Summary
Paraganglioma is a rare extra-adrenal pheochromocytoma which originates from chromaffin cells within the ganglia of the sympathetic trunk and of the celiac, renal, suprarenal, and hypogastric plexuses. Pancreatic paragangliomas are rarer still. And even then, paragangliomas are mostly reported to be nonfunctional. We report a case of a 64-year-old woman with underlying disease of hypertension who presented with biliary colic. Contrast-enhanced computer tomography showed an enhancing mass in the uncinate process of the pancreas. Pylorus-sparing Whipple procedure was performed for complete tumor excision. Hypertensive crisis developed after Whipple, which improved after continuous intravenous nicardipine infusion. Pathology revealed a paraganglioma. A 24-h catecholamine urine test showed increased norepinephrine and vanillylmandelic acid level. Functional paraganglioma was diagnosed.
Keywords
Pancreas ; Pancreatic neoplasm ; Paraganglioma
Introduction
Paragangliomas originate from chromaffin cells within the ganglia of the sympathetic trunk and of the celiac, renal, suprarenal, and hypogastric plexuses. They occur from the skull base to the pelvis, and the most common location being the retroperitoneum. Pancreatic paragangliomas are rare and most are nonfunctional. Herein, we report a case with a functional pancreatic paraganglioma and provide a review of the features associated with the tumor.
Case Report
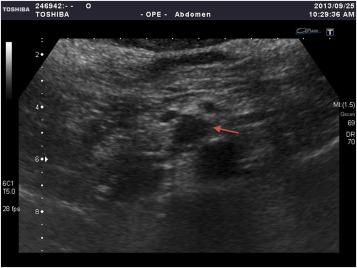
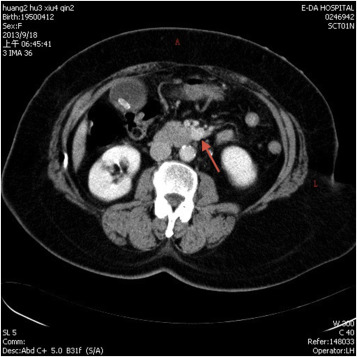
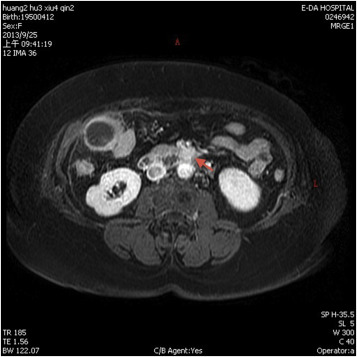
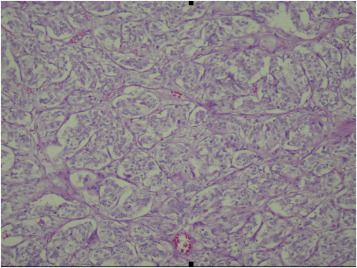
A 64-year-old woman with past medical history significant for hypertension had visited the emergency department many times over the course of several years due to intermittent hypertensive emergencies. On this presentation, she was admitted with features of symptomatic cholelithiasis. Abdominal ultrasound confirmed the presence gallstones and incidentally showed a 1.5-cm hypoechoic mass in the uncinate process of the pancreas (Figure 1 ). A physical examination was unremarkable except for mild right upper quadrant tenderness and elevated blood pressure (211/112 mmHg). Serum carcinoembryonic antigen and carbohydrate antigen 19-9 levels were both within normal limits. Contrast-enhanced computer tomography showed a 1.6-cm enhancing mass in the uncinate process of the pancreas (Figure 2 ). On magnetic resonance imaging, the lesion was identified as a 1.6-cm low-intensity mass on T1-weighted imaging and a slightly high-intensity mass on T2-weighted imaging. Magnetic resonance imaging with contrast enhancement revealed that the lesion was enhanced (Figure 3 ). On the basis of these findings, preoperative diagnosis was a pancreatic hypervascular tumor, suspected to be a neuroendocrine tumor. A pylorus-sparing Whipple procedure was recommended to achieve complete excision of the tumor and to treat the symptomatic cholelithiasis. Grossly, an oval and well encapsulated tumor measuring 1.5 cm in greatest dimension was noted within the lower part of uncinate process. Microscopically, this well-encapsulated tumor was composed of proliferation of polygonal cells arranged in trabecular, nest, and alveolar patterns separated by a stroma rich in vascular network. The tumor cells had an