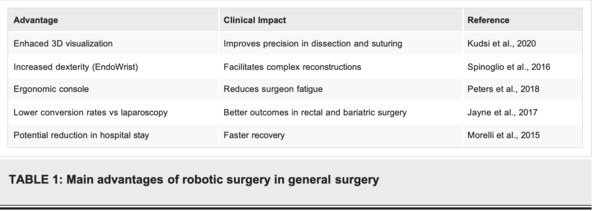
Robotic systems provide immersive three-dimensional visualization, tremor filtration, and enhanced dexterity, allowing surgeons to perform complex maneuvers in confined anatomical spaces. Ergonomic improvements also reduce musculoskeletal strain among surgeons, a common issue in prolonged laparoscopic procedures [5,7].
Multiple meta-analyses confirm that robotic colorectal surgery reduces conversion-to-open rates compared to laparoscopy, particularly in patients with narrow pelvises or obesity. Oncological outcomes, including lymph node harvest and margin status, remain comparable [6,8].
Robotic-assisted retromuscular ventral hernia repair has demonstrated reduced recurrence rates, improved mesh placement, and fewer postoperative complications [9].
Robotic Roux-en-Y gastric bypass demonstrates decreased anastomotic leak rates and improved reproducibility in complex revisional procedures. However, operative times remain longer, and cost- effectiveness is debated [10].
Robotic liver and pancreatic resections are associated with shorter learning curves, reduced blood loss, and equivalent complication rates compared with laparoscopy [11]. This technology facilitates safer dissections in anatomically challenging areas such as the hepatic hilum and pancreatic neck [12].
Overall, robotic surgery in general surgery correlates with shorter hospital stays, reduced blood loss, and faster recovery in select procedures. Patient satisfaction scores are often higher, attributed to smaller incisions and better cosmetic outcomes.
Discussion
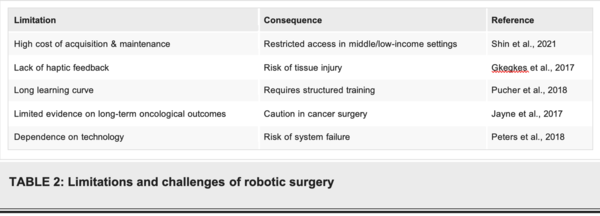
While robotic surgery represents a transformative advancement in general surgery, it is not without limitations.
High Costs: Acquisition and maintenance costs remain prohibitively high. A robotic platform may cost USD 1.5-2.5 million, with annual maintenance exceeding USD 150,000. This raises concerns about cost- effectiveness, particularly in low- and middle-income countries [10].
Learning Curve and Training: Although robotic systems may reduce the learning curve for complex procedures, standardized training curricula and certification pathways are lacking. Simulation-based training and mentorship are increasingly recognized as essential for safe adoption [11].
Lack of Haptic Feedback: Unlike traditional surgery, robotic systems lack tactile sensation, forcing surgeons to rely exclusively on visual cues for tissue handling. This limitation may increase the risk of tissue injury in inexperienced hands [13].
Accessibility and Equity: Robotic surgery is concentrated in high-resource settings, raising questions about equity and access. Global disparities in surgical care may widen unless more affordable platforms are developed [14].
Ethical and Health Policy Considerations: The introduction of robotic platforms requires careful evaluation of healthcare resource allocation. Hospitals must balance the prestige and innovation associated with robotic surgery against the obligation to provide cost-effective and equitable care. Furthermore, the marketing of robotic surgery directly to patients raises ethical concerns about informed consent and unrealistic expectations [15].
Future Perspectives
Next-generation platforms such as Senhance® and Versius® aim to reduce costs, increase portability, and enhance surgeon comfort.
Artificial Intelligence Integration: AI-driven image analysis, workflow optimization, and real-time error detection may further improve safety and efficiency [16].
Telementoring and Telesurgery: Advances in 5G connectivity may allow global surgical collaboration and remote procedures, expanding access in underserved regions [12].
Augmented Reality and 3D Modeling: Integration with preoperative imaging could allow real-time navigation and individualized surgical planning.
Integrating structured robotic curricula and proficiency-based progression [11], along with established frameworks for telementoring and telesurgery [12], expanded training pathways for general surgeons [13], ethical governance addressing consent, equity and transparency [14], steps toward supervised autonomy in defined tasks [15], and AI-enabled analytics for guidance and safety checks [16] are likely to shape the next decade of robotic generalsurgery.
Conclusions
Robotic surgery has established itself as one of the most significant technological innovations in general surgery, offering greater precision, improved ergonomics, and potential benefits in patient outcomes. Its application spans multiple subspecialties, including colorectal, hepatobiliary, hernia, and bariatric surgery, where it has demonstrated promising results in terms of reduced blood loss, shorter hospital stays, and lower conversion rates compared with traditional laparoscopy.
However, important limitations remain. The high acquisition and maintenance costs of robotic platforms restrict accessibility, particularly in low- and middle-income countries, raising concerns regarding equity in healthcare delivery. Furthermore, evidence on long-term outcomes and oncologic equivalence remains heterogeneous, requiring more randomized controlled trials and standardized reporting.
From an ethical standpoint, the introduction of robotics necessitates reconsideration of surgeon training, credentialing, and patient consent. Ensuring that surgeons are adequately trained to exploit robotic advantages while maintaining proficiency in conventional techniques is essential. Similarly, patients must be informed not only of the potential benefits but also of the limitations and current evidence gaps.
Looking ahead, ongoing technological advancements-such as artificial intelligence integration, haptic feedback, telesurgery, and reduced-cost platforms-are likely to transform the future of general surgery. These innovations may overcome current barriers and expand accessibility, democratizing robotic surgery worldwide. In this evolving landscape, multidisciplinary collaboration, evidence-based implementation, and patient-centered care willbe critical to fully harnessing the potential of robotic systems while safeguarding safety, quality, and cost-effectiveness.
Ultimately, robotic surgery should not be regarded as a replacement for traditional approaches but rather as a complementary tool that, when used appropriately, may enhance surgical care. Surgeons and institutions must strive to balance innovation with responsibility, ensuring that the adoption of robotics aligns with the overarching goal of improving patient outcomes and advancing the field of surgery.
Appendices
Document information
Published on 09/09/25
Submitted on 02/09/25
Licence: CC BY-NC-SA license