amphophilic-to-basophilic cytoplasm. Tumor nuclei were round to oval with moderate nuclear pleomorphism and prominent nucleoli (Figure 4 ). Mitotic figures were not identified. Capsular and vascular invasion was not present. By immunohistochemical staining, the tumor cells were reactive to CD 56, synaptophysin, and chromogranin A. The sustentacular cells surrounding the tumor clusters were also highlighted by immunostaining for S100. The lymph nodes dissected were free of malignancy. Both histomorphology and immunoprofiles of the tumor were typical of paraganglioma. Hypertensive urgency developed after the operation which was controlled with continuous intravenous nicardipine. Collected 24-h urine catecholamine data showed that norepinephrine levels were 175 μg/day (normal value: <97 μg/day) and vanillylmandelic acid levels were 8.06 mg/day (normal value: 1–7.5 mg/day). After 7-day nicardipine treatment, we gradually shifted to oral antihypertensive agents. Finally, the patient was successfully discharged with oral doxazosin (4 mg) one tablet per day. The patient had no clinical signs, symptoms, or family history suggestive of multiple endocrine neoplasia or Von Hippel–Lindau disease.
|
|
|
Figure 1. Transabdominal ultrasonogram demonstrated a hypoechoic mass (arrow) in the uncus of the pancreas. |
|
|
|
Figure 2. Axial contrast enhanced computed tomography abdomen demonstrated a 1.6-cm enhancing mass (arrow) in the uncus of the pancreas. |
|
|
|
Figure 3. Magnetic resonance imaging with contrast enhanced (T2 weighted) revealed an enhancing lesion (arrow) in the uncus of the pancreas. |
|
|
|
Figure 4. Tumor was composed of polygonal cells arranged in characteristic nested pattern “Zellballen.” Cytoplasm was amphophilic to basophilic. |
Discussion
Paragangliomas are rare extra-adrenal pheochromocytomas which originate from chromaffin cells within the ganglia of the sympathetic trunk and of the celiac, renal, suprarenal, and hypogastric plexuses. The incidence is about one in 2 million [1] . Although paragangliomas can be found within organs or soft tissues, the most common location is the infra-renal area near the origin of the inferior mesenteric artery where the organs of Zuckerkandl are located [2] . Pancreatic paragangliomas are extremely rare and only 18 cases are currently documented in English literature, including this present manuscript [3] ; [4] ; [5] . It remains unclear whether pancreatic paraganglioma represents an extension from a retroperitoneal tumor or ectopic paraganglia of visceral origin. In our case, the tumor was encapsulated within the pancreatic uncinate process. Although pancreatic paragangliomas are reported in different locations of the pancreas, the most common location is the head of the pancreas (13 of the 18 cases). Two lesions were located in the body and three lesions in the tail of the pancreas [3] ; [4] ; [5] .
Most of the extra-adrenal retroperitoneal paragangliomas are reported to be functional [6] . In contrast, most of the pancreatic paragangliomas are reported to be nonfunctional [5] . Functional paragangliomas can secrete catecholamine and usually present with hypertension, palpitation, and headache. Nonfunctional tumors may present with abdominal pain, palpable mass, or incidental image findings.
Typical imaging findings are characterized as well-defined hypervascular masses. Cystic degeneration change or hemorrhagic necrosis can be detected within larger masses [7] . Several image findings were reported to be a clue for differential diagnosis, including: (1) early enhancement of the prominent draining veins during arterial phase [7] ; and (2) absence of biliary dilation despite of large tumor size [8] . However, these findings are not specific. The differential diagnosis of pancreatic hypervascular tumors includes neuroendocrine tumors and paragangliomas. Laboratory diagnosis can be established with high urine catecholamine metabolites and metaiodobenzylguanidine scintigraphy examination. Pathological diagnosis can be obtained by endoscopic ultrasound/fine needle aspiration sampling or surgical resection. Without proper preoperative evaluation, tissue proof by endoscopic ultrasound/fine needle aspiration or resection is reported to be associated with higher risk, including hypertensive crisis [9] . Therefore, in cases where patients have with histories of pancreatic hypervascular tumors and malignant hypertension, functional paraganglioma should be taken into consideration. Proper laboratory examination should be done before tissue sampling.
Although most paragangliomas grow slowly and follow a benign course, the possibility of malignant transformation makes surgical resection the treatment of choice. Malignancy is unpredictable, and the only criterion for the diagnosis of malignancy is distant metastasis at the site where paraganglionic tissues do not exist [3] . Octreotide is reported to be able to control tumor size and ameliorate symptoms of catecholamine excess in unresectable cases [10] .
In summary, we report an extremely rare case of functional pancreatic paraganglioma. Despite its rarity, paraganglioma should be a part of the differential diagnosis of pancreatic hypervascular tumor. Proper laboratory examination of catecholamine excess should be performed before obtaining tissue samples, especially for patients with a history of malignant hypertension.
Conflicts of interest
All authors declare no conflicts of interest.
References
- [1] S.R. Malthouse, L. Robinson, S.C. Rankin; Ultrasonic and computed tomographic appearances of paraganglioma simulating pancreatic mass; Clin Radiol, 45 (1992), pp. 271–272
- [2] A. Tsukada, Y. Ishizaki, B. Nobukawa, S. Kawasaki; Paraganglioma of the pancreas: a case report and review of the literature; Pancreas, 36 (2008), pp. 214–216
- [3] N. Lightfoot, P. Santos, M. Nikfarjam; Paraganglioma mimicking a pancreatic neoplasm; JOP, 12 (2011), pp. 259–261
- [4] J. He, F. Zhao, H. Li, K. Zhou, B. Zhu; Pancreatic paraganglioma: a case report of CT manifestations and literature review; Quant Imaging Med Surg, 1 (2011), pp. 41–43
- [5] M. Borgohain, G. Gogoi, D. Das, M. Biswas; Pancreatic paraganglioma: an extremely rare entity and crucial role of immunohistochemistry for diagnosis; Indian J Endocr Metab, 17 (2013), pp. 917–919
- [6] W.S. Hayes, A.J. Davidson, P.M. Grimley, D.S. Hartman; Extra-adrenal retroperitoneal paraganglioma: clinical, pathologic, and CT findings; AJR Am J Roentgenol, 155 (1990), pp. 1247–1250
- [7] S.Y. Kim, J.H. Byun, G. Choi, E. Yu, E.K. Choi, S.H. Park, et al.; A case of primary paraganglioma that arose in the pancreas: the color Doppler ultrasonography and dynamic CT features; Korean J Radiol, 9 (Suppl.) (2008), pp. S18–S21
- [8] V.S. Parithivel, M. Niazi, A.K. Malhotra, K. Swaminathan, A. Kaul, A.K. Shah; Paraganglioma of the pancreas: literature review and case report; Dig Dis Sci, 45 (2000), pp. 438–441
- [9] M.K. Akdamar, I. Eltoum, M.A. Eloubeidi; Retroperitoneal paraganglioma: EUS appearance and risk associated with EUS-guided FNA; Gastrointest Endosc, 60 (2004), pp. 1018–1021
- [10] V. Tonyukuk, R. Emral, S. Temizkan, A. Sertcelik, I. Erden, D. Corapcioglu; Case report: patient with multiple paragangliomas treated with long acting somatostatin analogue; Endocr J, 50 (2003), pp. 507–513
Document information
Published on 15/05/17
Submitted on 15/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?